Pregnancy Mortality Surveillance System

When did CDC start conducting national surveillance of pregnancy-related deaths?
CDC initiated national surveillance of pregnancy-related deaths in 1986 because more clinical information was needed to fill data gaps about causes of maternal death.
How does CDC define pregnancy-related deaths?
For reporting purposes, a pregnancy-related death is defined as the death of a woman while pregnant or within 1 year of pregnancy termination–regardless of the duration or site of the pregnancy–from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
How are the data collected and coded?
Each year, CDC requests the 52 reporting areas (50 states, New York City, and Washington DC) to voluntarily send copies of death certificates for all women who died during pregnancy or within 1 year of pregnancy, and copies of the matching birth or fetal death certificates, if they have the ability to perform such record links. All of the information obtained is summarized, and medically trained epidemiologists determine the cause and time of death related to the pregnancy. Causes of death are coded by using a system established in 1986 by the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention Maternal Mortality Study Group.
How are the data used?
Data are analyzed by CDC scientists. Information about causes of pregnancy-related deaths and risk factors associated with these deaths is released periodically through peer-reviewed literature, CDC’s Morbidity and Mortality Weekly Reports, and the CDC Web site. This information helps clinicians and public health professionals to better understand circumstances surrounding pregnancy-related deaths and to take appropriate actions to prevent them.
How is data confidentiality protected?
Pregnancy mortality surveillance data are protected under 308(d) Assurance of Confidentiality. Because of this Assurance, all data and documents are considered confidential materials and are safeguarded to the greatest extent possible. This Assurance extends to all pregnancy mortality surveillance data obtained from individual states and reporting areas.
What is the pregnancy-related mortality ratio?
The pregnancy-related mortality ratio is an estimate of the number of pregnancy-related deaths for every 100,000 live births. This ratio is often used as an indicator to measure the nation’s health. Factors that affect the health of the entire population can also affect mortality among pregnant and postpartum women.
The pregnancy-related mortality ratio fell significantly in the United States during the 20th century. This historic decline was because of medical and technological advances. Interest and concern at the local, state, and federal levels for why pregnancy-related deaths occur led to the development of systems for identifying, reviewing, and analyzing pregnancy-related deaths.
Trends in Pregnancy-Related Deaths
Since the Pregnancy Mortality Surveillance System was implemented, the number of reported pregnancy-related deaths in the United States steadily increased from 7.2 deaths per 100,000 live births in 1987 to a high of 17.8 deaths per 100,000 live births in 2009 and 2011. The graph below shows trends in pregnancy-related mortality ratios defined as the number of pregnancy-related deaths per 100,000 live births in the United States between 1987 and 2013 (the latest available year of data).
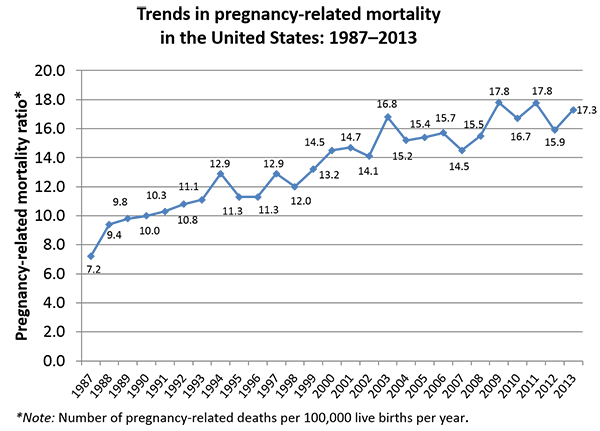
The reasons for the overall increase in pregnancy-related mortality are unclear. The use of computerized data linkages by the states, changes in the way causes of death are coded, and the addition of a pregnancy checkbox to the death certificate in many states have likely improved identification of pregnancy-related deaths over time. Whether the actual risk of a woman dying from pregnancy-related causes has increased is unclear. Many studies show that an increasing number of pregnant women in the United States have chronic health conditions such as hypertension,1 diabetes,2 and chronic heart disease.3 These conditions may put a pregnant woman at higher risk of pregnancy complications. Although the overall risk of dying from pregnancy complications is low, some women are at a higher risk than others. The higher pregnancy-related mortality ratios during 2009–2011 are due to an increase in infection and sepsis deaths. Many of these deaths occurred during the 2009–2010 influenza A (H1N1)pdm09 pandemic which occurred in the United States between April 2009 and June 2010. Influenza deaths accounted for 12 percent of all pregnancy-related deaths during that 15-month period.4 Variability in the risk of death by race, ethnicity, and age indicates that more can be done to understand and reduce pregnancy-related deaths.5
Causes of and risk factors for pregnancy-related deaths between 1987 and 2013 have already been published.9-10 Key pregnancy-related mortality data for 2011–2013 (the latest data available) are summarized below.
In the United States
Of the 5,259 deaths within a year of pregnancy completion that occurred during 2011–2013 and were reported to CDC, 2,009 were found to be pregnancy-related. The pregnancy-related mortality ratios were 17.8, 15.9, and 17.3 deaths per 100,000 live births in 2011, 2012 and 2013, respectively.
Considerable racial disparities in pregnancy-related mortality exist. During 2011–2013, the pregnancy-related mortality ratios were–
- 12.7 deaths per 100,000 live births for white women.
- 43.5 deaths per 100,000 live births for black women.
- 14.4 deaths per 100,000 live births for women of other races.
The graph below shows percentages of pregnancy-related deaths in the United States during 2011–2013 caused by–
- Cardiovascular diseases, 15.5%.
- Non-cardiovascular diseases, 14.5%.
- Infection or sepsis, 12.7%.
- Hemorrhage, 11.4%.
- Cardiomyopathy, 11.0%.
- Thrombotic pulmonary embolism, 9.2%.
- Hypertensive disorders of pregnancy, 7.4%.
- Cerebrovascular accidents, 6.6%.
- Amniotic fluid embolism, 5.5%.
- Anesthesia complications, 0.2%.
The cause of death is unknown for 6.1% of all 2011–2013 pregnancy-related deaths.

