Biggest Threats
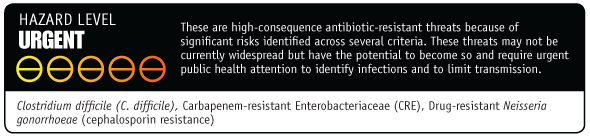
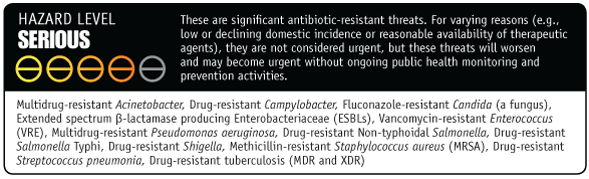
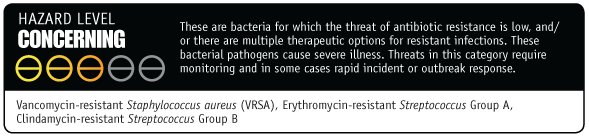
In general, threats assigned to the urgent and serious categories require more monitoring and prevention activities, whereas the threats in the concerning category require less. Regardless of category, threat-specific CDC activities are tailored to meet the epidemiology of the infectious agent and to address any gaps in the ability to detect resistance and to protect against infections.
On this Page
Clostridium Difficile (CDIFF)
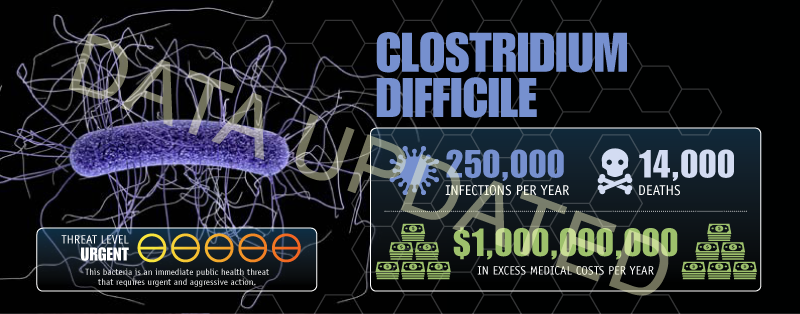
Clostridium difficile (C. difficile) causes life-threatening diarrhea. These infections mostly occur in people who have had both recent medical care and antibiotics. Often, C. difficile infections occur in hospitalized or recently hospitalized patients.
Update: A 2015 CDC study found that C. difficile caused almost half a million infections among patients in the United States in a single year. An estimated 15,000 deaths are directly attributable to C. difficile infections, making it a substantial cause of infectious disease death in the United States. We estimate that up to $3,800,000,000 in medical costs could be saved over 5 years.
Carbapenem-Resistant Enterobacteriaceae (CRE)
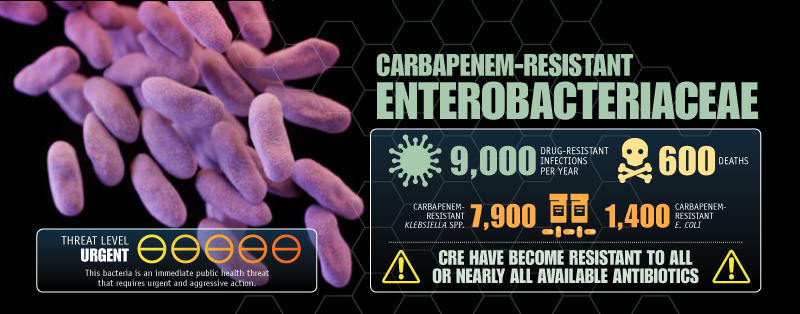
Untreatable and hard-to-treat infections from carbapenem-resistant Enterobacteriaceae (CRE) bacteria are on the rise among patients in medical facilities. CRE have become resistant to all or nearly all the antibiotics we have today. Almost half of hospital patients who get bloodstream infections from CRE bacteria die from the infection.
Neisseria gonorrhoeae

Neisseria gonorrhoeae causes gonorrhea, a sexually transmitted disease that can result in discharge and inflammation at the urethra, cervix, pharynx, or rectum.
