Tamoxifen
 | |
 | |
| Names | |
|---|---|
| Trade names | Nolvadex, Genox, Tamifen, others[1] |
| Other names | TMX; ICI-46474 |
IUPAC name
| |
| Clinical data | |
| Drug class | Selective estrogen receptor modulator |
| Pregnancy category | |
| Routes of use | By mouth |
| Defined daily dose | 20 mg [3] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682414 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | ~100%[4][5] |
| Protein binding | >99% (albumin)[4][6] |
| Metabolism | Liver (CYP3A4, CYP2C9, CYP2D6)[4][7][8] |
| Metabolites | • Afimoxifene[8] • Endoxifen[8] • Norendoxifen[8] |
| Elimination half-life | 5–7 days[4][8] |
| Excretion | Feces: 65% Urine: 9% |
| Chemical and physical data | |
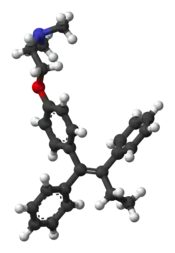
| Formula | C26H29NO |
| Molar mass | 371.515 g/mol 563.638 g/mol (citrate salt) g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Tamoxifen, sold under the brand name Nolvadex among others, is a medication that is used to prevent breast cancer in women and treat breast cancer in women and men.[9] It is also being studied for other types of cancer.[9] It has been used for Albright syndrome.[10] Tamoxifen is typically taken daily by mouth for five years for breast cancer.[10]
Serious side effects include a small increased risk of uterine cancer, stroke, vision problems, and pulmonary embolism.[10] Common side effects include irregular periods, weight loss, and hot flashes.[10] It may cause harm to the baby if taken during pregnancy or breastfeeding.[10] It is a selective estrogen-receptor modulator (SERM) and works by decreasing the growth of breast cancer cells.[10][11] It is a member of the triphenylethylene group of compounds.[12]
Tamoxifen was initially made in 1962, by chemist Dora Richardson.[13][14] It is on the World Health Organization's List of Essential Medicines.[15] Tamoxifen is available as a generic medication.[10] The wholesale price in the developing world is about US$0.07–0.23 per day.[16] In the United States, it costs about $1 per day.[10] In 2017, it was the 251st most commonly prescribed medication in the United States, with more than one million prescriptions.[17][18]
Medical uses
Breast cancer
Tamoxifen is used for the treatment of both early and advanced estrogen receptor-positive (ER-positive or ER+) breast cancer in pre- and post-menopausal women.[19] Additionally, it is the most common hormone treatment for male breast cancer.[20] It is also approved by the FDA for the prevention of breast cancer in women at high risk of developing the disease.[21] It has been further approved for the reduction of contralateral (in the opposite breast) cancer. The use of tamoxifen is recommended for 10 years.[22]
In 2006, the large STAR clinical study concluded that raloxifene is also effective in reducing the incidence of breast cancer. Updated results after an average of 6.75 years of follow up found that raloxifene retains 76% of tamoxifen's effectiveness in preventing invasive breast cancer, with 45% fewer uterine cancers and 25% fewer blood clots in women taking raloxifene than in women taking tamoxifen.[23][24][25]
Infertility
Tamoxifen is used for ovulation induction to treat infertility in women with anovulatory disorders. It is given at days three to seven of a woman's cycle.[26]
Tamoxifen improves fertility in males with infertility by disinhibiting the hypothalamic–pituitary–gonadal axis (HPG axis) via ER antagonism and thereby increasing the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) and increasing testicular testosterone production.[27]
Gynecomastia
Tamoxifen is used to prevent and treat gynecomastia.[28][29] It is taken as a preventative measure in small doses, or used at the onset of any symptoms such as nipple soreness or sensitivity. Other medications are taken for similar purposes such as clomifene and the anti-aromatase drugs which are used in order to try to avoid the hormone-related adverse effects.
| Follow-up timepoint | Tamoxifen dosage | |||||
|---|---|---|---|---|---|---|
| Placebo | 1 mg/day | 2.5 mg/day | 5 mg/day | 10 mg/day | 20 mg/day | |
| 0 months | – | |||||
| 6 months | 98% | 90% | 80% | 54% | 22% | 10% |
| 12 months | 99% | 95% | 84% | 56% | 38% | 19% |
| Notes: Prevention of breast symptoms—specifically gynecomastia and breast pain—induced by 150 mg/day bicalutamide monotherapy with tamoxifen in 282 men with prostate cancer. Bicalutamide and tamoxifen were initiated at the same time (0 months). Sources: [30][31] | ||||||
Early puberty
Tamoxifen is useful in the treatment of peripheral precocious puberty, for instance due to McCune–Albright syndrome, in both girls and boys.[32][33][34] It has been found to decrease growth velocity and the rate of bone maturation in girls with precocious puberty, and hence to improve final height in these individuals.[32][33]
Dosage

The defined daily dose is 20 mg (by mouth).[3] While the typical dose in adults is 20 mg once per day, 40 mg once per day may be used.[10]
Tamoxifen is available as a tablet or oral solution.[35][36]
Contraindications
Tamoxifen has a number of contraindications, including known hypersensitivity to tamoxifen or other ingredients, individuals taking concomitant coumarin-type anticoagulant therapy, and women with a history of venous thromboembolism (deep vein thrombosis or pulmonary embolism).[7]
Side effects
A report in September 2009 from Health and Human Services' Agency for Healthcare Research and Quality suggests that tamoxifen, raloxifene, and tibolone used to treat breast cancer significantly reduce invasive breast cancer in midlife and older women, but also increase the risk of adverse side effects.[37]
Some cases of lower-limb lymphedema have been associated with the use of tamoxifen, due to the blood clots and deep vein thrombosis (DVT) that can be caused by this medication. Resolution of the blood clots or DVT is needed before lymphedema treatment can be initiated.
Bone
A beneficial side effect of tamoxifen is that it prevents bone loss by acting as an ER agonist (i.e., mimicking the effects of estrogen) in this cell type. Therefore, by inhibiting osteoclasts, it prevents osteoporosis.[38][39] When tamoxifen was launched as a drug, it was thought that tamoxifen would act as an ER antagonist in all tissue, including bone, and therefore it was feared that it would contribute to osteoporosis. It was therefore very surprising that the opposite effect was observed clinically. Hence tamoxifen's tissue selective action directly led to the formulation of the concept of SERMs.[40] In contrast tamoxifen appears to be associated with bone loss in premenopausal women who continue to menstruate after adjuvant chemotherapy.[41]
Endometrial cancer
Tamoxifen is a selective estrogen receptor modulator (SERM).[42] Even though it is an antagonist in breast tissue it acts as partial agonist on the endometrium and has been linked to endometrial cancer in some women. Therefore, endometrial changes, including cancer, are among tamoxifen's side effects.[43] With time, risk of endometrial cancer may be doubled to quadrupled, which is a reason tamoxifen is typically only used for five years.[44]
The American Cancer Society lists tamoxifen as a known carcinogen, stating that it increases the risk of some types of uterine cancer while lowering the risk of breast cancer recurrence.[45] The ACS states that its use should not be avoided in cases where the risk of breast cancer recurrence without the drug is higher than the risk of developing uterine cancer with the drug.
