Pembrolizumab
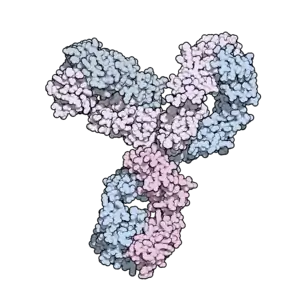 From PDB entry 5dk3 | |
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized (from mouse) |
| Target | PD-1 |
| Names | |
| Trade names | Keytruda |
| Other names | MK-3475, lambrolizumab |
| Clinical data | |
| Drug class | Antineoplastic agents |
| Main uses | Cancer[1] |
| Side effects | Tiredness, musculoskeletal pain, decreased appetite, itchy skin, diarrhea, nausea, rash, fever, cough, difficulty breathing, constipation, abdominal pain[1] |
| Pregnancy category | |
| Routes of use | IV |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a614048 |
| Legal | |
| License data |
|
| Legal status | |
| Chemical and physical data | |
| Formula | C6534H10004N1716O2036S46 |
| Molar mass | 146648.64 g·mol−1 |
Pembrolizumab (formerly lambrolizumab, brand name Keytruda) is a medication used in cancer immunotherapy.[1] This includes to treat melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, cervical cancer, and stomach cancer.[1] It is given by slow injection into a vein.[1]
Common side effects include tiredness, musculoskeletal pain, decreased appetite, itchy skin, diarrhea, nausea, rash, fever, cough, difficulty breathing, constipation, and abdominal pain.[1] Other side effects include liver problems and kidney problems.[1] Use during pregnancy or breastfeeding is not recommended.[4] It is an IgG4 isotype humanized antibody that blocks a protective mechanism of cancer cells and thereby, allows the immune system to destroy them.[1] It targets the programmed cell death protein 1 (PD-1) receptor of lymphocytes.[1]
Pembrolizumab was approved for medical use in the United States in 2014.[1] In 2017, it was approved for any non removable or metastatic solid tumor with certain genetic anomalies (mismatch repair deficiency or microsatellite instability).[5] It is on the World Health Organization's List of Essential Medicines as an alternative for nivolumab.[6] In the United Kingdom the typical dose costs 5,260 pounds every three weeks as of 2020.[7] In the United States this amount costs 8,760 USD.[8]
Medical uses
Pembrolizumab is used via intravenous infusion to treat inoperable or metastatic melanoma, metastatic non-small cell lung cancer (NSCLC) in certain situations, as a first-line treatment for metastatic bladder cancer in people who can't receive cisplatin-based chemotherapy and have high levels of PD-L1, as a second-line treatment for head and neck squamous cell carcinoma (HNSCC), after platinum-based chemotherapy, for the treatment of adult and children with refractory classic Hodgkin's lymphoma (cHL), and recurrent locally advanced or metastatic esophageal squamous cell carcinoma.[9][10][11][12][13][14][15][16]
For NSCLC, pembrolizumab is a first-line treatment if the cancer overexpresses PD-L1, a PD-1 receptor ligand, and the cancer has no mutations in EGFR or in ALK; if chemotherapy has already been administered, then pembrolizumab can be used as a second-line treatment, but if the cancer has EGFR or ALK mutations, agents targeting those mutations should be used first.[9][17] Assessment of PD-L1 expression must be conducted with a validated and approved companion diagnostic.[9][14]
In 2017, the U.S. Food and Drug Administration (FDA) approved pembrolizumab for any unresectable or metastatic solid tumor with certain genetic anomalies (mismatch repair deficiency or microsatellite instability).[5][18] This was the first time the FDA approved a cancer drug based on tumor genetics rather than tissue type or tumor site; therefore, pembrolizumab is a so-called tissue-agnostic drug.