Multidrug-Resistant Acinetobacter
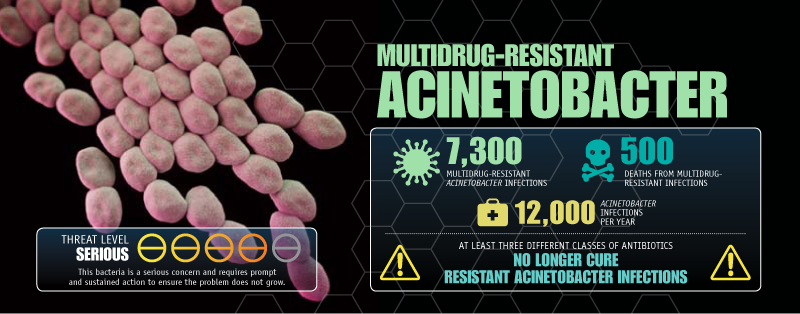
Acinetobacter is a type of gram-negative bacteria that is a cause of pneumonia or bloodstream infections among critically ill patients. Many of these bacteria have become very resistant to antibiotics.
Drug-Resistant Campylobacter
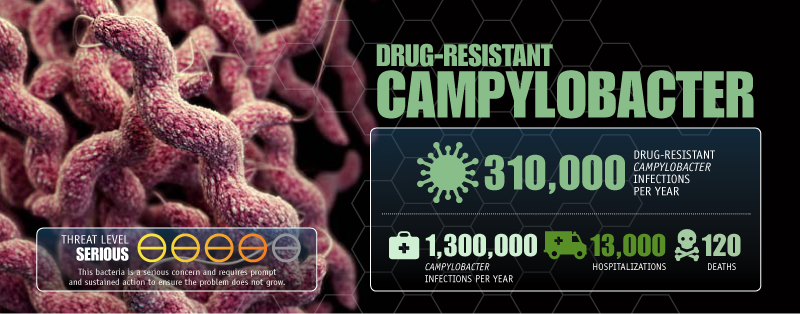
Campylobacter usually causes diarrhea (often bloody), fever, and abdominal cramps, and sometimes causes serious complications such as temporary paralysis.
Fluconazole-Resistant Candida
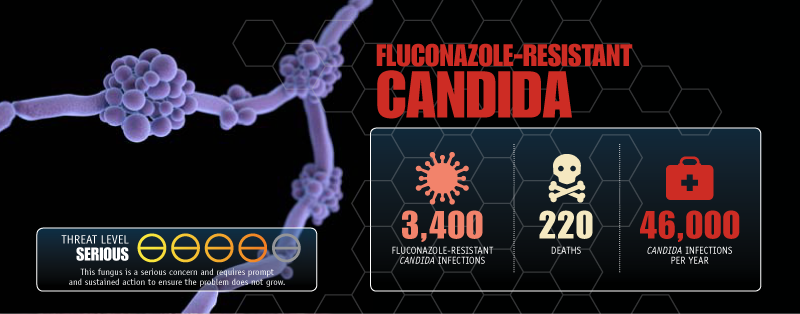
Candidiasis is a fungal infection caused by yeasts of the genus Candida. There are more than 20 species of Candida yeasts that can cause infection in humans, the most common of which is Candida albicans. Candida yeasts normally live on the skin and mucous membranes without causing infection. However, overgrowth of these microorganisms can cause symptoms to develop. Symptoms of candidiasis vary depending on the area of the body that is infected.
Candida is the fourth most common cause of healthcare-associated bloodstream infections in the United States. In some hospitals it is the most common cause. These infections tend to occur in the sickest patients.
Extended Spectrum Enterobacteriaceae (ESBL)
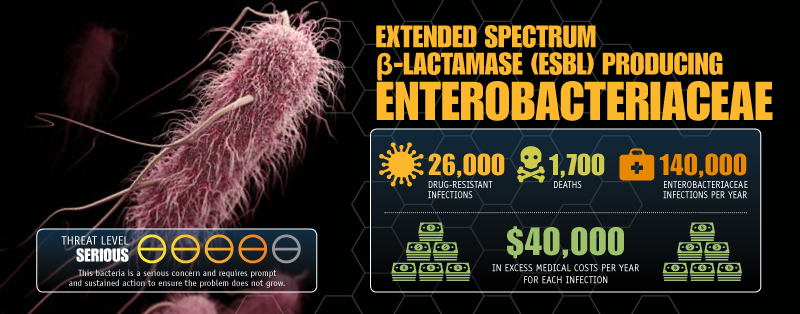
Extended-spectrum β-lactamase is an enzyme that allows bacteria to become resistant to a wide variety of penicillins and cephalosporins. Bacteria that contain this enzyme are known as ESBLs or ESBL-producing bacteria. ESBL-producing Enterobacteriaceae are resistant to strong antibiotics including extended spectrum cephalosporins.
