Today’s Heroin Epidemic
More people at risk, multiple drugs abused
On This Page
Overview
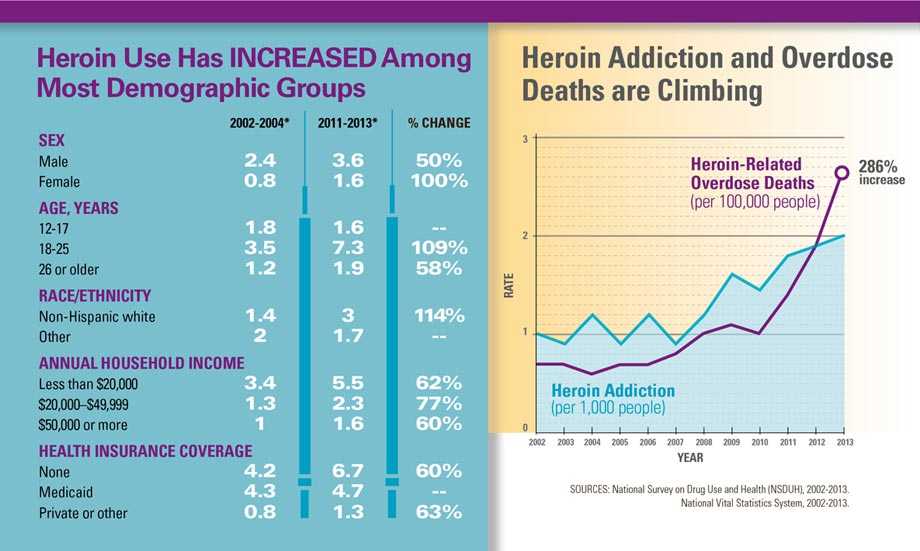
Heroin use has increased across the US among men and women, most age groups, and all income levels. Some of the greatest increases occurred in demographic groups with historically low rates of heroin use: women, the privately insured, and people with higher incomes. Not only are people using heroin, they are also abusing multiple other substances, especially cocaine and prescription opioid painkillers. As heroin use has increased, so have heroin-related overdose deaths. Between 2002 and 2013, the rate of heroin-related overdose deaths nearly quadrupled, and more than 8,200 people died in 2013. States play a central role in prevention, treatment, and recovery efforts for this growing epidemic.
States can:
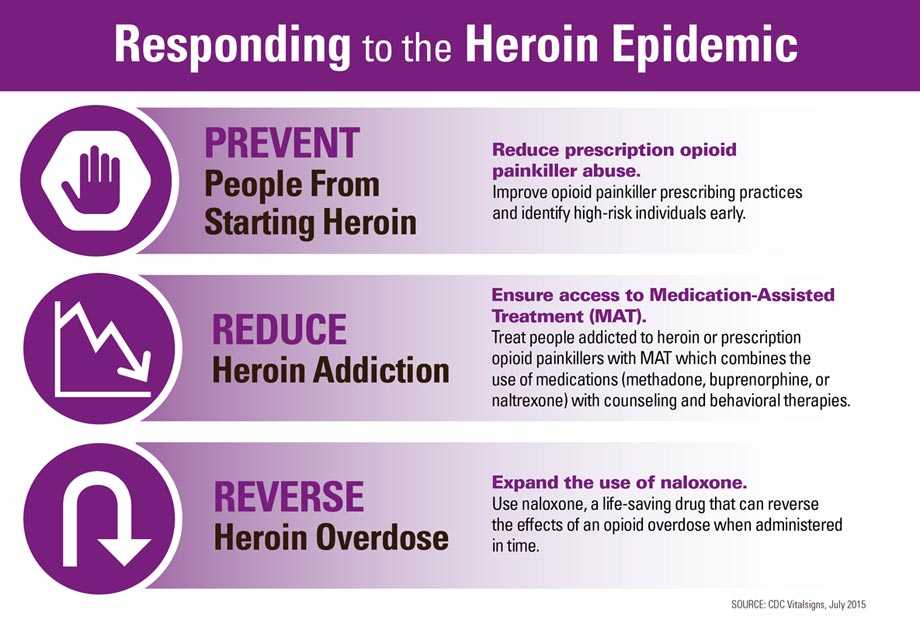
- Address the strongest risk factor for heroin addiction: addiction to prescription opioid painkillers.