In the European Union, pembrolizumab is indicated for:
- the treatment of advanced (unresectable or metastatic) melanoma in adults as monotherapy.[19]
- the adjuvant treatment of adults with Stage III melanoma and lymph node involvement who have undergone complete resection as monotherapy.[19]
- the first-line treatment of metastatic non-small cell lung carcinoma (NSCLC) in adults whose tumours express PD-L1 with a ≥ 50% tumour proportion score (TPS) with no EGFR or ALK positive tumour mutations as monotherapy.[19]
- the first-line treatment of metastatic non-squamous NSCLC in adults whose tumours have no EGFR or ALK positive mutations in combination with pemetrexed and platinum chemotherapy.[19]
- the first-line treatment of metastatic squamous NSCLC in adults in combination with carboplatin and either paclitaxel or nab-paclitaxel.[19]
- the treatment of locally advanced or metastatic NSCLC in adults whose tumours express PD-L1 with a ≥ 1% TPS and who have received at least one prior chemotherapy regimen. People with EGFR or ALK positive tumour mutations should also have received targeted therapy before receiving Keytruda as monotherapy.[19]
- the treatment of adults with relapsed or refractory classical Hodgkin lymphoma (cHL) who have failed autologous stem cell transplant (ASCT) and brentuximab vedotin (BV), or who are transplant-ineligible and have failed BV as monotherapy.[19]
- the treatment of locally advanced or metastatic urothelial carcinoma in adults who have received prior platinum-containing chemotherapy as monotherapy.[19]
- the treatment of locally advanced or metastatic urothelial carcinoma in adults who are not eligible for cisplatin-containing chemotherapy and whose tumours express PD L1 with a combined positive score (CPS) ≥ 10 as monotherapy.[19]
- the first-line treatment of metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC) in adults whose tumours express PD-L1 with a CPS ≥ 1 as monotherapy or in combination with platinum and 5-fluorouracil (5-FU) chemotherapy.[19]
- the treatment of recurrent or metastatic HNSCC in adults whose tumours express PD-L1 with a ≥ 50% TPS and progressing on or after platinum-containing chemotherapy as monotherapy.[19]
- the first-line treatment of advanced renal cell carcinoma (RCC) in adults in combination with axitinib.[19]
In 2020, the FDA approved pembrolizumab as the first-line treatment for people with unresectable or metastatic microsatellite instability-high (MSI‑H) or mismatch repair deficient (dMMR) colorectal cancer.[20] The approval marks the first immunotherapy approved in the US as a first-line treatment and which is administered to people without also giving chemotherapy.[20]
Dosage
In adults it is often given at a dose of 200 mg every three weeks.[1]
Contraindications
If a person is taking corticosteroids or immunosuppressants, those drugs should be stopped before starting pembrolizumab because they may interfere with pembrolizumab; they may be used after pembrolizumab is started to deal with immune-related adverse effects.[10]
Women of child-bearing age should use contraception when taking pembrolizumab; it should not be administered to pregnant women because animal studies have shown that it can reduce tolerance to the fetus, increasing the risk of miscarriage. It is not known whether pembrolizumab is present in breast milk.[10]
As of 2017, the drug had not been tested in people with active infections (including any HIV, hepatitis B or hepatitis C infection), kidney or liver disease, active CNS metastases, active systemic autoimmune disease, interstitial lung disease, prior pneumonia, and people with a history of severe reaction to another monoclonal antibody.[10]
Side effects
People have had severe infusion-related reactions to pembrolizumab. There have also been severe immune-related adverse effects including lung inflammation (including fatal cases) and inflammation of endocrine organs that caused inflammation of the pituitary gland, of the thyroid (causing both hypothyroidism and hyperthyroidism in different people), and pancreatitis that caused Type 1 diabetes and diabetic ketoacidosis; some people have had to go on lifelong hormone therapy as a result (e.g. insulin therapy or thyroid hormones). People have also had colon inflammation, liver inflammation, kidney inflammation due to the drug.[10][21]
The common adverse reactions have been fatigue (24%), rash (19%), itchiness (pruritus) (17%), diarrhea (12%), nausea (11%) and joint pain (arthralgia) (10%).[10]
Other adverse effects occurring in between 1% and 10% of people taking pembrolizumab have included anemia, decreased appetite, headache, dizziness, distortion of the sense of taste, dry eye, high blood pressure, abdominal pain, constipation, dry mouth, severe skin reactions, vitiligo, various kinds of acne, dry skin, eczema, muscle pain, pain in a limb, arthritis, weakness, edema, fever, chills, myasthenia gravis, and flu-like symptoms.[10]
