CDC Innovations: Real-Time Data Strengthens Uganda’s Efforts to End Mother-to-Child HIV Transmission

Fewer and fewer Ugandan babies are being born HIV-infected thanks to national efforts, supported by PEPFAR, to eliminate mother-to-child transmission of HIV. Photo credit: Betty Kagoro, CDC
Identifying opportunities to improve global health sometimes requires creative thinking and new collaborations. In Uganda, the Centers for Disease Control and Prevention (CDC) exemplified this approach in developing a strategy to use the Emergency Operations Center (EOC) in Kampala – established with CDC’s assistance in 2013 – to help eliminate mother-to-child HIV transmission (MTCT).
“The Uganda EOC seemed ideally equipped to support the systems needed to collect and report data that would monitor the rollout and ongoing implementation of the national strategy to eliminate MTCT,” said then CDC-Uganda Country Director Tadesse Wuhib, MD MPH. The rationale for his innovative idea was that since Uganda’s First Lady, Hon. Janet Kataaha Museveni, had declared MTCT a national energency, couldn’t the EOC serve the needs of this public health emergency response? After all, in 2011, CDC Director Thomas R. Frieden, MD MPH, had similarly activated CDC’s EOC in Atlanta to focus and strengthen efforts in the pursuit of polio eradication.
This unique leveraging of a proven HIV prevention strategy and existing resource is now not only helping to keep newborns in Uganda HIV-free, but is also demonstrating the tremendous value of having systems that capture health information electronically and using the collected data to make fast course corrections to improve programs and achieve greater public health impact.
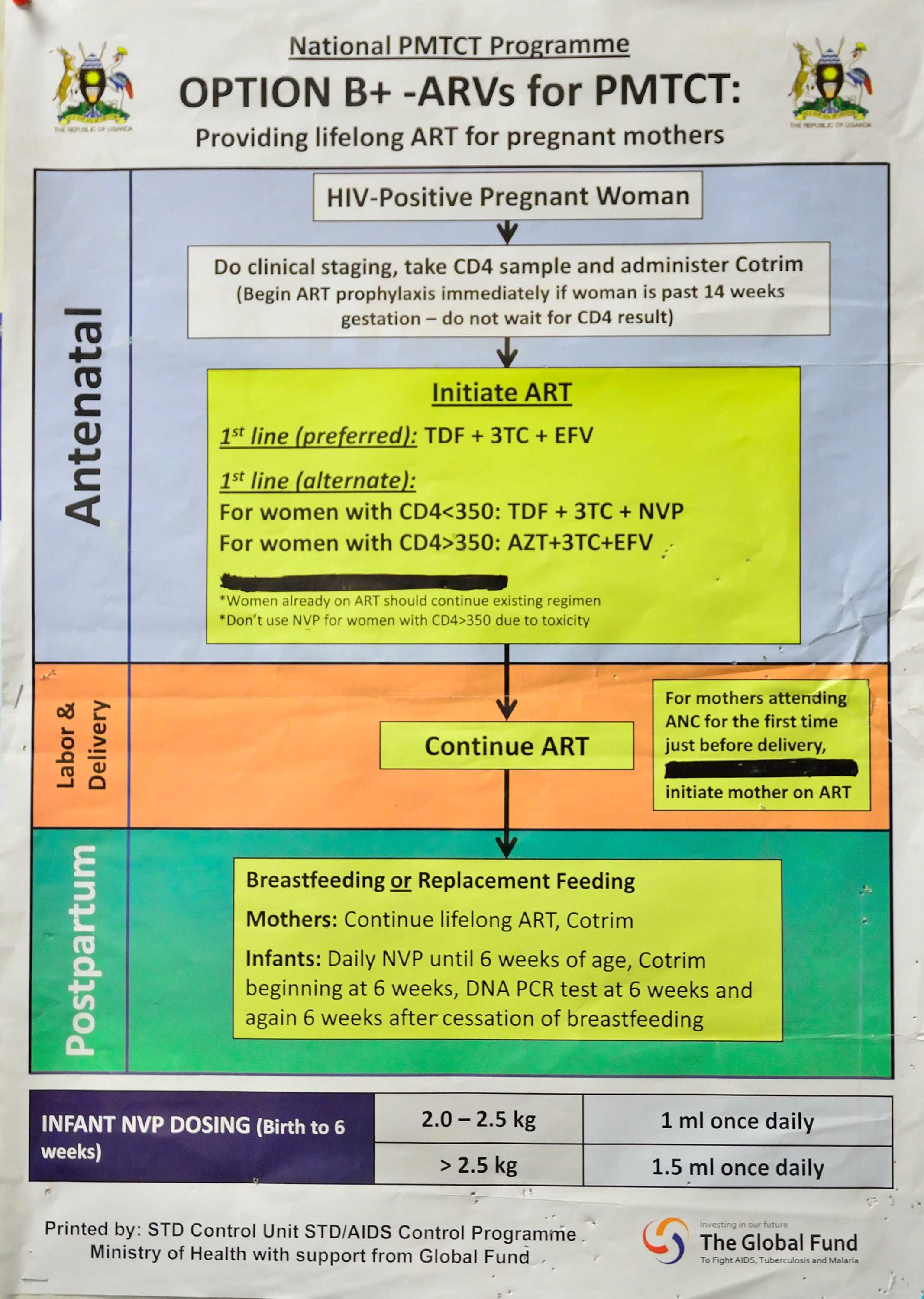
Uganda was one of the first countries in the world to adopt WHO’s Option B+ strategy to eliminate mother-to-child HIV transmission. This chart developed by the Uganda Ministry of Health guides health care workers in providing appropriate care and treatment to pregnant women who test positive for HIV.
Focus on high-impact interventions