- Increase access to substance abuse treatment services, including Medication-Assisted Treatment (MAT), for opioid addiction.
- Expand access to and training for administering naloxone to reduce opioid overdose deaths.
- Ensure that people have access to integrated prevention services, including access to sterile injection equipment from a reliable source, as allowed by local policy.
- Help local jurisdictions to put these effective practices to work in communities where drug addiction is common.

Heroin use more than doubled among young adults ages 18–25 in the past decade.
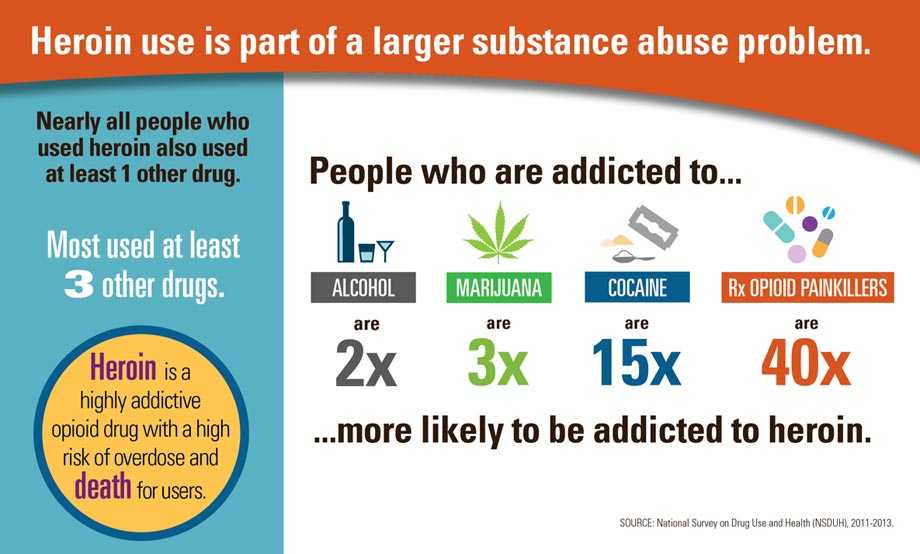
More than 9 in 10 people who used heroin also used at least one other drug.
45% of people who used heroin were also addicted to prescription opioid painkillers.
Problem
Heroin use is increasing, and so are heroin-related overdose deaths.
How is heroin harmful?
- Heroin is an illegal, highly addictive opioid drug.
- A heroin overdose can cause slow and shallow breathing, coma, and death.
- People often use heroin along with other drugs or alcohol. This practice is especially dangerous because it increases the risk of overdose.
- Heroin is typically injected but is also smoked or snorted. When people inject heroin, they are at risk of serious, long-term viral infections such as HIV, Hepatitis C, and Hepatitis B, as well as bacterial infections of the skin, bloodstream, and heart.
Who is most at risk of heroin addiction?
- People who are addicted to prescription opioid painkillers
- People who are addicted to cocaine
- People without insurance or enrolled in Medicaid
- Non-Hispanic whites
- Males
- People who are addicted to marijuana and alcohol
- People living in a large metropolitan area
- 18 to 25 year olds
What Can Be Done
The Federal government is
- Providing educational training and resources to health care providers so they can make informed decisions and ensure the appropriate prescribing of opioid painkillers. This includes:
- Developing prescribing guidelines for chronic pain.
- Supporting the use of prescription drug monitoring programs (electronic databases that track the dispensing of certain drugs) as a routine part of clinical practice.
- Increasing access to substance abuse treatment services through the Affordable Care Act.
- Expanding use of Medication-Assisted Treatment (MAT).
- Supporting the development and distribution of the life-saving drug naloxone to reduce prescription opioid painkiller and heroin overdose deaths.