Vancomycin-Resistant Enterococcus (VRE)
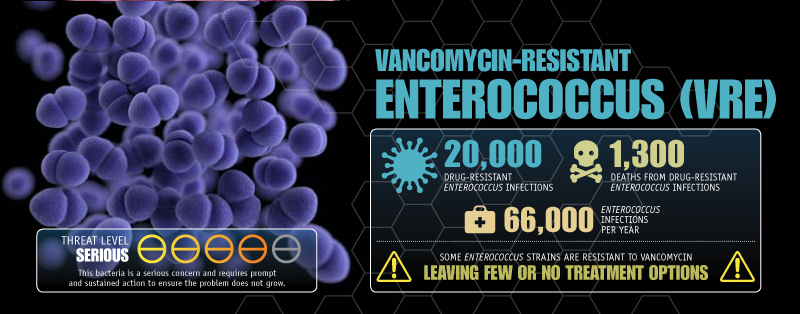
Enterococci cause a range of illnesses, mostly among patients receiving healthcare, but includes bloodstream infections, surgical site infections, and urinary tract infections.
Multidrug-Resistant Pseudomonas Aeruginosa
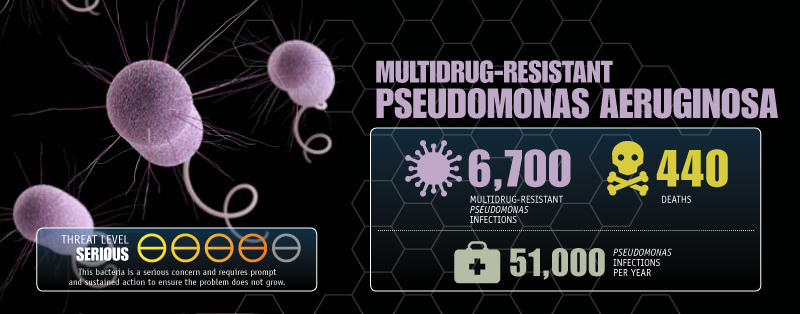
Pseudomonas aeruginosa is a common cause of healthcare-associated infections including pneumonia, bloodstream infections, urinary tract infections, and surgical site infections.
Drug-Resistant Non-Typhoidal Salmonella
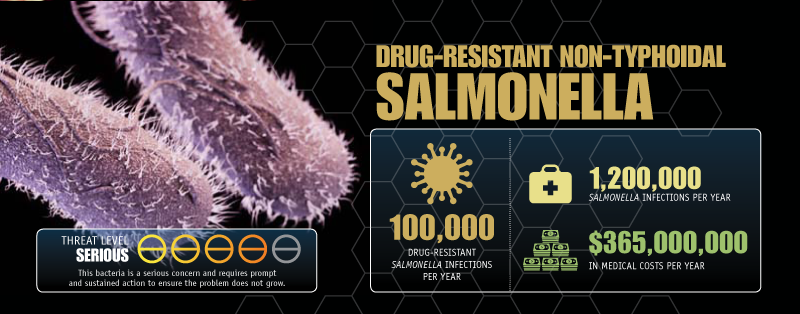
Non-typhoidal Salmonella (serotypes other than Typhi, Paratyphi A, Paratyphi B, and Paratyphi C) usually causes diarrhea (sometimes bloody), fever, and abdominal cramps. Some infections spread to the blood and can have life-threatening complications.
Drug-Resistant Salmonella Serotype Typhi
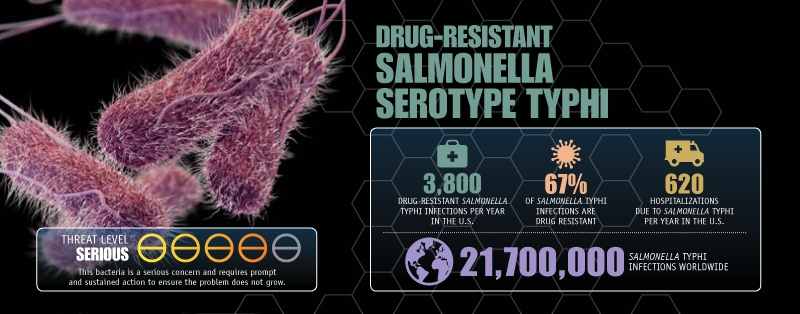
Salmonella serotype Typhi causes typhoid fever, a potentially life-threatening disease. People with typhoid fever usually have a high fever, abdominal pain, and headache. Typhoid fever can lead to bowel perforation, shock, and death.