Preventing MTCT has long been known as a highly effective intervention with huge potential to stem the tide of new pediatric HIV infections and improve both maternal and child health. Uganda’s Ministry of Health (MOH) was an early adopter of this prevention approach, introducing it in 2000 and subsequently scaling it up nationwide in 2005. Nonetheless, the number of infants continuing to be infected with HIV at birth remained unacceptably high; in 2013, an estimated 16,000 Ugandan babies were diagnosed HIV-positive.
This continued disease burden led Uganda to become one of the first countries to implement the World Health Organization’s treatment recommendation known as Option B+. This approach is fully supported by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), in which CDC plays a key role. Under Option B+, all pregnant and breastfeeding women living with HIV are offered lifelong antiretroviral treatment (ART). Not only does this reduce MTCT to less than five percent, it also maintains the mother’s health, reduces the risk of her transmitting HIV to uninfected sexual partners, and minimizes the risk of MTCT in future pregnancies.
Option B+ is part of Uganda’s comprehensive national strategy to eliminate MTCT, which aims to reduce new HIV infections in children by 90 percent and decrease HIV-associated maternal deaths by 50 percent by 2015 from the 2009 baseline. The strategy uses a four-pronged approach: (1) primary prevention of HIV in women of reproductive age, (2) prevention of unintended pregnancies in women living with HIV/AIDS, (3) provision of antiretroviral drugs to HIV-infected pregnant and lactating women to reduce MTCT risk, and (4) comprehensive care and support for HIV-infected women and their families.
With their ambitious national strategy in place, all that remained was to identify a method for effective, rapid monitoring of the initiative’s roll-out and impact. This is where CDC stepped in, leveraging systems put in place under President Obama’s Global Health Security Agenda (GHSA) for which Uganda was a pilot site.