Cardiovascular and metabolic
Tamoxifen treatment of postmenopausal women is associated with beneficial effects on serum lipid profiles. However, long-term data from clinical trials have failed to demonstrate a cardioprotective effect.[46] For some women, tamoxifen can cause a rapid increase in triglyceride concentration in the blood. In addition, there is an increased risk of thromboembolism especially during and immediately after major surgery or periods of immobility.[47] Use of tamoxifen has been shown to slightly increase risk of deep vein thrombosis, pulmonary embolism, and stroke.[48] Tamoxifen is also a cause of fatty liver, otherwise known as steatorrhoeic hepatosis or steatosis hepatis.[49]
Central nervous system
Tamoxifen-treated breast cancer patients show evidence of reduced cognition,[50] and semantic memory scores.[51] However, memory impairment in patients treated with tamoxifen was less severe compared with those treated with anastrozole (an aromatase inhibitor).[52]
A significant number of tamoxifen-treated breast cancer patients experience a reduction of libido.[53][54]
Liver toxicity
Tamoxifen has been associated with a number of cases of liver toxicity.[55] Several different varieties of hepatotoxicity have been reported.[55]
Weight gain
Weight gain is a commonly reported side effect,[56] but studies have not been able to find significant evidence of a correlation.[57]
Overdose
Acute overdose of tamoxifen has not been reported in humans.[7] In dose-ranging studies, tamoxifen was administered at very high doses in women (e.g., 300 mg/m2) and was found to produce acute neurotoxicity including tremor, hyperreflexia, unsteady gait, and dizziness.[7] These symptoms occurred within three to five days of therapy and disappeared within two to five days of discontinuation of therapy.[7] No indications of permanent neurotoxicity were observed.[7] QT prolongation was also observed with very high doses of tamoxifen.[7] There is no specific antidote for overdose of tamoxifen.[7] Instead, treatment should be based on symptoms.[7]
Interactions
Patients with variant forms of the gene CYP2D6 (also called simply 2D6) may not receive full benefit from tamoxifen because of too slow metabolism of the tamoxifen prodrug into its active metabolites.[58][59] On 18 October 2006, the Subcommittee for Clinical Pharmacology recommended relabeling tamoxifen to include information about this gene in the package insert.[60]
Certain CYP2D6 variations in breast cancer patients lead to a worse clinical outcome for tamoxifen treatment.[61] Genotyping therefore has the potential for identification of women who have these CYP2D6 phenotypes and for whom the use of tamoxifen is associated with poor outcomes.
Recent studies suggest that taking the selective serotonin reuptake inhibitors (SSRIs) antidepressants paroxetine (Paxil), fluoxetine (Prozac), and sertraline (Zoloft) can decrease the effectiveness of tamoxifen, as these drugs compete for the CYP2D6 enzyme which is needed to metabolize tamoxifen into its active forms.[62] A U.S. study presented at the American Society of Clinical Oncology's annual meeting in 2009 found that after two years, 7.5% of women who took only tamoxifen had a recurrence, compared with 16% who took either paroxetine, fluoxetine or sertraline, drugs considered to be the most potent CYP2D6 inhibitors. That difference translates to a 120% increase in the risk of breast cancer recurrence. Patients taking the SSRIs; Celexa (citalopram), Lexapro (escitalopram), and Luvox (fluvoxamine), did not have an increased risk of recurrence, due to their lack of competitive metabolism for the CYP2D6 enzyme.[63] A newer study demonstrated a clearer and stronger effect from paroxetine in causing the worst outcomes. Patients treated with both paroxetine and tamoxifen have a 67% increased risk of death from breast cancer, from 24% to 91%, depending on the duration of coadministration.[64]
Recent research has shown that 7–10% of women with breast cancer may not receive the full medical benefit from taking tamoxifen due to their genetic make-up. DNA Drug Safety Testing can examine DNA variations in the CYP2D6 and other important drug processing pathways. More than 20% of all clinically used medications are metabolized by CYP2D6 and knowing the CYP2D6 status of a person can help the doctor with the future selection of medications.[65] Other molecular biomarkers may also be used to select appropriate patients likely to benefit from tamoxifen.[66]
Tamoxifen interacts with certain other antiestrogens.[4] The aromatase inhibitor aminoglutethimide induces the metabolism of tamoxifen.[4] Conversely, the aromatase inhibitor letrozole does not affect the metabolism of tamoxifen.[4] However, tamoxifen induces the metabolism of letrozole and significantly reduces its concentrations.[4]
Pharmacology
Pharmacodynamics
Selective estrogen receptor modulator activity
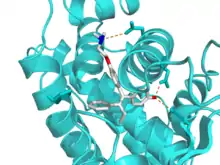
Tamoxifen acts as a selective estrogen receptor modulator (SERM), or as a partial agonist of the estrogen receptors (ERs). It has mixed estrogenic and antiestrogenic activity, with its profile of effects differing by tissue. For instance, tamoxifen has predominantly antiestrogenic effects in the breasts but predominantly estrogenic effects in the uterus and liver. In breast tissue, tamoxifen acts as an ER antagonist so that transcription of estrogen-responsive genes is inhibited.[68]
Tamoxifen has relatively little affinity for the ERs itself and instead acts as a prodrug of active metabolites such as afimoxifene (4-hydroxytamoxifen; 4-OHT) and endoxifen (N-desmethyl-4-hydroxytamoxifen). These metabolites have approximately 30 to 100 times greater affinity for the ERs as tamoxifen itself.[69] Tamoxifen has 7% and 6% of the affinity of estradiol for the ERα and ERβ, respectively, whereas afimoxifene has 178% and 338% of the affinity of estradiol for the ERα and ERβ, respectively.[70] Hence, afimoxifine has 25-fold higher affinity for the ERα and 56-fold higher affinity for the ERβ than tamoxifen.[71] Tamoxifen is a long-acting SERM, with a nuclear retention of the ER–tamoxifen complex of greater than 48 hours.[72][73]
Afimoxifene binds to ER, the ER/tamoxifen complex recruits other proteins known as co-repressors, and the complex then binds to DNA to modulate gene expression. Some of these proteins include NCoR and SMRT.[74] Tamoxifen function can be regulated by a number of different variables including growth factors.[75] Tamoxifen needs to block growth factor proteins such as ErbB2/HER2[76] because high levels of ErbB2 have been shown to occur in tamoxifen resistant cancers.[77] Tamoxifen seems to require a protein PAX2 for its full anticancer effect.[76][78] In the presence of high PAX2 expression, the tamoxifen/ER complex is able to suppress the expression of the pro-proliferative ERBB2 protein. In contrast, when AIB-1 expression is higher than PAX2, tamoxifen/ER complex upregulates the expression of ERBB2 resulting in stimulation of breast cancer growth.[76][79]
Afimoxifene binds to ER competitively (with respect to the endogenous agonist estrogen) in tumor cells and other tissue targets, producing a nuclear complex that decreases DNA synthesis and inhibits estrogen effects. It is a nonsteroidal agent with potent antiestrogenic properties which compete with estrogen for binding sites in breast and other tissues. Tamoxifen causes cells to remain in the G0 and G1 phases of the cell cycle. Because it prevents (pre)cancerous cells from dividing but does not cause cell death, tamoxifen is cytostatic rather than cytocidal.
The scientific literature is complex with respect to the activity of tamoxifen, and care should be taken to establish whether tamoxifen, or afimoxifene was used, especially in in-vitro assays.