Drug-Resistant Shigella
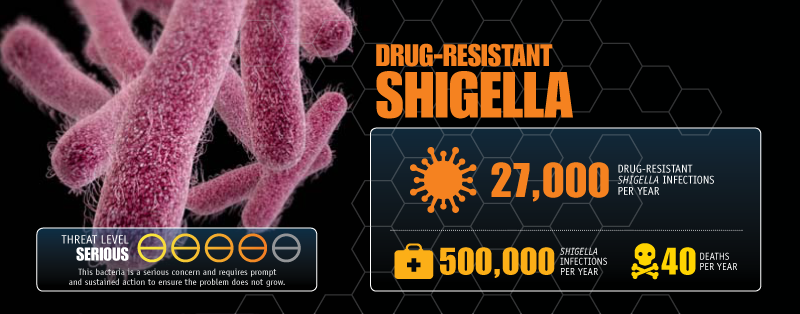
Shigella usually causes diarrhea (sometimes bloody), fever, and abdominal pain. Sometimes it causes serious complications such as reactive arthritis. High-risk groups include young children, people with inadequate handwashing and hygiene habits, and men who have sex with men.
Methicillin-Resistant Staphylococcus Aureus (MRSA)
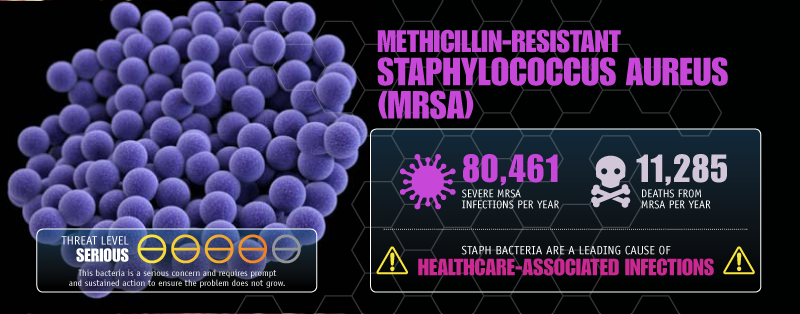
Methicillin-resistant Staphylococcus aureus (MRSA) causes a range of illnesses, from skin and wound infections to pneumonia and bloodstream infections that can cause sepsis and death. Staph bacteria, including MRSA, are one of the most common causes of healthcare-associated infections.
Drug-Resistant Streptococcus Pneumoniae
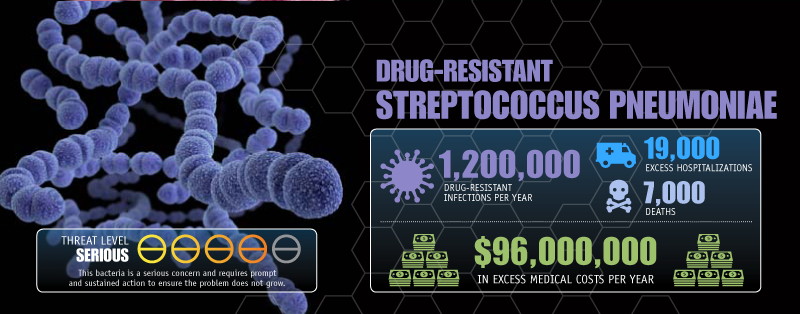
Streptococcus pneumoniae (S. pneumoniae, or pneumococcus) is the leading cause of bacterial pneumonia and meningitis in the United States. It also is a major cause of bloodstream infections and ear and sinus infections.
Drug-Resistant Tuberculosis
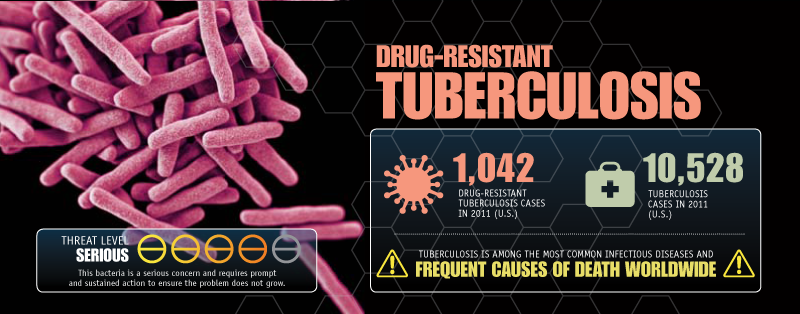
Tuberculosis (TB) is among the most common infectious diseases and a frequent cause of death worldwide. TB is caused by the bacteria Mycbacterium tuberculosis (M. tuberculosis) and is spread mostly through the air. M. tuberculosis can affect any part of the body, but disease is found most often in the lungs. In most cases, TB is treatable and curable with the available first-line TB drugs; however, in some cases, M. tuberculosis can be resistant to one or more of the drugs used to treat it. Drug-resistant TB is more challenging to treat – it can be complex and requires more time and more expensive drugs that often have more side effects. Extensively drug-resistant TB (XDR TB) is resistant to most TB drugs; therefore the patients are left with treatment options that are much less effective. The major factors driving TB drug resistance are incomplete or wrong treatment, short drug supply, and lack of new drugs. In the United States most drug-resistant TB is found among persons born outside of the country.