- Supporting the research, development, and approval of pain medications that are less prone to abuse.
- Improving surveillance to better track trends, identify communities at risk, and target prevention strategies.
States can
- Address the strongest risk factor for heroin addiction: addiction to prescription opioid painkillers.
- Make prescription drug monitoring programs timely and easy to use. Providers can analyze patient prescription drug history and make informed decisions before prescribing opioid painkillers.
- Look at the data and practices of state Medicaid and worker’s compensation programs to identify and reduce inappropriate prescribing.
- Increase access to substance abuse treatment services, including MAT for opioid addiction.
- Work with Medicaid and other insurance companies to provide coverage for MAT.
- Support adoption of MAT in community settings.
- Expand access to and training for administering naloxone to reduce opioid overdose deaths.
- Ensure that people have access to integrated prevention services, including access to sterile injection equipment from a reliable source, as allowed by local policy.
- Help local jurisdictions to put these effective practices to work in communities where drug addiction is common.
Health care providers can
- Follow best practices for responsible painkiller prescribing to reduce opioid painkiller addiction, the strongest risk factor for heroin addiction:
- Use prescription drug monitoring programs and ask patients about past or current drug and alcohol use prior to considering opioid treatment.
- Prescribe the lowest effective dose and only the quantity needed for each patient.
- Link patients with substance use disorders to effective substance abuse treatment services.
- Support the use of Food and Drug Administration approved MAT options (methadone, buprenorphine, and naltrexone) in patients addicted to prescription opioid painkillers or heroin.
Everyone can
Learn more about the risks of using heroin and other drugs.
- Learn how to recognize and respond to an opioid overdose.
- Get help for substance abuse problems: 1-800-662-HELP.
For more information on MAT and naloxone, visit SAMHSA at: www.samhsa.gov
Issue Details
- Vital Signs Issue details: Demographic and Substance Use Trends Among Heroin Users — United States, 2002–2013, Morbidity and Mortality Weekly Report (MMWR)
- Vital Signs – Today’s Heroin Epidemic [PODCAST – 1:15 minutes]
- Vital Signs – Today’s Heroin Epidemic [PSA – 0:60 seconds]
- Vital Signs: Opioid Painkiller Prescribing: Where You Live Makes a Difference
- Vital Signs: Prescription Painkiller Overdoses: A Growing Epidemic, Especially Among Women
- Vital Signs: Prescription Painkiller Overdoses: Use and Abuse of Methadone as a Painkiller
- Vital Signs: Prescription Painkiller Overdoses in the US
- CDC Prescription Drug Overdose
- Common Elements in Guidelines for Prescribing Opioids for Chronic Pain
- Data Brief: Drug-poisoning Deaths Involving Heroin: United States, 2000–2013
- Press Release: Heroin overdose deaths increased in many states through 2012
- Prescription Drug Overdose Prevention for States
- MedlinePlus – Heroin
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- The White House – Office of National Drug Control Policy: Opioid Abuse in the United States[471KB]
- Providers’ Clinical Support System for Medication Assisted Treatment
- Providers’ Clinical Support System for Opioid Therapies
- Drug Enforcement Administration (DEA): Heroin[145KB]
- National Heroin Threat Assessment Summary[6.02MB]
- National Institute on Drug Abuse
- PDMP Center of Excellence, Brandeis University
- The Dartmouth Atlas of Health Care
- National Alliance for Model State Drug Laws
- Office of the National Coordinator for Health Information Technology (ONC) – Linking PDMPs to Health IT
- National Action Plan for Adverse Drug Event Prevention
- CMS Improvements to Medicare Drug and Health Plans
- U.S. Food and Drug Administration (FDA): Information on Naloxone Auto-Injector
- National Institute on Drug Abuse (NIDA)
- Health Insurance and Mental Health Services
- Page last reviewed: July 7, 2015
- Page last updated: July 7, 2015
- Content source:
Error processing SSI file


 ShareCompartir
ShareCompartir