With the introduction of antibiotics into medical practice, clinically-relevant bacteria have had to adopt resistance mechanisms as part of their survival strategy. Antibiotic resistance occurs when antibiotics no longer work against disease-causing bacteria. These infections are difficult to treat and can mean longer-lasting illnesses, more doctor visits or extended hospital stays, and the need for more expensive and toxic medications. Some resistant infections can even cause death. Developing new antibiotics and other treatments to keep pace with antibiotic-resistant strains of bacteria is necessary. However, using antibiotics wisely is equally important for preventing the spread of resistant strains.
Antibiotic misuse has contributed largely to the emergence of new resistant strains. It is caused by taking an antibiotic too often for a condition it cannot treat such as viral infections and the common cold or in the wrong doses. It can also be manifested by not finishing a course of antibiotics as prescribed (stopping the antibiotic before the infection is fully cleared from the body). Overuse of antibiotics affects the body's normal flora and disrupts the balance between beneficial bacteria that help digestion for example, and harmful bacteria. Excessive use of antibiotics in intensive farming units, particularly pig and poultry farms, is also seen as a growing threat. Scientists say antimicrobial resistance may be passing between animals and humans through food consumption, making the need to cut unnecessary use of antibiotics in farming even more urgent. Responsible antibiotic use in industry, and good practice for patients and physicians, are essential to keep resistant bacterial strains curable, and antibiotic treatment affordable to patients.
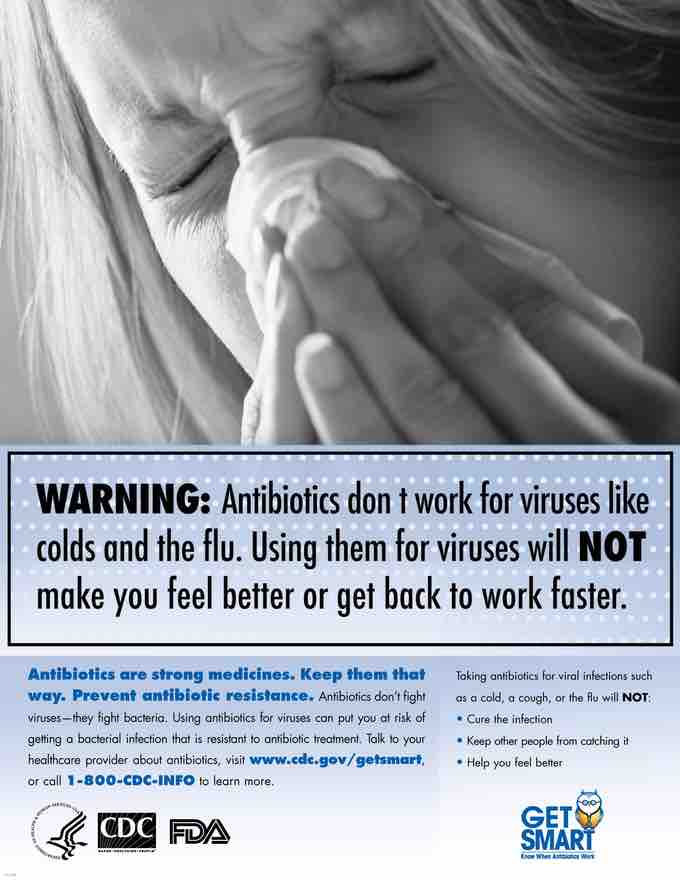
Antibiotic misuse
Antibiotics are not effective against viral infections. Misusing them leads to resistant bacterial strains.