Tamoxifen has been found to decrease insulin-like growth factor 1 (IGF-1) levels by 17 to 38% in women and men.[80] Suppression of IGF-1 production in the liver is a well-known action of estrogens and SERMs.[80] A 10 mg/day dosage of tamoxifen is nearly as effective as a 20 mg/day dosage in suppressing IGF-1 levels.[4]
The effects of tamoxifen on breast cancer Ki-67 expression, sex hormone-binding globulin (SHBG) levels, and IGF-1 levels are dose-dependent across a dosage range of one to 20 mg/day in women with breast cancer.[81]
Tamoxifen is antigonadotropic in postmenopausal women and partially suppresses levels of the gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in such women.[82] However, it has progonadotropic effects in premenopausal women and increases estrogen levels by 6-fold in them.[82] Due to the nature of tamoxifen as a competitive ER ligand, this increase in estrogen levels is liable to interfere with the antiestrogenic efficacy of tamoxifen.[82]
| Medication | Breast | Bone | Liver | Uterus | Vagina | Brain | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lipids | Coagulation | SHBG | IGF-1 | Hot flashes | Gonadotropins | |||||||||
| Estradiol | + | + | + | + | + | + | + | + | + | + | ||||
| "Ideal SERM" | – | + | + | ± | ± | ± | – | + | + | ± | ||||
| Bazedoxifene | – | + | + | + | + | ? | – | ± | – | ? | ||||
| Clomifene | – | + | + | ? | + | + | – | ? | – | ± | ||||
| Lasofoxifene | – | + | + | + | ? | ? | ± | ± | – | ? | ||||
| Ospemifene | – | + | + | + | + | + | ± | ± | – | ± | ||||
| Raloxifene | – | + | + | + | + | + | ± | – | – | ± | ||||
| Tamoxifen | – | + | + | + | + | + | + | – | – | ± | ||||
| Toremifene | – | + | + | + | + | + | + | – | – | ± | ||||
| Effect: + = Estrogenic / agonistic. ± = Mixed or neutral. – = Antiestrogenic / antagonistic. Note: SERMs generally increase gonadotropin levels in hypogonadal and eugonadal men as well as premenopausal women (antiestrogenic) but decrease gonadotropin levels in postmenopausal women (estrogenic). Sources: See template. | ||||||||||||||
Other activities
Afimoxifene is an agonist of the G protein-coupled estrogen receptor (GPER) with relatively low affinity (100–1,000 nM, relative to 3–6 nM for estradiol).[83]
Norendoxifen (N,N-didesmethyl-4-hydroxytamoxifen), another active metabolite of tamoxifen, has been found to act as a potent competitive aromatase inhibitor (IC50 = 90 nM), and may also be involved in the antiestrogenic activity of tamoxifen.[84]
In addition to its activity as a SERM, tamoxifen is a potent and selective protein kinase C inhibitor, and is active in this regard at therapeutic concentrations.[85] This action is thought to underlie the efficacy of tamoxifen in the treatment of bipolar disorder.[85]
Tamoxifen is an inhibitor of P-glycoprotein.[7]
Pharmacokinetics
Tamoxifen is rapidly and extensively absorbed from the intestines with oral administration.[4][5] The oral bioavailability of tamoxifen is high at approximately 100%, which is suggestive of minimal first-pass metabolism in the intestines and liver.[4] Following intake, peak levels of tamoxifen occur after three to seven hours.[86][4] Steady state levels of tamoxifen are reached typically after three to four weeks but possibly up to 16 weeks of daily administration.[4][87] Steady state levels of afimoxifene are achieved after 8 weeks of daily tamoxifen administration.[87][6]
The volume of distribution of tamoxifen is 50 to 60 L/kg and its clearance has been estimated as 1.2 to 5.1 L/hour.[4][86] High concentrations of tamoxifen have been found in breast, uterus, liver, kidney, lung, pancreas, and ovary tissue in animals and humans.[4] Levels of tamoxifen in the uterus have been found to be 2- to 3-fold higher than in the circulation.[4] The plasma protein binding of tamoxifen and afimoxifene is greater than 99%.[6] A majority of tamoxifen is bound to albumin.[4]
Tamoxifen itself is a prodrug is metabolized in the liver by the cytochrome P450 isoforms CYP3A4, CYP2C9, and CYP2D6 into active metabolites such as afimoxifene and endoxifen.[4][7][8] Tamoxifen and its metabolites undergo conjugation, including glucuronidation and sulfation.[87] Tamoxifen may inhibit its own metabolism.[4]
Tamoxifen has a long elimination half-life of typically five to seven days, with a range of four to eleven days.[4][8][86] Similarly, the half-life of afimoxifene is 14 days.[6] Conversely, the half-life of endoxifen is 50 to 70 hours.[8] The long half-lives of tamoxifen and afimoxifene are attributed to their high plasma protein binding as well as to enterohepatic recirculation.[6] Upon discontinuation of treatment, levels of tamoxifen and its metabolites persist in the circulation for at least 6 weeks.[6] Tamoxifen is excreted in bile and is eliminated in feces, while small amounts are eliminated in urine.[4]
Chemistry
Tamoxifen is a nonsteroidal SERM of the triphenylethylene family and was structurally derived from diethylstilbestrol-like estrogens and antiestrogens such as chlorotrianisene and ethamoxytriphetol.[88][89][90][91] Initially, clomifene was synthesized, and tamoxifen was developed subsequently.[88][90][91] Tamoxifen is closely related structurally to other triphenylethylenes, such as clomifene, nafoxidine, ospemifene, toremifene, and numerous others.[92][93] Other SERMs, like raloxifene, are structurally distinct from tamoxifen and other triphenylethylenes.[93]
History
In the late 1950s, pharmaceutical companies were actively researching a newly discovered class of anti-estrogen compounds in the hope of developing a morning-after contraceptive pill. Arthur L Walpole was a reproductive endocrinologist who led such a team at the Alderley Park research laboratories of ICI Pharmaceuticals.[14] It was there in 1962 that chemist Dora Richardson first synthesized tamoxifen, back then known as ICI-46,474, when she was looking to create triphenylethylene derivatives for the contraceptive pill project that her team was researching.[94]
This compound was originally created to work as an estrogen inhibitor, but instead was found to stimulate ovulation in participants of the drug testing trial.[13] Walpole and his colleagues filed a UK patent covering this compound in 1962, but patent protection on this compound was repeatedly denied in the US until the 1980s.[95] Tamoxifen did eventually receive marketing approval as a fertility treatment, but the class of compounds never proved useful in human contraception. A link between estrogen and breast cancer had been known for many years, but cancer treatments were not a corporate priority at the time, and Walpole's personal interests were important in keeping support for the compound alive in the face of this and the lack of patent protection.[14] It was only when Walpole threatened to leave his position that corporate decided to allow trials and testing for Tamoxifen as a drug that could be used to treat breast cancer. Without Walpole's effort towards defending the work that his team had done in discovering a possibly revolutionary source for breast cancer treatment, Tamoxifen could have become a discarded or under-researched idea. Walpole's team consisted of Dora Richardson and G.A. Snow, who worked on the chemistry portion of the project, along with G.E. Paget and J.K. Walley, who focused primarily on the biological side.[13]
Tamoxifen is one of three drugs in an anti-angiogenetic protocol developed by Dr. Judah Folkman, a researcher at Children's Hospital at Harvard Medical School in Boston. Folkman discovered in the 1970s that angiogenesis – the growth of new blood vessels – plays a significant role in the development of cancer. Since his discovery, an entirely new field of cancer research has developed. Clinical trials on angiogenesis inhibitors have been underway since 1992 using many different drugs. The Harvard researchers developed a specific protocol for a golden retriever named Navy who was cancer-free after receiving the prescribed cocktail of celecoxib, doxycycline, and tamoxifen – the treatment subsequently became known as the Navy Protocol.[96] Furthermore, tamoxifen treatment alone has been shown to have anti-angiogenetic effects in animal models of cancer which appear to be, at least in part, independent of tamoxifen's ER antagonist properties.[97]
Other antiestrogens, such as ethamoxytriphetol (MER-25) and clomifene (MRL-41), were assessed for treatment of breast cancer and found to be effective before tamoxifen, but were plagued with toxicity issues.[98][99] The first clinical study of tamoxifen took place at the Christie Hospital in 1971, and showed a convincing effect in advanced breast cancer, but nevertheless ICI's development programme came close to termination when it was reviewed in 1972.[100] In an unpublished article from the early days of the trial, Dora Richardson documented her team's excitement about tamoxifen's effects in counteracting infertility problems and the early positive effects found in breast cancer patients. Unfortunately, this work was not well received by everyone, as the team was supposed to be looking for a contraceptive pill.[13] Tamoxifen's further development may have been bolstered by a second clinical study by Harold W.C. Ward [101] at the Queen Elizabeth Hospital, Birmingham. Ward's study showed a more definitive response to the drug at a higher dosage. Walpole also may have helped to convince the company to market tamoxifen for late stage breast cancer in 1973.[95] He was also instrumental in funding V. Craig Jordan to work on tamoxifen. In 1972, ICI Pharmaceuticals Division abandoned development of tamoxifen for financial reasons. The drug was subsequently reinvented from a failed contraceptive, to become tamoxifen, the gold standard for the adjuvant treatment of breast cancer and the pioneering medicine for chemprevention for high risk women.[102][103] Two books, Estrogen Action, Selective Estrogen Receptor Modulators and Women's Health (Imperial College Press 2013) and Tamoxifen Pioneering Medicine in Breast Cancer (Springer 2013) tell this story.