.jpg.webp) Dermatitis induced by pembrolizumab
Dermatitis induced by pembrolizumab.jpg.webp) Bullous pemphigoid induced by pembrolizumab
Bullous pemphigoid induced by pembrolizumab.jpg.webp) Bullous pemphigoid induced by pembrolizumab
Bullous pemphigoid induced by pembrolizumab.jpg.webp) Bullous pemphigoid induced by pembrolizumab
Bullous pemphigoid induced by pembrolizumab
Mechanism of action
Pembrolizumab is a therapeutic antibody that binds to and blocks PD-1 located on lymphocytes. This receptor is generally responsible for preventing the immune system from attacking the body's own tissues; it is a so-called immune checkpoint.[22][23] Many cancers make proteins that bind to PD-1, thus shutting down the ability of the body to kill the cancer on its own.[14][22] Inhibiting PD-1 on the lymphocytes prevents this, allowing the immune system to target and destroy cancer cells;[24] this same mechanism also allows the immune system to attack the body itself, and checkpoint inhibitors like pembrolizumab have immune-dysfunction side effects as a result.[23]
Tumors that have mutations that cause impaired DNA mismatch repair, which often results in microsatellite instability, tend to generate many mutated proteins that could serve as tumor antigens; pembrolizumab appears to facilitate clearance of any such tumor by the immune system, by preventing the self-checkpoint system from blocking the clearance.[14][25]
Pharmacology
Since pembrolizumab is cleared from the circulation through non-specific catabolism, no metabolic drug interactions are expected and no studies were done on routes of elimination.[10] The systemic clearance [rate] is about 0.2 L/day and the terminal half-life is about 25 days.[10]
Chemistry and manufacturing
Pembrolizumab is an immunoglobulin G4, with a variable region against the human PD-1 receptor, a humanized mouse monoclonal [228-L-proline(H10-S>P)]γ4 heavy chain (134-218') disulfide and a humanized mouse monoclonal κ light chain dimer (226-226:229-229)-bisdisulfide.[26]
It is recombinantly manufactured in Chinese hamster ovary (CHO) cells.[27][19]
History
Pembrolizumab was invented by scientists Gregory Carven, Hans van Eenennaam and John Dulos at Organon after which they worked with Medical Research Council Technology (which became LifeArc) starting in 2006, to humanize the antibody; Schering-Plough acquired Organon in 2007, and Merck & Co. acquired Schering-Plough two years later.[28] Carven, van Eenennaam and Dulos were recognized as Inventors of the Year by the Intellectual Property Owners Education Foundation in 2016.[29]
The development program for pembrolizumab was seen as high priority at Organon, but low at Schering and later Merck. In early 2010, Merck terminated development and began preparing to out-license it.[30] Later, in 2010, scientists from Bristol Myers Squibb published a paper in The New England Journal of Medicine showing that their checkpoint inhibitor, ipilimumab (Yervoy) had shown strong promise in treating metastatic melanoma[31] and that a second Bristol-Myers Squibb checkpoint inhibitor, nivolumab, (Opdivo) was also promising.[30] Merck at that time had little commitment or expertise in either oncology or immunotherapy, but understood the opportunity and reacted strongly, reactivating the program and filing its IND by the end of 2010.[30] As one example, Martin Huber was one of the few senior people at Merck with strong experience in lung cancer drug development, but had been promoted to senior management and was no longer involved in product development. He stepped down from his role to lead clinical development of pembrolizumab for lung cancer.[30]
Scientists at the company argued for developing a companion diagnostic and limiting testing of the drug only to patients with biomarkers showing they were likely to respond, and received agreement from management. Some people, including shareholders and analysts, criticized this decision as it limited the potential market size for the drug, while others argued it increased the chances of proving the drug would work and would make clinical trials faster. (The trials would need fewer patients because of the likelihood of greater effect size.) Moving quickly and reducing the risk of failure was essential for catching up with Bristol-Myers Squibb, which had an approximate five year lead over Merck.[30] The phase I study started in early 2011, and Eric Rubin, who was running the melanoma trial, argued for and was able to win expansion of the trial until it reached around 1300 people. This was the largest Phase I study ever run in oncology, with the patients roughly divided between melanoma and lung cancer.[30]
