Norovirus is the leading cause of disease outbreaks from contaminated food in the U.S.
The food service industry can help prevent norovirus outbreaks
This website is archived for historical purposes and is no longer being maintained or updated.
Press Release
Embargoed Until: Tuesday, June 3, 2014, 1:00 p.m. ET
Contact: Media Relations
(404) 639-3286
Norovirus Questions and Answers.
Entire Infographic
Most norovirus outbreaks from contaminated food occur in food service settings, according to a Vital Signs report by the Centers for Disease Control and Prevention. Infected food workers are frequently the source of these outbreaks, often by touching ready-to-eat foods served in restaurants with their bare hands. The food service industry can help prevent norovirus outbreaks by enforcing food safety practices, such as making sure workers always practice good hand hygiene on the job and stay home when they are sick.
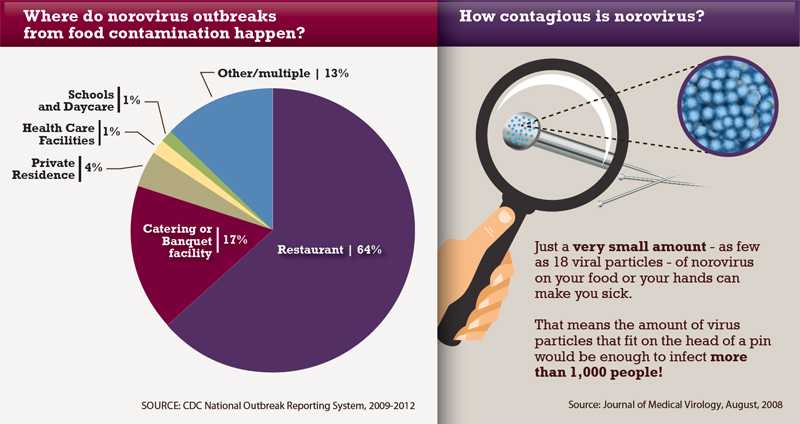
Norovirus often gets a lot of attention for outbreaks on cruise ships, but those account for only about 1 percent of all reported norovirus outbreaks. Norovirus is highly contagious and can spread anywhere people gather or food is served, making people sick with vomiting and diarrhea. About 20 million people get sick from norovirus each year; most get infected by having close contact with other infected people or by eating contaminated food.
"Norovirus outbreaks from contaminated food in restaurants are far too common." said CDC Director Tom Frieden, M.D., M.P.H. "All who prepare food, especially the food service industry, can do more to create a work environment that promotes food safety and ensures that workers adhere to food safety laws and regulations that are already in place."
The Vital Signs report provides key recommendations to help the food service industry prevent norovirus outbreaks from contaminated food. The recommendations, which underscore provisions in the Food and Drug Administration model Food Code (http://www.fda.gov/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/default.htm) and CDC guidelines (http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6003a1.htm), include:
- Making sure food service workers practice proper hand washing and use utensils and single-use disposable gloves to avoid touching ready-to-eat foods with bare hands,
- Certifying kitchen managers and training food service workers in food safety practices, and
- Establishing policies that require food service workers to stay home when sick with vomiting and diarrhea and for at least 48 hours after symptoms stop.
"It is vital that food service workers stay home if they are sick; otherwise, they risk contaminating food that many people will eat," said Aron Hall, D.V.M., M.S.P.H., of CDC's Division of Viral Diseases. However, 1 in 5 food service workers have reported working at least once in the previous year while sick with vomiting or diarrhea. Fear of job loss and not wanting to leave coworkers short-staffed were cited as significant factors in their decision. "Businesses can consider using measures that would encourage sick workers to stay home, such as paid sick leave and a staffing plan that includes on-call workers," said Hall.
CDC analyzed norovirus outbreak data reported by state, local, and territorial health departments from 2009 to 2012 through CDC's National Outbreak Reporting System (NORS). Over the four years, health departments reported 1,008 norovirus outbreaks from contaminated food, most of which occurred in food service settings such as restaurants and catering or banquet facilities.
Factors contributing to food contamination were reported in 520 of the outbreaks, with an infected food worker implicated in 364 (70 percent) of them. Of these outbreaks, 196 (54 percent) involved food workers touching ready-to-eat foods with their bare hands. Ready-to-eat foods are foods that are ready to be served without additional preparation, such as washed raw fruits and vegetables for salads or sandwiches, baked goods, or items that have already been cooked.
CDC's analysis also looked at which foods were commonly implicated in norovirus outbreaks. Of 324 outbreaks with a specific food item implicated, more than 90 percent were contaminated during final preparation (such as making a sandwich with raw and already cooked ingredients) and 75 percent were foods eaten raw. Leafy vegetables, fruits, and mollusks, such as oysters, were the most common single food categories implicated in these outbreaks.
The report also highlights the key role health departments play in investigating and reporting norovirus outbreaks. Outbreak reporting rates varied greatly among states, likely illustrating differences in surveillance efforts rather than variation in norovirus disease incidence. "There is a continued need to build the capacity of health departments to more thoroughly investigate and report outbreaks to NORS," said Hall.
About NORS
CDC launched NORS in 2009 to collect information on outbreaks of foodborne, waterborne, and enteric diseases that spread from person-to-person, animals, environmental surfaces, and other or unknown ways. Public health agencies can report all outbreaks of gastroenteritis, including norovirus illness, through this web-based system. This information is used to determine where norovirus outbreaks commonly occur, how the virus is spread, and specific food or water sources involved. In turn, this helps identify the best ways to prevent and control norovirus illnesses and outbreaks.
For more information about norovirus, please visit www.cdc.gov/norovirus. Additional information on preventing foodborne diseases is available at www.foodsafety.gov.
Vital Signs is a CDC report that appears on the first Tuesday of the month as part of the CDC journal Morbidity and Mortality Weekly Report, or MMWR. The report provides the latest data and information on key health indicators. These are cancer prevention, obesity, tobacco use, motor vehicle passenger safety, prescription drug overdose, HIV/AIDS, alcohol use, health care-associated infections, cardiovascular health, teen pregnancy, food safety and developmental disabilities.
- Page last reviewed: June 3, 2014 (archived document)
- Content source:
Error processing SSI file


 ShareCompartir
ShareCompartir