| Antiestrogen | Dosage | Year(s) | Response rate | Toxicity |
|---|---|---|---|---|
| Ethamoxytriphetol | 500–4,500 mg/day | 1960 | 25% | Acute psychotic episodes |
| Clomifene | 100–300 mg/day | 1964–1974 | 34% | Fears of cataracts |
| Nafoxidine | 180–240 mg/day | 1976 | 31% | Cataracts, ichthyosis, photophobia |
| Tamoxifen | 20–40 mg/day | 1971–1973 | 31% | Transient thrombocytopeniaa |
| Footnotes: a = "The particular advantage of this drug is the low incidence of troublesome side effects (25)." "Side effects were usually trivial (26)." Sources: See template. | ||||
1980 saw the publication of the first trial to show that tamoxifen given in addition to chemotherapy improved survival for patients with early breast cancer.[104] In advanced disease, tamoxifen is now only recognized as effective in ER+ patients, but the early trials did not select ER+ patients, and by the mid 1980s the clinical trial picture was not showing a major advantage for tamoxifen.[105] Nevertheless, tamoxifen had a relatively mild side-effect profile, and a number of large trials continued.
The pharmacology of SERMs was discovered, defined, and deciphered during the 1980s [106] A clinical strategy was described [107] that led to the creation of SERMs as a group of multifunctional medicines aimed at the treatment or prevention of many conditions in postmenopausal women, e.g. osteoporosis and breast cancer. This story is told in: V. Craig Jordan, ed. 2013. "Estrogen Action, Selective Estrogen Receptor Modulators and Women's Health" Imperial College Press, Singapore.
The early sales of tamoxifen in both the UK and in the U.S. far exceeded ICI's original estimate, but despite this, at the annual portfolio review ICI's board members still asserted that "there was no market for cancer", leaving the drug's marketing success to rely on its clinical results and clinicians and scientists interests in it. Shortly after, Dora Richardson published a history of Tamoxifen that, unusually for that type of paper, included personal accounts and letters from patients who attributed their healing to the drug. It is by giving voice to cancer patients using Tamoxifen, and so helping to push it forward, by justifying it both morally and scientifically to corporations.[13]
It was not until 1998 that the meta-analysis of the Oxford-based Early Breast Cancer Trialists' Collaborative Group showed definitively that tamoxifen saved lives in early breast cancer.[108]
Society and culture
Brand names
Tamoxifen is marketed primarily under the brand name Nolvadex, but is also available under a variety of other brand names throughout the world.[109]
Economics
Global sales of tamoxifen in 2001 were $1,024 million.[110] Since the expiration of the patent in 2002, it is widely available as a generic drug around the world. As of 2004, tamoxifen was the world's largest selling hormonal drug for the treatment of breast cancer.[111]
Cost
The wholesale price in the developing world is about US$0.07–0.23 per day.[16] In 2017, it was the 251st most commonly prescribed medication in the United States, with more than one million prescriptions.[17][18] Tamoxifen is inexpensive in the UK,[112] costing the NHS around £0.16 per day.[113]
.svg.png.webp) Tamoxifen costs (US)
Tamoxifen costs (US).svg.png.webp) Tamoxifen prescriptions (US)
Tamoxifen prescriptions (US)
Research
In McCune-Albright syndrome (MAS) tamoxifen has been used to treat premature puberty and the consequences of premature puberty. Tamoxifen has been seen to decrease rapid bone maturation which is the result of excessive estrogen and alter predicted adult height (PAH).[114][115] The same effects have also been seen in short pubertal boys.[116] However, one in vitro study in 2007 and later an in vivo study in 2008 have shown that tamoxifen induces apoptosis in growth plate chondrocytes, reduces serum insulin-like growth factor 1 (IGF-1) levels and causes persistent retardation of longitudinal and cortical radial bone growth in young male rats, leading the researchers to express concern giving tamoxifen to growing individuals.[117][118]
Tamoxifen has been studied in the treatment of the rare conditions of retroperitoneal fibrosis[119] and idiopathic sclerosing mesenteritis.[120] It has also been proposed as part of a treatment plan for Riedel's thyroiditis.[121]
Tamoxifen is used as a research tool to trigger tissue-specific gene expression in many conditional expression constructs in genetically modified animals including a version of the Cre-Lox recombination technique.[122]
Tamoxifen may be effective in the treatment of mania in people with bipolar disorder.[123] This is thought to be due to blockade of protein kinase C (PKC), an enzyme that regulates neuron activity in the brain.[123][124] Researchers believe PKC is overactive during the mania in bipolar patients.[123][124] As of September 2019, endoxifen, a major active metabolite of tamoxifen with a fourfold more potent PKC inhibition, was in phase III clinical trials for bipolar disorder.[125][126]
References
- ↑ "NCI Drug Dictionary". 2011-02-02. Archived from the original on 8 December 2015. Retrieved 28 November 2015.
- 1 2 "Tamoxifen Use During Pregnancy". Drugs.com. 25 July 2019. Archived from the original on 27 January 2020. Retrieved 27 January 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 8 November 2020. Retrieved 22 September 2020.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Morello KC, Wurz GT, DeGregorio MW (2003). "Pharmacokinetics of selective estrogen receptor modulators". Clinical Pharmacokinetics. 42 (4): 361–72. doi:10.2165/00003088-200342040-00004. PMID 12648026. S2CID 13003168.
- 1 2 George M. Brenner; Craig Stevens (28 September 2017). Brenner and Stevens' Pharmacology E-Book. Elsevier Health Sciences. pp. 394–. ISBN 978-0-323-39172-6. Archived from the original on 29 August 2021. Retrieved 6 July 2019.
- 1 2 3 4 5 6 Bruce A. Chabner; Dan L. Longo (7 December 2011). Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. pp. 655–. ISBN 978-1-4511-4820-6. Archived from the original on 29 August 2021. Retrieved 6 July 2019.
- 1 2 3 4 5 6 7 8 9 10 11 "Archive copy" (PDF). Archived (PDF) from the original on 2021-03-30. Retrieved 2019-07-06.
{{cite web}}: CS1 maint: archived copy as title (link) - 1 2 3 4 5 6 7 8 Sanchez-Spitman AB, Swen JJ, Dezentje VO, Moes DJ, Gelderblom H, Guchelaar HJ (June 2019). "Clinical pharmacokinetics and pharmacogenetics of tamoxifen and endoxifen". Expert Review of Clinical Pharmacology. 12 (6): 523–536. doi:10.1080/17512433.2019.1610390. PMID 31008668.
- 1 2 "Tamoxifen Citrate". NCI. August 26, 2015. Archived from the original on 4 January 2016. Retrieved 28 November 2015.
- 1 2 3 4 5 6 7 8 9 "Tamoxifen Citrate". The American Society of Health-System Pharmacists. Archived from the original on 2014-01-04. Retrieved 27 Nov 2015.
- ↑ "Selective estrogen receptor modulators". Archived from the original on 9 December 2013. Retrieved 28 November 2015.
- ↑ Cano A, Calaf i Alsina J, Duenas-Diez JL, eds. (2006). Selective Estrogen Receptor Modulators a New Brand of Multitarget Drugs. Berlin, Heidelberg: Springer-Verlag Berlin Heidelberg. p. 52. ISBN 9783540347422. Archived from the original on 2021-06-24. Retrieved 2017-09-15.
- 1 2 3 4 5 Quirke VM (12 Sep 2017). "Tamoxifen from Failed Contraceptive Pill to Best-Selling Breast Cancer Medicine: A Case-Study in Pharmaceutical Innovation". Frontiers in Pharmacology. 8: 620. doi:10.3389/fphar.2017.00620. PMC 5600945. PMID 28955226.