Note: The cause of death is unknown for 6.1% of all 2011-2013 pregnancy-related deaths.
References
- Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States: 1998–2006. Obstet Gynecol. 2009;113(6):1299–1306.
- Albrecht SS, Kuklina EV, Bansil P et al. Diabetes trends among delivery hospitalizations in the United States, 1994–2004. Diabetes Care. 2010;33(4):768–773.
- Kuklina EV, Callaghan WM. Chronic heart disease and severe obstetric morbidity among hospitalizations for pregnancy in the USA: 1995–2006. Br J Obstet Gynaecol. 2011;118(3): 345–352.
- Callaghan WM, Creanga AA, Jamieson DJ. Pregnancy-Related Mortality Due to Influenza in the United States During the 2009–2010 Pandemic. Obstet Gynecol. 2015; 126:486–490.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce C, Callaghan WM. Race, ethnicity and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol. 2012;120(2):261-8.
- Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987–1990. Obstet Gynecol. 1996;88:161–167.
- Berg CJ, Chang J, Callaghan WM, Whitehead SJ. Pregnancy-related mortality in the United States, 1991–1997. Obstet Gynecol. 2003;101:289-296.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998–2005. Obstet Gynecol. 2010;116:1302–1309.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce C, Callaghan WM. Pregnancy-Related Mortality in the United States, 2006–2010. Obstetrics & Gynecology. 2015;125(1):5–12.
- Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-Related Mortality in the United States, 2011-2013. Obstetrics & Gynecology. 2017;130(2).
- Page last reviewed: June 29, 2017
- Page last updated: June 29, 2017
- Content source:


 ShareCompartir
ShareCompartir