Information for clinicians
Download materials to assist clinicians evaluating and treating skin and soft tissue infections in the era of community-associated MRSA
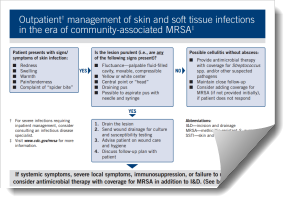
Poster 11″ X 17″ [PDF – 164 KB]
Flyer 8.5″ X 11″ [PDF – 147 KB]
Pocket Card 4″ X 7″ [PDF – 193 KB]
The CDC encourages clinicians to consider MRSA in the differential diagnosis of skin and soft tissue infections (SSTIs) compatible with S. aureus infections, especially those that are purulent (fluctuant or palpable fluid-filled cavity, yellow or white center, central point or “head,” draining pus, or possible to aspirate pus with needle or syringe). A patient’s presenting complaint of “spider bite” should raise suspicion of an S. aureus infection.
Recent data suggest that MRSA as a cause of skin infections in the general community remains at high probability. The spectrum of disease caused by MRSA appears to be similar to that of Staphylococcus aureus in the community. SSTIs, specifically furuncles (abscessed hair follicles or “boils”), carbuncles (coalesced masses of furuncles), and abscesses, are the most frequently reported clinical manifestations. The role of MRSA in cellulitis without abscess or purulent drainage is less clear since cultures are rarely obtained.
For recent MRSA treatment guidance, see Infectious Diseases Society of America (IDSA) website.
In the community, incision and drainage remains the primary therapy for these purulent skin infections. Empiric antimicrobial coverage for MRSA may be warranted in addition to incision and drainage based on clinical assessment (e.g., presence of systemic symptoms, severe local symptoms, immune suppression, extremes of patient age, infections in a difficult to drain area, or lack of response to incision and drainage alone).
Antibiotic treatment, if indicated, should be guided by the susceptibility profile of the organism. Obtaining specimens for culture and susceptibility testing is useful to guide therapy, particularly for those with more severe infections and those who fail to respond adequately to initial management.
MRSA skin infections can develop into more serious infections. It is important to discuss a follow-up plan with your patients in case they develop systemic symptoms or worsening local symptoms, or if symptoms do not improve within 48 hours.
For more information about MRSA in the community, read Strategies for Clinical Management of MRSA in the Community: Summary of an Experts’ Meeting Convened by the Centers for Disease Control and Prevention (March 2006) [PDF – 308K].
- Page last reviewed: February 4, 2016
- Page last updated: April 8, 2016
- Content Source:


 ShareCompartir
ShareCompartir