- 1 2 3 Jordan VC (January 2006). "Tamoxifen (ICI46,474) as a targeted therapy to treat and prevent breast cancer". British Journal of Pharmacology. 147 Suppl 1 (Suppl 1): S269-76. doi:10.1038/sj.bjp.0706399. PMC 1760730. PMID 16402113.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- 1 2 "Tamoxifen Citrate". International Drug Price Indicator Guide. Archived from the original on 22 January 2018. Retrieved 28 November 2015.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 18 March 2020. Retrieved 11 April 2020.
- 1 2 "Tamoxifen Citrate - Drug Usage Statistics". ClinCalc. Archived from the original on 22 September 2020. Retrieved 11 April 2020.
- ↑ Jordan VC (October 1993). "Fourteenth Gaddum Memorial Lecture. A current view of tamoxifen for the treatment and prevention of breast cancer". British Journal of Pharmacology. 110 (2): 507–17. doi:10.1111/j.1476-5381.1993.tb13840.x. PMC 2175926. PMID 8242225.
- ↑ "Breast cancer in men". CancerHelp UK. Cancer Research UK. 2007-09-28. Archived from the original on 2008-12-01. Retrieved 2009-03-22.
- ↑ Center for Drug Evaluation and Research (July 7, 2005). "Tamoxifen Information: reducing the incidence of breast cancer in women at high risk". U.S. Food and Drug Administration. Archived from the original on June 19, 2007. Retrieved July 3, 2007.
- ↑ Burstein HJ, Temin S, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. (July 2014). "Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update". Journal of Clinical Oncology. 32 (21): 2255–69. doi:10.1200/JCO.2013.54.2258. PMC 4876310. PMID 24868023.
- ↑ National Cancer Institute (2006-04-26). "Study of Tamoxifen and Raloxifene (STAR) Trial". U.S. National Institutes of Health. Archived from the original on July 4, 2007. Retrieved July 3, 2007.
- ↑ University of Pittsburgh. "STAR Study of Tamoxifen and Raloxifen". Archived from the original on June 11, 2007. Retrieved July 3, 2007.
- ↑ Dr Susan Love (April 22, 2006). "Study Finds New Use for Raloxifene: Reducing Breast Cancer in High-Risk Postmenopausal Women". Archived from the original on August 2, 2009. Retrieved March 19, 2009.
- ↑ Steiner AZ, Terplan M, Paulson RJ (June 2005). "Comparison of tamoxifen and clomiphene citrate for ovulation induction: a meta-analysis". Human Reproduction. 20 (6): 1511–5. doi:10.1093/humrep/deh840. PMID 15845599.
- ↑ Chua ME, Escusa KG, Luna S, Tapia LC, Dofitas B, Morales M (September 2013). "Revisiting oestrogen antagonists (clomiphene or tamoxifen) as medical empiric therapy for idiopathic male infertility: a meta-analysis". Andrology. 1 (5): 749–57. doi:10.1111/j.2047-2927.2013.00107.x. PMID 23970453.
- ↑ Lapid O, van Wingerden JJ, Perlemuter L (2013). "Tamoxifen therapy for the management of pubertal gynecomastia: a systematic review". Journal of Pediatric Endocrinology & Metabolism. 26 (9–10): 803–7. doi:10.1515/jpem-2013-0052. PMID 23729603. S2CID 2101602.
- ↑ Viani GA, Bernardes da Silva LG, Stefano EJ (July 2012). "Prevention of gynecomastia and breast pain caused by androgen deprivation therapy in prostate cancer: tamoxifen or radiotherapy?". International Journal of Radiation Oncology, Biology, Physics. 83 (4): e519-24. doi:10.1016/j.ijrobp.2012.01.036. PMID 22704706.
- ↑ Fentiman IS (January 2018). "Managing Male Mammary Maladies". Eur J Breast Health. 14 (1): 5–9. doi:10.5152/ejbh.2017.3841. PMC 5758064. PMID 29322112.
- ↑ Fradet Y, Egerdie B, Andersen M, Tammela TL, Nachabe M, Armstrong J, Morris T, Navani S (July 2007). "Tamoxifen as prophylaxis for prevention of gynaecomastia and breast pain associated with bicalutamide 150 mg monotherapy in patients with prostate cancer: a randomised, placebo-controlled, dose-response study". Eur. Urol. 52 (1): 106–14. doi:10.1016/j.eururo.2007.01.031. PMID 17270340.
- 1 2 Neyman A, Eugster EA (December 2017). "Treatment of Girls and Boys with McCune-Albright Syndrome with Precocious Puberty - Update 2017". Pediatric Endocrinology Reviews. 15 (2): 136–141. doi:10.17458/per.vol15.2017.nau.treatmentgirlsboys. PMC 5808444. PMID 29292624.
- 1 2 Haddad NG, Eugster EA (April 2019). "Peripheral precocious puberty including congenital adrenal hyperplasia: causes, consequences, management and outcomes". Best Practice & Research. Clinical Endocrinology & Metabolism. 33 (3): 101273. doi:10.1016/j.beem.2019.04.007. hdl:1805/19111. PMID 31027974.
- ↑ Zacharin M (May 2019). "Disorders of Puberty: Pharmacotherapeutic Strategies for Management". Handbook of Experimental Pharmacology. doi:10.1007/164_2019_208. PMID 31144045.
- ↑ Product Information: tamoxifen citrate oral tablets, tamoxifen citrate oral tablets. Watson Laboratories (per manufacturer), Corona, CA, 2011.
- ↑ Product Information: SOLTAMOX(R) oral solution, tamoxifen citrate oral solution. Midatech Pharma US Inc (per FDA), Raleigh, NC, 2018.
- ↑ OncoGenetics.Org (September 2009). "Medications Effective in Reducing Risk of Breast Cancer But Increase Risk of Adverse Effects". OncoGenetics.Org. Archived from the original on September 24, 2009. Retrieved 2009-09-14.
- ↑ Nakamura T, Imai Y, Matsumoto T, Sato S, Takeuchi K, Igarashi K, et al. (September 2007). "Estrogen prevents bone loss via estrogen receptor alpha and induction of Fas ligand in osteoclasts". Cell. 130 (5): 811–23. doi:10.1016/j.cell.2007.07.025. PMID 17803905. S2CID 17177462.
- ↑ Krum SA, Miranda-Carboni GA, Hauschka PV, Carroll JS, Lane TF, Freedman LP, Brown M (February 2008). "Estrogen protects bone by inducing Fas ligand in osteoblasts to regulate osteoclast survival". The EMBO Journal. 27 (3): 535–45. doi:10.1038/sj.emboj.7601984. PMC 2241656. PMID 18219273.
- ↑ Mincey BA, Moraghan TJ, Perez EA (August 2000). "Prevention and treatment of osteoporosis in women with breast cancer". Mayo Clinic Proceedings. 75 (8): 821–9. doi:10.4065/75.8.821. PMID 10943237.
- ↑ Vehmanen L, Elomaa I, Blomqvist C, Saarto T (February 2006). "Tamoxifen treatment after adjuvant chemotherapy has opposite effects on bone mineral density in premenopausal patients depending on menstrual status". Journal of Clinical Oncology. 24 (4): 675–80. doi:10.1200/JCO.2005.02.3515. PMID 16446340.
- ↑ Gallo MA, Kaufman D (February 1997). "Antagonistic and agonistic effects of tamoxifen: significance in human cancer". Seminars in Oncology. 24 (1 Suppl 1): S1-71-S1-80. PMID 9045319.
- ↑ Grilli S (2006). "Tamoxifen (TAM): the dispute goes on" (PDF). Annali dell'Istituto Superiore di Sanita. 42 (2): 170–3. PMID 17033137. Archived from the original (PDF) on 2007-08-10. Retrieved 2007-07-03.
- ↑ "Tamoxifen for Breast Cancer & Side Effects". Health and Life. 2009-12-11. Archived from the original on 2010-02-16.
