Posttraumatic stress disorder (PTSD) develops after exposure to an event that is so stressful for an individual that it becomes traumatic. Historically (DSM-IV) categorized as an anxiety disorder, it is now categorized under "Trauma- and Stressor-Related Disorders" in the DSM 5.
The traumatic event may involve the threat of death to oneself or to someone else, or to one's own or someone else's physical, sexual, or psychological integrity, overwhelming the individual's ability to cope. As an effect of psychological trauma, PTSD is less frequent and more enduring than the more commonly seen acute stress response. Diagnostic symptoms for PTSD include re-experiencing the original trauma through flashbacks or nightmares, avoidance of stimuli associated with the trauma, and increased arousal, such as difficulty falling or staying asleep, anger, and hypervigilance. Additionally, PTSD and other posttraumatic disturbances in parental psychological functioning can, despite the best efforts of traumatized parents, interfere with their response to their child as well as their child's response to trauma.
PTSD is believed to be caused by experiencing any of a wide range of events which produces intense negative feelings of "fear, helplessness, or horror" in the observer or participant. Sources of such feelings may include (but are not limited to):
- Experiencing or witnessing childhood or adult physical, emotional, or sexual abuse
- Experiencing or witnessing physical assault, adult experiences of sexual assault, accidents, drug addiction, illnesses, and medical complications
- Employment in occupations exposed to war (such as soldiers) or disaster (such as emergency service workers)
- Getting a diagnosis of a life-threatening illness
Causes
Evolutionary psychology views different types of fears and reactions to fears as adaptations that may have been useful in the ancestral environment in order to avoid or cope with various threats. Mammals generally display several defensive behaviors roughly dependent on how close the threat is: avoidance, vigilant immobility, withdrawal, aggressive defense, appeasement, and finally complete, frozen immobility (the last possibly to confuse a predator's attack reflex or to simulate a dead and contaminated body). PTSD may correspond to and be caused by overactivation of such fear circuits. Thus, PTSD avoidance behaviors may correspond to mammal avoidance of and withdrawal from threats.
PTSD symptoms may result when a traumatic event causes an over-reactive adrenaline response, which creates deep neurological patterns in the brain. PTSD causes biochemical changes in the brain and body that differ from other psychiatric disorders such as major depression. Most people with PTSD also show a low secretion of cortisol and high secretion of catecholamines in urine, with a norepinephrine to cortisol ratio consequently higher than comparable non-diagnosed individuals. These findings suggest abnormality in the hypothalamic-pituitary-adrenal (HPA) axis.
Although most people (50–90%) encounter trauma over a lifetime, only about 8% develop full PTSD. Vulnerability to PTSD presumably stems from an interaction of biological diathesis, early childhood developmental experiences, and trauma severity. Predictor models have consistently found that childhood trauma, chronic adversity, and familial stressors increase risk for PTSD as well as biological markers of risk for PTSD after a traumatic event in adulthood. This effect of childhood trauma, which is not well-understood, may be a marker for both traumatic experiences and attachment problems.
Treatments
Modest benefits have been seen from early access to cognitive behavioral therapy, as well as from some medications such as propranolol. Critical incident stress management has been suggested as a means of preventing PTSD, but subsequent studies suggest the likelihood of its producing iatrogenic outcomes. A review of multiple studies, involving a number of different post-event psychological interventions structured to prevent PTSD "...did not find any evidence to support the use of an intervention offered to everyone", and that "...multiple session interventions may result in a worse outcome than no intervention for some individuals."
Cognitive behavioral therapy (CBT) seeks to change the way a trauma victim feels and acts by changing the patterns of thinking or behavior, or both, responsible for negative emotions. CBT have been proven to be an effective treatment for PTSD and is currently considered the standard of care for PTSD by the United States Department of Defense. In CBT, individuals learn to identify thoughts that make them feel afraid or upset and replace them with less distressing thoughts.
Eye movement desensitization and reprocessing (EMDR) is specifically targeted as a treatment for PTSD. Based on the evidence of controlled research, the American Psychiatric Association and the United States Department of Veterans Affairs and Department of Defense have placed EMDR in the highest category of effectiveness and research support in the treatment of trauma.
SSRIs (selective serotonin reuptake inhibitors) are considered to be a first-line drug treatment. SSRIs for which there are data to support use include: citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline. Among the anti-depressants described in this section, bupropion and venlafaxine have the lowest patient drop-out rates. Sertraline, fluoxetine, and nefazodone have a modestly higher drop-out rate (~15%), and the heterocyclics and paroxetine have the highest rates (~20%+).
The hypothalmic-pituitary-adrenal axis.
The HPA axis is a major biological mechanism of stress and stress response
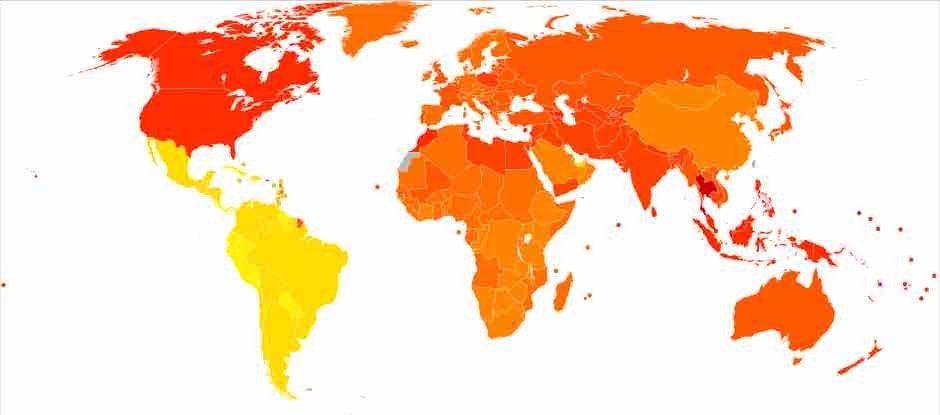
Post-traumatic stress disorder worldwide.
Incidences of PTSD by country (per 100,000 persons). The redder the country, the higher the incidence of PTSD.