In 2013, Merck quietly applied for and won a breakthrough therapy designation for the drug. This regulatory pathway was new at the time and not well understood. One of its advantages is that the US FDA holds more frequent meetings with drug developers, reducing the risk of developers making mistakes or misunderstandings arising between regulators' expectations and what the developers want to do. This was Merck's first use of the designation and the reduction in regulatory risk was one of the reasons management was willing to put company resources into development.[30]
In 2013, the United States Adopted Name (USAN) name was changed from lambrolizumab to pembrolizumab.[26] In that year clinical trial results in advanced melanoma were published in The New England Journal of Medicine.[32] This was part of the large Phase I NCT01295827 trial.[33]
On 4 September 2014, the US Food and Drug Administration (FDA) approved pembrolizumab under the Fast Track Development Program.[34] It is approved for use following treatment with ipilimumab, or after treatment with ipilimumab and a BRAF inhibitor in advanced melanoma patients who carry a BRAF mutation.[35]
As of 2015, the only PD-1/PD-L1 targeting drugs on the market were pembrolizumab and nivolumab, with clinical developments in the class of drugs receiving coverage in The New York Times.[36]
By April 2016, Merck applied for approval to market the drug in Japan and signed an agreement with Taiho Pharmaceutical to co-promote it there.[37]
In July 2015, pembrolizumab received marketing approval in Europe.[10][38][19]
On 2 October 2015, the US FDA approved pembrolizumab for the treatment of metastatic non-small cell lung cancer (NSCLC) in patients whose tumors express PD-L1 and who have failed treatment with other chemotherapeutic agents.[39]
In July 2016, the US FDA accepted for priority review an application for recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) after a platinum-based chemotherapy.[40] They granted accelerated approval to pembrolizumab as a treatment for patients with recurrent or metastatic (HNSCC) ("regardless of PD-L1 staining") following progression on a platinum-based chemotherapy, based on objective response rates (ORR) in the Phase Ib KEYNOTE-012 study in August of the same year.[41][42] Full approval depended on the results of the Phase III KEYNOTE-040 study (NCT02252042), which ran until Jan 2017.[42]
In May 2017, pembrolizumab received an accelerated approval from the US FDA for use in any unresectable or metastatic solid tumor with DNA mismatch repair deficiencies or a microsatellite instability-high state (or, in the case of colon cancer, tumors that have progressed following chemotherapy).[43] This approval marked the first instance in which the FDA approved marketing of a drug based only on the presence of a genetic mutation, with no limitation on the site of the cancer or the kind of tissue in which it originated.[43][18][25][44] The approval was based on a clinical trial of 149 patients with microsatellite instability-high or mismatch repair deficient cancers who enrolled on one of five single-arm trials. Ninety patients had colorectal cancer, and 59 patients had one of 14 other cancer types. The objective response rate for all patients was 39.6%. Response rates were similar across all cancer types, including 36% in colorectal cancer and 46% across the other tumor types. Notably, there were 11 complete responses, with the remainder partial responses. Responses lasted for at least six months in 78% of responders.[25] Because the clinical trial was fairly small, Merck is obligated to conduct further post-marketing studies to ensure that the results are valid.[45] Pembrolizumab was granted orphan drug designation for SCLC in October 2017.[46]
In June 2018, the US FDA approved pembrolizumab for use in both advanced cervical cancer for PD-L1 positive patients[47] and for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after two or more prior lines of therapy.[48]
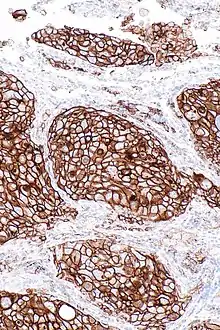
In August 2018, the US FDA updated the prescribing information for pembrolizumab atezolizumab to require the use of an FDA-approved companion diagnostic test to determine PD-L1 levels in tumor tissue from patients with locally advanced or metastatic urothelial cancer who are cisplatin-ineligible.[49] On 16 August 2018, the FDA approved the Dako PD-L1 IHC 22C3 PharmDx Assay (Dako North America, Inc.) as a companion diagnostic to select patients with locally advanced or metastatic urothelial carcinoma who are cisplatin-ineligible for treatment with pembrolizumab.[49] The 22C3 assay determines PD-L1 expression by using a combined positive score (CPS) assessing PD-L1 staining in tumor and immune cells.[49] As of August 2018, pembrolizumab is indicated for the treatment of those with locally advanced or metastatic urothelial carcinoma who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 [Combined Positive Score (CPS) ≥ 10] as determined by an FDA-approved test, or in patients who are not eligible for any platinum-containing chemotherapy regardless of PD-L1 status.[49]