- ↑ "Known and Probable Carcinogens". American Cancer Society. 2006-02-03. Archived from the original on 2008-03-17. Retrieved 2008-03-21.
- ↑ Esteva FJ, Hortobagyi GN (June 2006). "Comparative assessment of lipid effects of endocrine therapy for breast cancer: implications for cardiovascular disease prevention in postmenopausal women". Breast. 15 (3): 301–12. doi:10.1016/j.breast.2005.08.033. PMID 16230014.
- ↑ Decensi A, Maisonneuve P, Rotmensz N, Bettega D, Costa A, Sacchini V, et al. (February 2005). "Effect of tamoxifen on venous thromboembolic events in a breast cancer prevention trial". Circulation. 111 (5): 650–6. doi:10.1161/01.CIR.0000154545.84124.AC. PMID 15699284.
- ↑ Harvey HA, Kimura M, Hajba A (April 2006). "Toremifene: an evaluation of its safety profile". Breast. 15 (2): 142–57. doi:10.1016/j.breast.2005.09.007. PMID 16289904.
- ↑ Osman KA, Osman MM, Ahmed MH (January 2007). "Tamoxifen-induced non-alcoholic steatohepatitis: where are we now and where are we going?". Expert Opinion on Drug Safety. 6 (1): 1–4. doi:10.1517/14740338.6.1.1. PMID 17181445. S2CID 33505288.
- ↑ Paganini-Hill A, Clark LJ (November 2000). "Preliminary assessment of cognitive function in breast cancer patients treated with tamoxifen". Breast Cancer Research and Treatment. 64 (2): 165–76. doi:10.1023/A:1006426132338. PMID 11194452. S2CID 1033695.
- ↑ Eberling JL, Wu C, Tong-Turnbeaugh R, Jagust WJ (January 2004). "Estrogen- and tamoxifen-associated effects on brain structure and function". NeuroImage. 21 (1): 364–71. doi:10.1016/j.neuroimage.2003.08.037. PMID 14741674. S2CID 15920274.
- ↑ Bender CM, Sereika SM, Brufsky AM, Ryan CM, Vogel VG, Rastogi P, et al. (2007). "Memory impairments with adjuvant anastrozole versus tamoxifen in women with early-stage breast cancer". Menopause. 14 (6): 995–8. doi:10.1097/gme.0b013e318148b28b. PMC 2831410. PMID 17898668.
- ↑ Mortimer JE, Boucher L, Baty J, Knapp DL, Ryan E, Rowland JH (May 1999). "Effect of tamoxifen on sexual functioning in patients with breast cancer". Journal of Clinical Oncology. 17 (5): 1488–92. doi:10.1200/JCO.1999.17.5.1488. PMID 10334535.
- ↑ Cella D, Fallowfield L, Barker P, Cuzick J, Locker G, Howell A (December 2006). "Quality of life of postmenopausal women in the ATAC ("Arimidex", tamoxifen, alone or in combination) trial after completion of 5 years' adjuvant treatment for early breast cancer". Breast Cancer Research and Treatment. 100 (3): 273–84. doi:10.1007/s10549-006-9260-6. PMID 16944295. S2CID 24855843.
- 1 2 Ross Cameron; George Feuer; Felix de la Iglesia (6 December 2012). Drug-Induced Hepatotoxicity. Springer Science & Business Media. pp. 565–. ISBN 978-3-642-61013-4. Archived from the original on 28 August 2021. Retrieved 13 July 2019.
- ↑ "Tamoxifen: Hormone therapy drugs". Breast Cancer Care. 2015-06-08. Archived from the original on 2019-09-20. Retrieved 2019-09-20.
- ↑ Kumar, N.B.; Allen, K.; Cantor, A.; Cox, C.E.; Greenberg, H.; Shah, S.; Lyman, G.H. (1997-06-01). "Weight gain associated with adjuvant tamoxifen therapy in stage I and II breast cancer: fact or artifact?". Breast Cancer Research and Treatment. 44 (2): 135–143. doi:10.1023/A:1005721720840. ISSN 1573-7217. PMID 9232272. S2CID 39451228.
- ↑ Goetz MP, Rae JM, Suman VJ, Safgren SL, Ames MM, Visscher DW, et al. (December 2005). "Pharmacogenetics of tamoxifen biotransformation is associated with clinical outcomes of efficacy and hot flashes". Journal of Clinical Oncology. 23 (36): 9312–8. doi:10.1200/JCO.2005.03.3266. PMID 16361630.
- ↑ Beverage JN, Sissung TM, Sion AM, Danesi R, Figg WD (September 2007). "CYP2D6 polymorphisms and the impact on tamoxifen therapy". Journal of Pharmaceutical Sciences. 96 (9): 2224–31. doi:10.1002/jps.20892. PMID 17518364.
- ↑ Information about CYP2D6 and tamoxifen from DNADirect's website Archived 2007-03-11 at the Wayback Machine
- ↑ Schroth W, Goetz MP, Hamann U, Fasching PA, Schmidt M, Winter S, et al. (October 2009). "Association between CYP2D6 polymorphisms and outcomes among women with early stage breast cancer treated with tamoxifen". JAMA. 302 (13): 1429–36. doi:10.1001/jama.2009.1420. PMC 3909953. PMID 19809024.
- ↑ Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH, et al. (January 2005). "CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment". Journal of the National Cancer Institute. 97 (1): 30–9. doi:10.1093/jnci/dji005. PMID 15632378.
- ↑ Staff Reports (Summer 2009). "ASCO Updates: Antidepressants Reduce the Effectiveness of Tamoxifen". CURE (Cancer Updates, Research and Education). Archived from the original on 2009-06-22.
- ↑ Kelly CM, Juurlink DN, Gomes T, Duong-Hua M, Pritchard KI, Austin PC, Paszat LF (February 2010). "Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study". BMJ. 340: c693. doi:10.1136/bmj.c693. PMC 2817754. PMID 20142325.
- ↑ Information about Tamoxitest and how DNA testing can help in the selection of the best treatment methodology from Genelex's website Archived 2010-05-27 at the Wayback Machine
- ↑ Criscitiello C, Fumagalli D, Saini KS, Loi S (December 2010). "Tamoxifen in early-stage estrogen receptor-positive breast cancer: overview of clinical use and molecular biomarkers for patient selection". OncoTargets and Therapy. 4: 1–11. doi:10.2147/OTT.S10155. PMC 3084302. PMID 21552410.
- ↑ PDB: 3ERT; Shiau AK, Barstad D, Loria PM, Cheng L, Kushner PJ, Agard DA, Greene GL (December 1998). "The structural basis of estrogen receptor/coactivator recognition and the antagonism of this interaction by tamoxifen". Cell. 95 (7): 927–37. doi:10.1016/S0092-8674(00)81717-1. PMID 9875847.
- ↑ Wang DY, Fulthorpe R, Liss SN, Edwards EA (February 2004). "Identification of estrogen-responsive genes by complementary deoxyribonucleic acid microarray and characterization of a novel early estrogen-induced gene: EEIG1". Molecular Endocrinology. 18 (2): 402–11. doi:10.1210/me.2003-0202. PMID 14605097.
- ↑ Ahmad A, Shahabuddin S, Sheikh S, Kale P, Krishnappa M, Rane RC, Ahmad I (December 2010). "Endoxifen, a new cornerstone of breast cancer therapy: demonstration of safety, tolerability, and systemic bioavailability in healthy human subjects". Clinical Pharmacology and Therapeutics. 88 (6): 814–7. doi:10.1038/clpt.2010.196. PMID 20981001.
- ↑ Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ↑ Potts RO, Lobo RA (May 2005). "Transdermal drug delivery: clinical considerations for the obstetrician-gynecologist". Obstet Gynecol. 105 (5 Pt 1): 953–61. doi:10.1097/01.AOG.0000161958.70059.db. PMID 15863530. S2CID 23411589.