An HIV-positive mother gave birth to a healthy, HIV-free daughter thanks to Uganda’s national campaign to eliminate mother-to-child HIV transmission. Photo credit: Baylor-Uganda
From health security to healthy babies
Put simply, GHSA aims to improve the ability of countries to prevent, detect, and respond to infectious disease outbreaks such as Ebola and cholera. As part of the GHSA pilot project, CDC helped the (MOH) establish an EOC modeled on CDC’s own at its headquarters in Atlanta. To help implement the MTCT strategy, CDC used an existing project it supports in Uganda known as META—Monitoring and Evaluation Technical Assistance—to manage the data coming into the EOC. META is a partnership between the Makerere University School of Public Health and the University of California, San Francisco.
A team comprised of members from the MOH, CDC, and the United States Agency for International Development (USAID), and other stakeholders recommended nine indicators for weekly data reporting. Additionally, CDC’s Health Information System team evaluated the mobile SMS reporting component of Uganda’s national health management information system and then customized and stood up the weekly reporting platform. Further, META and CDC provided training to PEPFAR-funded implementing partners (IPs) in Uganda on how to submit their reports, and IPs cascaded this training down to the health -facility level, often to midwives.

This Ugandan family is a beneficiary of CDC-supported services to eliminate mother-to-child HIV transmission through Reach out Mbuya in Kampala.
Monitoring program implementation in real time
“The key to this entire concept is the generation, management, and dissemination of data that quickly demonstrate the results we are achieving,” says Dr. Wuhib. Data are gathered weekly via SMS text messages received from facility health care workers through a special toll-free number. Information from the data is collected, collated, and analyzed every week and a report is then generated and distributed. Data are also available in real time through a web-based, open-source dashboard (http://reports.dhis2sms.ug) accessible to all stakeholders with no password. The data are used to monitor progress toward achieving set targets and to identify bottlenecks and enable appropriate and timely corrective action. A team of national stakeholders—including MOH , CDC, USAID, META, Uganda’s Central Public Health Laboratory , representatives of MOH’s Pharmacy and Warehouse Divisions, PEPFAR-funded IPs, and District Health Officers (DHOs)—meets weekly at the EOC and identifies follow-up actions disseminated through the report.
META’s Project Manager, Evelyn Akello, says the weekly reporting focuses on quality of service, including the number of women tested, numbers of women initiated on Option B+, stock-outs of commodities, missed appointments, as well as broad progress on Option B+ implementation. “The weekly meetings and corrective actions taken resulted in increased health facility reporting rates, which grew from from 27 percent in October 2013 to 88 percent in November 2014 (Week 46). It also reduced stock-outs of commodities, for example, reported HIV test kits stock-outs decreased from 156 sites (Week 1) to 28 sites (Week 46, November 2014).”
Akello also notes that, contrary to what may be commonly thought, the technology used is not the most important investment made. “The greatest investments are the availability of human resources through all our stakeholders. The momentum of the weekly meetings is crucial for a successful and responsive monitoring system,” she said.

Seemingly beating the odds, an HIV-positive mother in Uganda gave birth to HIV-free twins after receiving appropriate treatment services made possible by PEPFAR. Photo credit: Baylor-Uganda
Challenges, lessons learned—and timely solutions
The project has not been without its challenges, of course. In the beginning, low reporting rates were observed, but they improved significantly following an intervention by MOH leadership directing DHOs to submit data. Regular troubleshooting by META and CDC has helped address technology issues. Other common reporting challenges include a lack of data-collection tools and data quality from some facilities or districts, but fundamentally, the availability of the data has provided a solid basis for timely action.
Results of this innovative use of an EOC platform for program implementation show clearly that real-time data play a pivotal role in public health decision making. Facilities have been able to reduce missed appointments and increase monitoring of women tested and initiated on ART. Districts use the data to monitor their MTCT programs and make timely adjustments, and CDC, along with other partners, is looking at ways to incorporate new indicators and to establish more formal district monitoring teams to use the data to improve aspects like retention in care. At the national level, the data are being used to monitor district performance and identify gaps in service delivery. For CDC, the data allow greater focus on more robust planning and IP performance.
As PEPFAR focuses more sharply on epidemic control, effective surveillance and program monitoring and evaluation become even more crucial. CDC, as a scientific and technical agency and key implementer of the PEPFAR partner program, is uniquely poised to provide innovative approaches to these needs. Preventing Uganda’s children from acquiring HIV at birth is achievable, but requires an organized, accessible, and well-functioning information system as a key component of the nation’s overall health system. CDC’s cost-effective experiment in leveraging health security infrastructure for improving the nation’s HIV response may have demonstrated an unexpected way to achieve just that.
- Page last reviewed: August 30, 2016
- Page last updated: August 30, 2016
- Content source:


 ShareCompartir
ShareCompartir