Post-Streptococcal Glomerulonephritis
Post-streptococcal glomerulonephritis (PSGN) is an immunologically-mediated sequela of pharyngitis or skin infections caused by nephritogenic strains of Streptococcus pyogenes, which is also called group A Streptococcus or group A strep. The etiology, clinical features, diagnosis and treatment options, prognosis and complications, and prevention are described below.
Etiology
PSGN is an immunologically-mediated, nonsuppurative, delayed sequela of pharyngitis or skin infections caused almost universally by nephritogenic strains of S. pyogenes. Outbreaks of PSGN caused by group C streptococci are rare but have been reported. 1,2
S. pyogenes are gram-positive cocci that grow in chains (see figure 1). They exhibit β-hemolysis (complete hemolysis) when grown on blood agar plates. They belong to group A in the Lancefield classification system for β-hemolytic Streptococcus, and thus are also called group A streptococci.1
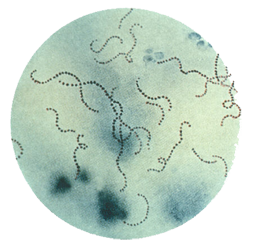
Figure 1. Streptococcus pyogenes (group A Streptococcus) on Gram stain. Source: Public Health Image Library, CDC
Clinical Features
The clinical features of acute glomerulonephritis include:
- Edema (often pronounced facial and orbital edema, especially on arising in the morning)
- Hypertension
- Proteinuria
- Macroscopic hematuria, with urine appearing dark, reddish-brown
- Complaints of lethargy, generalized weakness, or anorexia
Laboratory examination usually reveals mild normocytic normochromic anemia, slight hypoproteinemia, elevated blood urea nitrogen and creatinine, elevated erythrocyte sedimentation rate, and low total hemolytic complement and C3 complement. Urine output is usually decreased, and urine examination often reveals protein (usually <3 grams per day) and hemoglobin with red blood cell casts.
Additionally, some evidence from epidemic situations indicates that subclinical cases of PSGN may occur, as some individuals may have symptoms that are mild enough to not come to medical attention.1
Transmission
As a delayed sequelae of group A strep infection, PSGN is not contagious. However, group A strep are most commonly spread through direct person-to-person transmission, typically through saliva or nasal secretions from an infected person. Ill persons, such as those with group A strep pharyngitis, scarlet fever, or impetigo, are much more likely to transmit the bacteria than asymptomatic carriers. Crowded conditions — such as those in schools, daycare centers, or military training facilities — facilitate transmission. Although rare, spread of group A strep infections may also occur via food. Foodborne outbreaks of pharyngitis have occurred due to improper food handling. Fomites, such as household items like plates or toys, are very unlikely to spread these bacteria.
Humans are the primary reservoir for group A strep. There is no evidence to indicate that pets can transmit the bacteria to humans.
Incubation Period
PSGN occurs after a latent period of approximately 10 days following group A strep pharyngitis and up to 3 weeks following group A strep skin infections.1
Risk Factors
The risk factors for PSGN are the same as for the preceding group A strep pharyngitis or skin infection (like impetigo). PSGN is more common in children, although it can occur in adults. Pharyngitis-associated PSGN is most common among children of early school age, while pyoderma-associated PSGN is most common among children of pre-school age.
There are no known risk factors specific for PSGN, although the risk of PSGN is increased if a nephritogenic strain of group A strep is introduced into a household.
Diagnosis and Testing
The differential diagnosis of PSGN includes other infectious and non-infectious causes of acute glomerulonephritis. The diagnosis of PSGN is made based on clinical history and findings in the setting of evidence of a preceding group A strep infection, including isolation of group A strep from throat or skin lesions or elevated streptococcal antibodies.1
Treatment
Treatment of PSGN is aimed at managing hypertension and edema. Additionally, penicillin (preferably penicillin G benzathine) should be given to eradicate the nephritogenic strain in order to prevent spread of the strain to other people.1
Prognosis and Complications
The prognosis of PSGN in children is very good; more than 90% of children make a full recovery. The proportion of adults with PSGN who have a worse outcome due to residual renal function impairment is higher but not well quantified.1
Prevention
Unfortunately, antibiotics for acute streptococcal infections have not been shown to be effective in preventing PSGN from developing in persons with impetigo or pharyngitis.1,2 Thus, it is important to prevent the primary group A streptococcal skin or pharyngeal infection. However, treating PSGN patients can stop a nephritogenic strain from circulating in a household, and thus prevent additional infections among these close contacts.
The spread of all types of group A strep infection can be reduced by good hand hygiene, especially after coughing and sneezing and before preparing foods or eating, and respiratory etiquette (e.g., covering your cough or sneeze). Treating an infected person with an antibiotic for 24 hours or longer generally eliminates their ability to transmit the bacteria. Thus, people with group A strep pharyngitis or scarlet fever should stay home from work, school, or daycare until afebrile and until at least 24 hours after starting appropriate antibiotic therapy.
Epidemiology
Humans are the only reservoir for group A strep. The attack rate of PSGN following throat or skin infection with a nephritogenic strain of group A strep was measured to be between 10% and 15% in a prospective study performed in the 1960s.5 An estimated 470,000 cases of PSGN and 5,000 deaths from PSGN occur each year globally.3
Resources
- Shulman ST, Bisno AL. Nonsupprative poststreptococcal sequelae: Rheumatic fever and glomerulonephritis. In Bennett J, Dolin R, Blaser M, editors. 8th ed. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Philadelphia (PA). Elsevier. 2015;2:2300–9.
- Bryant AE, Stevens DL. Streptococcus pyogenes. In Bennett J, Dolin R, Blaser M, editors. 8th ed. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Philadelphia (PA). Elsevier. 2015:2:2285–300.
- Carapetis JR. The current evidence for the burden of group A streptococcal diseases. World Health Organization. Geneva. 2005.
- Committee on Infectious Diseases. Group A streptococcal infections. In Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. 30th ed. Red Book: 2015 Report of the Committee on Infectious Diseases. Elk Grove Village (IL). American Academy of Pediatrics. 2015;732–44.
- Anthony BF, Kaplan EL, Wannamaker LW, Briese FW, Chapman SS. Attack rates of acute nephritis after Type 49 streptococcal infection of the skin and of the respiratory tract. J Clin Invest. 1969;48(9):1679–704.
Related Pages
- Page last reviewed: September 16, 2016
- Page last updated: September 16, 2016
- Content source:


 ShareCompartir
ShareCompartir