In November 2018, the US FDA granted accelerated approval to pembrolizumab for those with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib.[50]
In February 2019, the US FDA approved pembrolizumab for the adjuvant treatment of people with melanoma with involvement of lymph node(s) following complete resection.[51] The FDA granted the application orphan drug designation.[51]
In June 2019, the US FDA granted accelerated approval to pembrolizumab for those with metastatic small cell lung cancer (SCLC) with disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy,[46] and the FDA approved pembrolizumab for the first-line treatment of people with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).[52] Pembrolizumab was approved for use in combination with platinum and fluorouracil (FU) for all patients and as a single agent for patients whose tumors express PD‑L1 (Combined Positive Score [CPS] ≥1) as determined by an FDA‑approved test.[52] The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.[52]
In July 2019, the FDA approved pembrolizumab for people with recurrent, locally advanced or metastatic, squamous cell carcinoma of the esophagus (ESCC) whose tumors express PD-L1 (Combined Positive Score [CPS] ≥10), as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.[15] The FDA also approved a new use for the PD-L1 IHC 22C3 pharmDx kit as a companion diagnostic device for selecting people for the above indication.[15]
In June 2020, the US FDA approved pembrolizumab as monotherapy for the treatment of adult and children with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.[53]
Society and culture
Pembrolizumab was priced at $150,000 per year when it launched (late 2014).[54]
Research
In 2015, Merck reported results in 13 cancer types; much attention was given to early results in head and neck cancer.[14][55][56]
As of May 2016, pembrolizumab was in Phase IB clinical trials for triple-negative breast cancer (TNBC), gastric cancer, urothelial cancer, and head and neck cancer (all under the "Keynote-012" trial) and in Phase II trial for TNBC (the "Keynote-086" trial).[57] At ASCO, in June 2016, Merck reported that the clinical development program was directed to around 30 cancers and that it was running over 270 clinical trials (around 100 in combination with other treatments) and had four registration-enabling studies in process.[58]
Results of a Phase III clinical trial in triple-negative breast cancer were reported in Annals of Oncology in October 2019.[59]
Results of a Phase II clinical trial in Merkel-cell carcinoma were reported in The New England Journal of Medicine in June 2016.[60]
Results of a clinical trial in people with untreatable metastases arising from various solid tumors were published in Science in 2017.[61]
A clinical Phase III trial in combination with epacadostat, an Indoleamine 2,3-dioxygenase (IDO1) inhibitor to treat melanoma was completed in 2019.[14][62]
References
- 1 2 3 4 5 6 7 8 9 10 11 "Pembrolizumab Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 14 June 2020. Retrieved 15 July 2019.
- 1 2 "Pembrolizumab (Keytruda) Use During Pregnancy". Drugs.com. 24 September 2019. Archived from the original on 14 June 2020. Retrieved 10 January 2020.
- ↑ "Keytruda 50 mg powder for concentrate for solution for infusion - Summary of Product Characteristics (SmPC)". (emc). 7 April 2020. Archived from the original on 13 December 2017. Retrieved 30 April 2020.
- ↑ "Pembrolizumab (Keytruda) Use During Pregnancy". Drugs.com. Archived from the original on 14 June 2020. Retrieved 19 October 2020.
- 1 2 Syn, Nicholas L; Teng, Michele W L; Mok, Tony S K; Soo, Ross A (2017). "De-novo and acquired resistance to immune checkpoint targeting". The Lancet Oncology. 18 (12): e731–e741. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ BNF 79. London: Pharmaceutical Press. March 2020. p. 909. ISBN 978-0857113658.
- ↑ Huang, M; Lou, Y; Pellissier, J; Burke, T; Liu, FX; Xu, R; Velcheti, V (August 2017). "Cost Effectiveness of Pembrolizumab vs. Standard-of-Care Chemotherapy as First-Line Treatment for Metastatic NSCLC that Expresses High Levels of PD-L1 in the United States". PharmacoEconomics. 35 (8): 831–844. doi:10.1007/s40273-017-0527-z. PMID 28620848.
- 1 2 3 "Keytruda- pembrolizumab injection, powder, lyophilized, for solution Keytruda- pembrolizumab injection, solution". DailyMed. 17 September 2019. Archived from the original on 17 June 2020. Retrieved 10 January 2020.
