States Monitoring Assisted Reproductive Technology Collaborative
What Is the SMART Collaborative?
States Monitoring Assisted Reproductive Technology (SMART) is a collaborative project between CDC’s Division of Reproductive Health (DRH) and the Connecticut Department of Health, the Florida Department of Health, the Massachusetts Department of Public Health, and the Michigan Department of Community Health.
The purpose of SMART is to establish, evaluate, improve, and promote state-based surveillance of Assisted Reproductive Technology (ART), infertility, and related activities. This surveillance can be used to monitor and study maternal and infant health outcomes related to ART. Learn more about SMART state projects.
History of SMART
 In 2001, the CDC’s Division of Reproductive Health initiated a project linking Assisted Reproductive Technology surveillance data for infants born in 1997 and 1998 to Massachusetts resident women who attended ART clinics in Massachusetts and Rhode Island with data obtained from the state of Massachusetts birth and death certificate files. The main objectives were to (1) create a population-based dataset of ART mother-infant pairs with information on both conception and delivery, and (2) compare this with similar data from other mother-infant pairs in the population.
In 2001, the CDC’s Division of Reproductive Health initiated a project linking Assisted Reproductive Technology surveillance data for infants born in 1997 and 1998 to Massachusetts resident women who attended ART clinics in Massachusetts and Rhode Island with data obtained from the state of Massachusetts birth and death certificate files. The main objectives were to (1) create a population-based dataset of ART mother-infant pairs with information on both conception and delivery, and (2) compare this with similar data from other mother-infant pairs in the population.
The project results indicated that the linkage of ART data with existing vital statistics data and health care information systems is feasible, and provided data for a systematic assessment of certain adverse outcomes that otherwise could not be accomplished. In 2008, the linkage process was expanded to include additional information (e.g., hospital discharge data, birth defect registries, cancer registries) and other states (Florida and Michigan) to develop surveillance data on maternal and infant health outcomes after ART. Initially, data from the National Assisted Surveillance System (NASS) linked with vital records files from three states: Florida, Massachusetts, and Michigan. In 2013, Connecticut joined the collaborative and data from their vital records are also linked with NASS. These projects have been jointly established under a consortium called the States Monitoring Assisted Reproductive Technology (SMART) Collaborative.
What Are SMART Core Functions?
The core functions of the SMART Collaborative are as follows:
- Develop and implement state-based ART surveillance systems.
- Share ART, infertility, and related surveillance science and practice.
- Support collaborative activities between states, CDC, and other organizations to develop science and practice for ART, infertility, and related public health surveillance.
The vision of this collaborative is to
- Support the development of a surveillance system for ART maternal and infant health outcomes.
- Strengthen our capacity for evaluating these outcomes.
- Provide information to improve maternal and perinatal outcomes and programs in all three states.
The SMART Collaborative further envisions establishing a network of 5–10 states where ART use is common and vital statistics records allow linkages to the NASS dataset. Such a network would be an important step to developing a national surveillance system of ART maternal and infant health outcomes.
SMART Linkage Methodology
 The SMART Collaborative aims to link information from ART surveillance with state birth records, infant and fetal death records, and other surveillance systems and registries.The linked data set creates a population-based data registry of ART and non-ART births that can be used to monitor and examine ART pregnancy outcomes. This allows comparison of infants conceived using ART and their mothers to the general birth population.
The SMART Collaborative aims to link information from ART surveillance with state birth records, infant and fetal death records, and other surveillance systems and registries.The linked data set creates a population-based data registry of ART and non-ART births that can be used to monitor and examine ART pregnancy outcomes. This allows comparison of infants conceived using ART and their mothers to the general birth population.
Because direct identifiers are not available in NASS, the linkage methodology uses a probabilistic linkage method, Link Plus software, developed by CDC’s Division of Cancer Prevention and Control, using the following indirect linking variables:
- Mother’s date of birth.
- Infant’s date of birth.
- Plurality.
- Gravidity.
- Zip code.
Rates of Linkage Between Assisted Reproductive Technology Surveillance System Data and Vital Records, by State, October 2014.
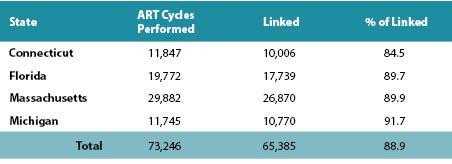
P-value=0.60 based on χ2 [test] for comparison of linkage rates among three states (no difference between linkage rates among three states).
As of October 2014, ART data have been linked to vital records file in Florida (1998—2010), Massachusetts (1997—2010), and Michigan (1996—2009), yielding an average linkage rate of 90%.
How Is Data Confidentiality Protected?