Vancomycin-Resistant Staphylococcus Aureus
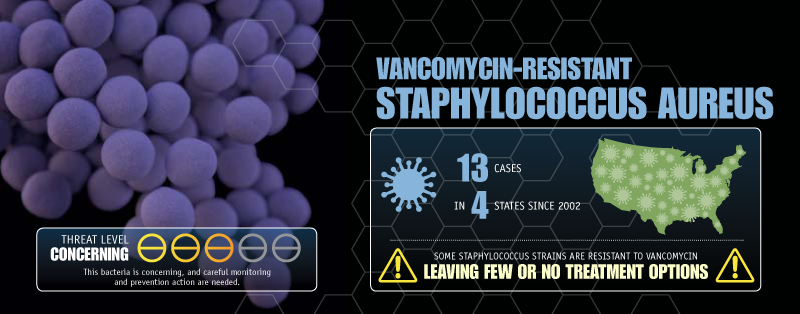
Staphylococcus aureus is a common type of bacteria that is found on the skin. During medical procedures when patients require catheters or ventilators or undergo surgical procedures, Staphylococcus aureus can enter the body and cause infections. When Staphylococcus aureus becomes resistant to vancomycin, there are few treatment options available because vancomycin-resistant S. aureus bacteria identified to date were also resistant to methicillin and other classes of antibiotics.
Erythromycin-Resistant Group A Streptococcus
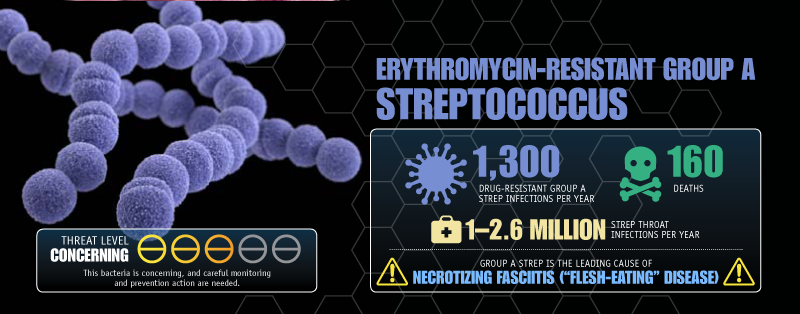
Group A Streptococcus (GAS) causes many illnesses, including pharyngitis (strep throat), streptococcal toxic shock syndrome, necrotizing fasciitis (“flesh-eating” disease), scarlet fever, rheumatic fever, and skin infections such as impetigo.
Clindamycin-Resistant Group B Streptococcus
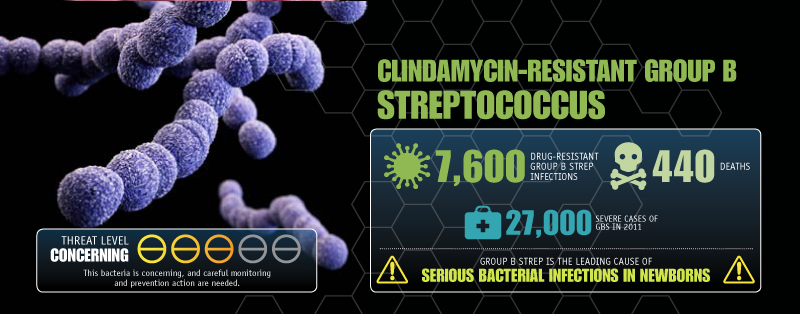
Group B Streptococcus (GBS) is a type of bacteria that can cause severe illness in people of all ages, ranging from bloodstream infections (sepsis) and pneumonia to meningitis and skin infections.
- Page last reviewed: September 8, 2016
- Page last updated: April 14, 2017
- Content source:


 ShareCompartir
ShareCompartir