- 1 2 3 4 5 6 7 8 9 10 "Keytruda 50 mg powder for concentrate for solution for infusion - Summary of Product Characteristics (SmPC)". (emc). 25 November 2019. Archived from the original on 13 December 2017. Retrieved 10 January 2020.
- ↑ Redman, Jason M.; Gibney, Geoffrey T.; Atkins, Michael B. (6 February 2016). "Advances in immunotherapy for melanoma". BMC Medicine. 14 (1): 20. doi:10.1186/s12916-016-0571-0. PMC 4744430. PMID 26850630.
- ↑ Fuereder, Thorsten (20 June 2016). "Immunotherapy for head and neck squamous cell carcinoma". Memo - Magazine of European Medical Oncology. 9 (2): 66–69. doi:10.1007/s12254-016-0270-8. PMC 4923082. PMID 27429658.
- ↑ "Pembrolizumab (Keytruda) for classical Hodgkin lymphoma". U.S. Food and Drug Administration (FDA). 14 March 2017. Archived from the original on 12 January 2020. Retrieved 12 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 4 5 6 Syn, Nicholas L; Teng, Michele W L; Mok, Tony S K; Soo, Ross A (2017). "De-novo and acquired resistance to immune checkpoint targeting". The Lancet Oncology. 18 (12): e731–e741. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- 1 2 3 "FDA approves pembrolizumab for advanced esophageal squamous cell cancer". U.S. Food and Drug Administration (FDA) (Press release). 30 July 2019. Archived from the original on 12 January 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Checkpoint Inhibitor Use Changed for Bladder Cancer". National Cancer Institute. 26 July 2018. Archived from the original on 18 March 2021. Retrieved 12 November 2019.
- ↑ Chen, Hongbin; Vachhani, Pankit (September 2016). "Spotlight on pembrolizumab in non-small cell lung cancer: the evidence to date". OncoTargets and Therapy. 9: 5855–5866. doi:10.2147/ott.s97746. PMC 5045223. PMID 27713639.
- 1 2 "FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication". U.S. Food and Drug Administration (FDA) (Press release). 23 May 2017. Archived from the original on 23 April 2019. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Keytruda EPAR". European Medicines Agency (EMA). Archived from the original on 24 May 2020. Retrieved 30 April 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- 1 2 "FDA Approves First-Line Immunotherapy for Patients with MSI-H/dMMR Metastatic Colorectal Cancer". U.S. Food and Drug Administration (FDA) (Press release). 29 June 2020. Archived from the original on 29 June 2020. Retrieved 29 June 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Linardou, Helena; Gogas, Helen (July 2016). "Toxicity management of immunotherapy for patients with metastatic melanoma". Annals of Translational Medicine. 4 (14): 272. doi:10.21037/atm.2016.07.10. PMC 4971373. PMID 27563659.
- 1 2 Buqué A, Bloy N, Aranda F, Castoldi F, Eggermont A, Cremer I, Fridman WH, Fucikova J, Galon J, Marabelle A, Spisek R, Tartour E, Zitvogel L, Kroemer G, Galluzzi L (July 2010). "The PD-1 pathway in tolerance and autoimmunity". Immunological Reviews. 236: 219–42. doi:10.1111/j.1600-065X.2010.00923.x. PMC 2919275. PMID 20636820.
- 1 2 Buqué, Aitziber (April 2015). "Trial Watch: Immunomodulatory monoclonal antibodies for oncological indications". Oncoimmunology. 4 (4): e1008814. doi:10.1080/2162402x.2015.1008814. PMC 4485728. PMID 26137403.
- ↑ Pardoll DM (March 2012). "The blockade of immune checkpoints in cancer immunotherapy". Nature Reviews Cancer. 12 (4): 252–64. doi:10.1038/nrc3239. PMC 4856023. PMID 22437870.
- 1 2 3 Bala S, Nair A, Lemery S, et al. (30 May 2017). "FDA D.I.S.C.O.: First Tissue/Site Agnostic Approval Transcript". U.S. Food and Drug Administration (FDA). Archived from the original on 12 January 2020. Retrieved 12 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "Statement on a Nonproprietary Name Adopted by the USAN Council" (PDF). AMA ASSN. 27 November 2013. Archived (PDF) from the original on 26 October 2020. Retrieved 5 November 2016.