- ↑ Benno Runnebaum; Thomas Rabe (17 April 2013). Gynäkologische Endokrinologie und Fortpflanzungsmedizin: Band 1: Gynäkologische Endokrinologie. Springer-Verlag. pp. 88–. ISBN 978-3-662-07635-4. Archived from the original on 17 June 2020. Retrieved 27 April 2019.
- ↑ Wallach, Edward E.; Hammond, Charles B.; Maxson, Wayne S. (1982). "Current status of estrogen therapy for the menopause". Fertility and Sterility. 37 (1): 5–25. doi:10.1016/S0015-0282(16)45970-4. ISSN 0015-0282. PMID 6277697.
- ↑ Shang Y, Hu X, DiRenzo J, Lazar MA, Brown M (December 2000). "Cofactor dynamics and sufficiency in estrogen receptor-regulated transcription". Cell. 103 (6): 843–52. doi:10.1016/S0092-8674(00)00188-4. PMID 11136970. S2CID 6659079.
- ↑ Massarweh S, Osborne CK, Creighton CJ, Qin L, Tsimelzon A, Huang S, et al. (February 2008). "Tamoxifen resistance in breast tumors is driven by growth factor receptor signaling with repression of classic estrogen receptor genomic function". Cancer Research. 68 (3): 826–33. doi:10.1158/0008-5472.CAN-07-2707. PMID 18245484.
- 1 2 3 Hurtado A, Holmes KA, Geistlinger TR, Hutcheson IR, Nicholson RI, Brown M, et al. (December 2008). "Regulation of ERBB2 by oestrogen receptor-PAX2 determines response to tamoxifen". Nature. 456 (7222): 663–6. Bibcode:2008Natur.456..663H. doi:10.1038/nature07483. PMC 2920208. PMID 19005469.
- ↑ Osborne CK, Bardou V, Hopp TA, Chamness GC, Hilsenbeck SG, Fuqua SA, et al. (March 2003). "Role of the estrogen receptor coactivator AIB1 (SRC-3) and HER-2/neu in tamoxifen resistance in breast cancer". Journal of the National Cancer Institute. 95 (5): 353–61. doi:10.1093/jnci/95.5.353. PMID 12618500.
- ↑ "New Mechanism Predicts Tamoxifen Response: PAX2 gene implicated in tamoxifen-induced inhibition of ERBB2/HER2-mediated tumor growth". www.modernmedicine.com. 2008-11-13. Archived from the original on 2011-07-14. Retrieved 2008-11-14.
- ↑ "Study sheds new light on tamoxifen resistance". News. CORDIS News. Archived from the original on 2009-02-20. Retrieved 2008-11-14.
- 1 2 Duarte FH, Jallad RS, Bronstein MD (November 2016). "Estrogens and selective estrogen receptor modulators in acromegaly". Endocrine. 54 (2): 306–314. doi:10.1007/s12020-016-1118-z. PMID 27704479. S2CID 10136018.
- ↑ Fabian CJ, Kimler BF (March 2005). "Selective estrogen-receptor modulators for primary prevention of breast cancer". J. Clin. Oncol. 23 (8): 1644–55. doi:10.1200/JCO.2005.11.005. PMID 15755972.
- 1 2 3 Li J, Ma Z, Jiang RW, Wu B (September 2013). "Hormone-related pharmacokinetic variations associated with anti-breast cancer drugs". Expert Opin Drug Metab Toxicol. 9 (9): 1085–95. doi:10.1517/17425255.2013.802771. PMID 23687971.
- ↑ Prossnitz ER, Arterburn JB (July 2015). "International Union of Basic and Clinical Pharmacology. XCVII. G Protein-Coupled Estrogen Receptor and Its Pharmacologic Modulators". Pharmacol. Rev. 67 (3): 505–40. doi:10.1124/pr.114.009712. PMC 4485017. PMID 26023144.
- ↑ Liu J, Flockhart PJ, Lu D, Lv W, Lu WJ, Han X, et al. (September 2013). "Inhibition of cytochrome p450 enzymes by the e- and z-isomers of norendoxifen". Drug Metabolism and Disposition. 41 (9): 1715–20. doi:10.1124/dmd.113.052506. PMC 3876808. PMID 23824607.
- 1 2 Zarate CA, Manji HK (2009). "Protein kinase C inhibitors: rationale for use and potential in the treatment of bipolar disorder". CNS Drugs. 23 (7): 569–82. doi:10.2165/00023210-200923070-00003. PMC 2802274. PMID 19552485.
- 1 2 3 Vincent T. DeVita; Theodore S. Lawrence; Steven A. Rosenberg (18 March 2016). Prostate and Other Genitourinary Cancers: From Cancer: Principles & Practice of Oncology, 10th edition. Wolters Kluwer Health. pp. 990–. ISBN 978-1-4963-5421-1. Archived from the original on 29 August 2021. Retrieved 6 July 2019.
- 1 2 3 Nagar S (2010). "Pharmacokinetics of anti-cancer drugs used in breast cancer chemotherapy". Advances in Experimental Medicine and Biology. 678: 124–32. doi:10.1007/978-1-4419-6306-2_16. ISBN 978-1-4419-6305-5. PMID 20738014. S2CID 12537667.
- 1 2 Virgil Craig Jordan (1986). Estrogen/antiestrogen Action and Breast Cancer Therapy. Univ of Wisconsin Press. pp. 28, 154. ISBN 978-0-299-10480-1.
- ↑ William B. Pratt (1994). The Anticancer Drugs. Oxford University Press. pp. 21–. ISBN 978-0-19-506739-2.
- 1 2 Philipp Y. Maximov; Russell E. McDaniel; V. Craig Jordan (23 July 2013). Tamoxifen: Pioneering Medicine in Breast Cancer. Springer Science & Business Media. pp. 7–. ISBN 978-3-0348-0664-0. Archived from the original on 5 August 2020. Retrieved 13 July 2019.
- 1 2 Enrique Ravina (11 January 2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. pp. 177–178. ISBN 978-3-527-32669-3.
- ↑ Antonio Cano; Joacquim Calaf i Alsina; Jose Luis Duenas-Diez (22 September 2006). Selective Estrogen Receptor Modulators: A New Brand of Multitarget Drugs. Springer Science & Business Media. pp. 52–. ISBN 978-3-540-34742-2. Archived from the original on 24 June 2021. Retrieved 15 September 2017.
- 1 2 Eric S. Orwoll; John P. Bilezikian; Dirk Vanderschueren (30 November 2009). Osteoporosis in Men: The Effects of Gender on Skeletal Health. Academic Press. pp. 717–. ISBN 978-0-08-092346-8. Archived from the original on 29 August 2021. Retrieved 13 July 2019.
- ↑ Sneader, Walter (2005). Drug Discovery: A History. New York: Wiley. p. 472 pages. ISBN 978-0-471-89979-2.
- 1 2 Jordan VC (March 2003). "Tamoxifen: a most unlikely pioneering medicine". Nature Reviews. Drug Discovery. 2 (3): 205–13. doi:10.1038/nrd1031. PMID 12612646. S2CID 31333174.
- ↑ Kirk E (2002-07-24). "Dog's tale of survival opens door in cancer research". Health and Behavior. USA Today. Archived from the original on 2008-06-28. Retrieved 2008-06-24.
- ↑ Blackwell KL, Haroon ZA, Shan S, Saito W, Broadwater G, Greenberg CS, Dewhirst MW (November 2000). "Tamoxifen inhibits angiogenesis in estrogen receptor-negative animal models". Clinical Cancer Research. 6 (11): 4359–64. PMID 11106254. Archived from the original on 2008-09-06.
- ↑ Jensen EV, Jordan VC (June 2003). "The estrogen receptor: a model for molecular medicine". Clin. Cancer Res. 9 (6): 1980–9. PMID 12796359. Archived from the original on 2020-11-27. Retrieved 2020-06-02.
- ↑ Howell, Anthony; Jordan, V. Craig (2013). "Adjuvant Antihormone Therapy". In Craig, Jordan V. (ed.). Estrogen Action, Selective Estrogen Receptor Modulators And Women's Health: Progress And Promise. World Scientific. pp. 229–254. doi:10.1142/9781848169586_0010. ISBN 978-1-84816-959-3. Archived from the original on 2021-08-28. Retrieved 2020-06-02.