ART surveillance data and linked data files are protected under 308(d) Assurance of Confidentiality. Because of this Assurance, all data files are considered confidential materials and are safeguarded to the greatest extent possible. This Assurance extends to all ART-state linked data.
SMART Collaborative Research
The SMART data set is used for both research and surveillance. The main research questions being addressed pertain to three categories:
- The validity and agreement of information collected through different mechanisms. For example, if the birth certificate data includes data on the use of ART or other infertility treatments, the linked data will allow validating the birth certificate information against the information collected through the ART surveillance system. Similarly, maternal and child health outcomes may be available through the birth certificate and validated through information reported through the hospital discharge summaries.
- The association of ART with pregnancy complications, pregnancy outcomes, child health outcomes, and adverse maternal health outcomes. For example, the birth-linked infant death file information allows comparing the rates and causes of death of ART-born children with the rates of other children.
- Trends in the association of ART with specific health outcomes, and trends in the overall impact of ART on the health of mothers and infants. Currently, efforts are under way by the SMART Collaborative to develop a surveillance plan in each state to use these data to monitor overall trends in infertility occurrence and ART outcomes.
Through the Collaborative, continuing research has been conducted to guide the development of a surveillance system to monitor ART-related maternal and infant health outcomes. This Collaborative has also resulted in a number of articles published using the linked dataset. Several papers have been published including the following:
Tong VT, Kissin DM, Bernson D, Copeland G, Boulet SL, Zhang Y, Jamieson DJ, England LJ. Maternal Smoking Among Women With and Without Use of Assisted Reproductive Technologies. J Womens Health. (Larchmt). 2016–25(10):1066–1072.
Dhalwani NN, Boulet SL, Kissin DM, Zhang Y, McKane P, Bailey MA, Hood ME, Tata LJ. Assisted reproductive technology and perinatal outcomes: conventional versus discordant-sibling design. Fertil Steril. 2016–106(3):710–716.
Boulet SL, Kirby RS, Reefhuis J, Zhang Y, Sunderam S, Cohen B, Bernson D, Copeland G, Bailey MA, Jamieson DJ, Kissin DM. Assisted Reproductive Technology and Birth Defects Among Liveborn Infants in Florida, Massachusetts, and Michigan, 2000–2010. JAMA Pediatr. 2016;170(6):e154934.
Martin AS, Zhang Y, Crawford S, Boulet SL, McKane P, Kissin DM, Jamieson DJ; States Monitoring Assisted Reproductive Technology (SMART) Collaborative. Antenatal Hospitalizations Among Pregnancies Conceived With and Without Assisted Reproductive Technology. Obstet Gynecol. 2016–127(5):941–50.
Luke S, Sappenfield WM, Kirby RS, McKane P, Bernson D, Zhang Y, Chuong F, Cohen B, Boulet SL, Kissin DM. The Impact of ART on Live Birth Outcomes: Differing Experiences across Three States. Paediatr Perinat Epidemiol. 2016;30(3):209–16
Crawford S, Fussman C, Bailey M, Bernson D, Jamieson DJ, Murray-Jordan M, Kissin DM. Estimates of lifetime infertility from three states: the behavioral risk factor surveillance system. J Womens Health (Larchmt). 2015;24(7):578–86.
Boulet SL, Crawford S, Zhang Y, Sunderam S, Cohen B, Bernson D, McKane P, Bailey MA, Jamieson DJ, Kissin DM. States Monitoring ART Collaborative. Embryo transfer practices and perinatal outcomes by insurance mandate status. Fertil Steril. 2015–104(2):403–9.
Dunietz GL, Holzman C, McKane P, Li C, Boulet SL, Todem D, Kissin DM, Copeland G, Bernson D, Sappenfield WM, Diamond MP. Assisted reproductive technology and the risk of preterm birth among primiparas. Fertil Steril. 2015–103(4):974–979.
Cohen B, Bernson D, Sappenfield W, et al. Accuracy of Assisted Reproductive Technology information on birth certificates: Florida and Massachusetts, 2004–2006. Paediatric and Perinatal Epidemiology. 2014;28:181–90.
Grigorescu V, Zhang Y, Kissin DM, et al. Maternal characteristics and pregnancy outcomes after assisted reproductive technology by infertility diagnosis: ovulatory dysfunction versus tubal obstruction. Fertil Steril. 2014;101:1019-25.
Mneimneh AS, Boulet SL, Sunderam S, et al. States Monitoring Assisted Reproductive Technology (SMART) collaborative: data collection, linkage, dissemination, and use. J Womens Health. 2013;22:571-77.
- Page last reviewed: February 8, 2017
- Page last updated: February 17, 2017
- Content source:
- Maintained By:


 ShareCompartir
ShareCompartir