- ↑ "Assessment report: Keytruda. Procedure No. EMEA/H/C/003820/0000" (PDF). European Medicines Agency (EMA). 21 May 2015. Archived (PDF) from the original on 14 June 2018. Retrieved 5 November 2016.
- ↑ "Unlocking Checkpoint Inhibition". Translational Scientist. 9 August 2016. Archived from the original on 5 November 2018. Retrieved 5 November 2016.
- ↑ "Inventors of the Year". Inventors Digest. Archived from the original on 28 October 2020. Retrieved 8 May 2017.
- 1 2 3 4 5 6 7 Shaywitz, David (26 July 2017). "The Startling History Behind Merck's New Cancer Blockbuster". Forbes. Archived from the original on 26 July 2017. Retrieved 26 July 2017.
- ↑ Hodi FS, O'Day SJ, McDermott DF, et al. (August 2010). "Improved survival with ipilimumab in patients with metastatic melanoma". New England Journal of Medicine. 363 (8): 711–723. doi:10.1056/nejmoa1003466. ISSN 0028-4793. PMC 3549297. PMID 20525992.
- ↑ Hamid O, Robert C, Daud A, et al. (July 2013). "Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma". New England Journal of Medicine. 369 (2): 134–44. doi:10.1056/nejmoa1305133. PMC 4126516. PMID 23724846.
- ↑ Clinical trial number NCT01295827 for "Study of Pembrolizumab (MK-3475) in Participants With Progressive Locally Advanced or Metastatic Carcinoma, Melanoma, or Non-small Cell Lung Carcinoma (P07990/MK-3475-001/KEYNOTE-001) (KEYNOTE-001)" at ClinicalTrials.gov
- ↑ "FDA approves Keytruda for advanced melanoma" (Press release). U.S. Food and Drug Administration (FDA). 4 September 2014. Archived from the original on 27 December 2015. Retrieved 24 December 2015.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "FDA Approves Anti-PD-1 Drug for Advanced Melanoma". cancernetwork.com. Archived from the original on 10 January 2016. Retrieved 7 September 2014.
- ↑ Pollack, Andrew (29 May 2015). "New Class of Drugs Shows More Promise in Treating Cancer". The New York Times. Archived from the original on 29 May 2015. Retrieved 30 May 2015.
- ↑ "Merck & Co and Taiho to co-promote cancer immunotherapy pembrolizumab in Japan". The Pharma Letter. 13 April 2016. Archived from the original on 18 April 2018. Retrieved 10 November 2016.
- ↑ "Keytruda index page at EMA". European Medicines Agency (EMA). Archived from the original on 20 June 2018. Retrieved 10 November 2016.
- ↑ "FDA approves Keytruda for advanced non-small cell lung cancer" (Press release). U.S. Food and Drug Administration (FDA). 2 October 2015. Archived from the original on 8 November 2015. Retrieved 12 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Potential Biomarkers Identified for Pembrolizumab in Head and Neck Cancer. July 2016
- ↑ "pembrolizumab (Keytruda)". U.S. Food and Drug Administration (FDA) (Press release). 5 August 2016. Archived from the original on 16 December 2019. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "FDA Approves Pembrolizumab for Head and Neck Cancer. Aug 2016". Archived from the original on 7 August 2016. Retrieved 6 August 2016.
- 1 2 "FDA approves first cancer treatment for any solid tumor with a specific genetic feature". U.S. Food and Drug Administration (FDA) (Press release). 23 May 2017. Archived from the original on 12 January 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Ledford, Heidi (24 May 2017). "Tissue-independent cancer drug gets fast-track approval from US regulator". Nature. doi:10.1038/nature.2017.22054. Archived from the original on 12 November 2020. Retrieved 17 June 2017.
- ↑ "Accelerated approval notice: BLA 125514/S-14" (PDF). U.S. Food and Drug Administration (FDA). 23 May 2017. Archived (PDF) from the original on 28 August 2021. Retrieved 17 June 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "FDA approves pembrolizumab for metastatic small cell lung cancer". U.S. Food and Drug Administration (FDA) (Press release). 17 June 2019. Archived from the original on 6 April 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "FDA Approves Pembrolizumab for Advanced Cervical Cancer with Disease Progression During or After Chemotherapy". ASCO. 12 June 2018. Archived from the original on 12 January 2020. Retrieved 13 June 2018.