- ↑ Cole MP, Jones CT, Todd ID. "A new anti-oestrogenic agent in late breast cancer".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Ward HW (January 1973). "Anti-oestrogen therapy for breast cancer: a trial of tamoxifen at two dose levels". British Medical Journal. 1 (5844): 13–4. doi:10.1136/bmj.1.5844.13. PMC 1588574. PMID 4567104.
- ↑ "Maverick and pioneer whose work is improving odds in breast cancer fight". Archived from the original on 2013-06-28. Retrieved 2013-11-05.
- ↑ "Maverick and pioneer whose work is improving odds in breast cancer fight". The Yorkshire Post. 27 June 2013. Archived from the original on 2016-03-09. Retrieved April 7, 2017.
- ↑ Baum M, Brinkley DM, Dossett JA, McPherson K, Patterson JS, Rubens RD, et al. (August 1983). "Improved survival among patients treated with adjuvant tamoxifen after mastectomy for early breast cancer". Lancet. 2 (8347): 450. doi:10.1016/S0140-6736(83)90406-3. PMID 6135926. S2CID 54230182.
- ↑ Furr BJ, Jordan VC (1984). "The pharmacology and clinical uses of tamoxifen". Pharmacology & Therapeutics. 25 (2): 127–205. doi:10.1016/0163-7258(84)90043-3. PMID 6438654.
- ↑ Jordan VC (August 2001). "Selective estrogen receptor modulation: a personal perspective". Cancer Research. 61 (15): 5683–7. PMID 11479197.
- ↑ Lerner LJ, Jordan VC (July 1990). "Development of antiestrogens and their use in breast cancer: eighth Cain memorial award lecture". Cancer Research. 50 (14): 4177–89. PMID 2194650.
- ↑ Early Breast Cancer Trialists' Collaborative Group (May 1998). "Tamoxifen for early breast cancer: an overview of the randomised trials". Lancet. 351 (9114): 1451–67. doi:10.1016/S0140-6736(97)11423-4. PMID 9605801. S2CID 46287542.
- ↑ "Tamoxifen". Archived from the original on 2019-07-07. Retrieved 2019-07-07.
- ↑ "Cancer the generic impact". BioPortfolio Limited. Archived from the original on 2008-05-16. Retrieved 2008-11-14.
- ↑ Vose B. "AstraZenecain Cancer: Slide #15" (PDF). AstraZeneca Annual Business Review. www.astrazeneca.com. Archived (PDF) from the original on 2010-01-31. Retrieved 2009-03-28.
2004 tamoxifen market share: 70% Source: IMS HEALTH, IMS MIDAS Monthly. July 2004. Aromatase Inhibitors + Tamoxifen
- ↑ Hitchings, Andrew; Lonsdale, Dagan; Burrage, Daniel; Baker, Emma (2019). The Top 100 Drugs: Clinical Pharmacology and Practical Prescribing (2nd ed.). Elsevier. pp. 202–203. ISBN 978-0-7020-7442-4. Archived from the original on 2021-05-22. Retrieved 2021-11-09.
- ↑ BNF (80 ed.). London: BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 1005. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ Eugster EA, Shankar R, Feezle LK, Pescovitz OH (1999). "Tamoxifen treatment of progressive precocious puberty in a patient with McCune-Albright syndrome". Journal of Pediatric Endocrinology & Metabolism. 12 (5): 681–6. doi:10.1515/jpem.1999.12.5.681. PMID 10703542.
- ↑ Eugster EA, Rubin SD, Reiter EO, Plourde P, Jou HC, Pescovitz OH (July 2003). "Tamoxifen treatment for precocious puberty in McCune-Albright syndrome: a multicenter trial". The Journal of Pediatrics. 143 (1): 60–6. doi:10.1016/S0022-3476(03)00128-8. PMID 12915825.
- ↑ Kreher NC, Eugster EA, Shankar RR (December 2005). "The use of tamoxifen to improve height potential in short pubertal boys". Pediatrics. 116 (6): 1513–5. doi:10.1542/peds.2005-0577. PMID 16322179. S2CID 45133251.
- ↑ Karimian E, Chagin AS, Gjerde J, Heino T, Lien EA, Ohlsson C, Sävendahl L (August 2008). "Tamoxifen impairs both longitudinal and cortical bone growth in young male rats". Journal of Bone and Mineral Research. 23 (8): 1267–77. doi:10.1359/jbmr.080319. PMID 18348701. S2CID 35813153.
- ↑ Chagin AS, Karimian E, Zaman F, Takigawa M, Chrysis D, Sävendahl L (May 2007). "Tamoxifen induces permanent growth arrest through selective induction of apoptosis in growth plate chondrocytes in cultured rat metatarsal bones". Bone. 40 (5): 1415–24. doi:10.1016/j.bone.2006.12.066. PMID 17293177.
- ↑ van Bommel EF, Hendriksz TR, Huiskes AW, Zeegers AG (January 2006). "Brief communication: tamoxifen therapy for nonmalignant retroperitoneal fibrosis". Annals of Internal Medicine. 144 (2): 101–6. doi:10.7326/0003-4819-144-2-200601170-00007. PMID 16418409. S2CID 25699557.
- ↑ Akram S, Pardi DS, Schaffner JA, Smyrk TC (May 2007). "Sclerosing mesenteritis: clinical features, treatment, and outcome in ninety-two patients". Clinical Gastroenterology and Hepatology. 5 (5): 589–96, quiz 523–4. doi:10.1016/j.cgh.2007.02.032. PMID 17478346.
- ↑ Dabelic N, Jukic T, Labar Z, Novosel SA, Matesa N, Kusic Z (April 2003). "Riedel's thyroiditis treated with tamoxifen" (PDF). Croatian Medical Journal. 44 (2): 239–41. PMID 12698518. Archived (PDF) from the original on 2008-09-10.
- ↑ Feil R, Brocard J, Mascrez B, LeMeur M, Metzger D, Chambon P (October 1996). "Ligand-activated site-specific recombination in mice". Proceedings of the National Academy of Sciences of the United States of America. 93 (20): 10887–90. Bibcode:1996PNAS...9310887F. doi:10.1073/pnas.93.20.10887. PMC 38252. PMID 8855277.
- 1 2 3 Talaei A, Pourgholami M, Khatibi-Moghadam H, Faridhosseini F, Farhoudi F, Askari-Noghani A, Sadeghi R (June 2016). "Tamoxifen: A Protein Kinase C Inhibitor to Treat Mania: A Systematic Review and Meta-Analysis of Randomized, Placebo-Controlled Trials". Journal of Clinical Psychopharmacology. 36 (3): 272–5. doi:10.1097/JCP.0000000000000492. PMID 27088436. S2CID 39792641.
- 1 2 Saxena A, Scaini G, Bavaresco DV, Leite C, Valvassori SS, Carvalho AF, Quevedo J (November 2017). "Role of Protein Kinase C in Bipolar Disorder: A Review of the Current Literature". Molecular Neuropsychiatry. 3 (2): 108–124. doi:10.1159/000480349. PMC 5701269. PMID 29230399.
- ↑ "Endoxifen - Intas Pharmaceuticals/Jina pharmaceuticals - AdisInsight". Archived from the original on 2020-02-25. Retrieved 2019-09-03.
- ↑ Shagufta, Ahmad I (January 2018). "Tamoxifen a pioneering drug: An update on the therapeutic potential of tamoxifen derivatives". Eur J Med Chem. 143: 515–531. doi:10.1016/j.ejmech.2017.11.056. PMID 29207335.
Further reading
- Dean L (2014). "Tamoxifen Therapy and CYP2D6 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520357. Bookshelf ID: NBK247013. Archived from the original on 2020-10-26. Retrieved 2020-02-07.
External links
| External sites: |
|
|---|---|
| Identifiers: |