- ↑ "FDA approves pembrolizumab for treatment of relapsed or refractory PMBCL". U.S. Food and Drug Administration (FDA) (Press release). 13 June 2018. Archived from the original on 12 January 2020. Retrieved 16 June 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 4 "FDA updates prescribing information for Keytruda and Tecentriq". U.S. Food and Drug Administration (Press release). 16 August 2018. Archived from the original on 22 December 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "FDA grants accelerated approval to pembrolizumab for hepatocellular carcinoma". U.S. Food and Drug Administration (FDA) (Press release). 9 November 2018. Archived from the original on 12 January 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 "FDA approves pembrolizumab for adjuvant treatment of melanoma". U.S. Food and Drug Administration (FDA) (Press release). 15 February 2019. Archived from the original on 12 January 2020. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 "FDA approves pembrolizumab for first-line treatment of head and neck squamous cell carcinoma". U.S. Food and Drug Administration (FDA) (Press release). 10 June 2019. Archived from the original on 16 December 2019. Retrieved 10 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Research, Center for Drug Evaluation and (17 June 2020). "FDA approves pembrolizumab for adults and children with TMB-H solid tumors". FDA. Archived from the original on 15 March 2021. Retrieved 19 June 2020.
- ↑ "Amgen slaps record-breaking $178K price on rare leukemia drug Blincyto". Archived from the original on 1 April 2016. Retrieved 29 April 2016.
- ↑ Timmerman, Luke (2 June 2015). "ASCO Wrapup: Immunotherapy Shines, Hope For Brain Tumors, & The Great Cancer Drug Price Debate". Forbes. Archived from the original on 8 November 2020. Retrieved 8 September 2017.
- ↑ Adams, Katherine T. (24 July 2015). "Cancer Immunotherapies--and Their Cost--Take Center Stage at ASCO's 2015 Annual Meeting". Managed Care Magazine Online. Archived from the original on 13 December 2017. Retrieved 5 November 2016.
- ↑ Jenkins, Kristin (5 May 2016). "Keytruda Impresses in Triple-Negative Breast Cancer". MedPage Today. Archived from the original on 19 December 2016. Retrieved 14 May 2016.
- ↑ "Merck & Co updates Keytruda findings at ASCO". The Pharma Letter. 10 June 2016. Archived from the original on 5 November 2016. Retrieved 5 November 2016.
- ↑ Schmid P, Cortés J, Dent R, et al. (2019). "KEYNOTE-522: Phase III study of pembrolizumab (pembro) + chemotherapy (chemo) vs placebo (pbo) + chemo as neoadjuvant treatment, followed by pembro vs pbo as adjuvant treatment for early triple-negative breast cancer (TNBC)". Annals of Oncology. 30 (5): v853–v854. doi:10.1093/annonc/mdz394.003.
- ↑ Nghiem (2016). "PD-1 Blockade with Pembrolizumab in Advanced Merkel-Cell Carcinoma". N. Engl. J. Med. 374 (26): 2542–2552. doi:10.1056/NEJMoa1603702. PMC 4927341. PMID 27093365.
- ↑ Le DT, Durham JN, Smith KN, et al. (8 June 2017). "Mismatch-repair deficiency predicts response of solid tumors to PD-1 blockade". Science. 357 (6349): 409–413. Bibcode:2017Sci...357..409L. doi:10.1126/science.aan6733. PMC 5576142. PMID 28596308.
- ↑ Clinical trial number NCT02752074 for "A Phase 3 Study of Pembrolizumab + Epacadostat or Placebo in Subjects With Unresectable or Metastatic Melanoma (Keynote-252 / ECHO-301)" at ClinicalTrials.gov
 This article incorporates public domain material from the United States Department of Health and Human Services document: Bala S, Nair A, Lemery S, Marcus L, Goldberg KB, Pazdur R. "FDA D.I.S.C.O.: First Tissue/Site Agnostic Approval Transcript".
This article incorporates public domain material from the United States Department of Health and Human Services document: Bala S, Nair A, Lemery S, Marcus L, Goldberg KB, Pazdur R. "FDA D.I.S.C.O.: First Tissue/Site Agnostic Approval Transcript".{{cite web}}: CS1 maint: multiple names: authors list (link)
External links
| External sites: |
|
|---|---|
| Identifiers: |