Tasimelteon
 | |
 | |
| Names | |
|---|---|
| Trade names | Hetlioz, Hetlioz LQ |
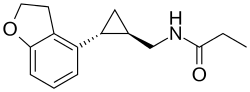
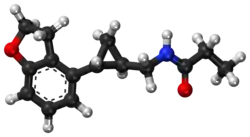
IUPAC name
| |
| Clinical data | |
| Drug class | Melatonin receptor agonist[1] |
| Main uses | Non-24-hour sleep–wake disorder[1] |
| Side effects | Headache, sleepiness, nausea, dizziness[2] |
| Dependence risk | None[1] |
| Addiction risk | None[1] |
| Pregnancy category |
|
| Routes of use | By mouth |
| Typical dose | 20 mg OD[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| US NLM | Tasimelteon |
| MedlinePlus | a615004 |
| Legal | |
| License data |
|
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | not determined in humans[3] |
| Protein binding | 89–90% |
| Metabolism | extensive liver, primarily CYP1A2 and CYP3A4-mediated |
| Elimination half-life | 0.9–1.7 h / 0.8–5.9 h (terminal) |
| Excretion | 80% in urine, 4% in feces |
| Chemical and physical data | |
| Formula | C15H19NO2 |
| Molar mass | 245.322 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Tasimelteon, sold under the brand name Hetlioz among others, is a medication used to treat non-24-hour sleep–wake disorder.[1] It is taken by mouth, an hour before bedtime.[1][2] Benefits may take months to occur.[1]
Common side effects include headache, sleepiness, nausea, and dizziness.[2] Safety in pregnancy is unclear.[1] It works by activating the melatonin receptor.[2]
Tasimelteon was approved for medical use in the United States in 2014 and Europe in 2015.[1][2] In the United States it costs about 23,000 USD per month as of 2021.[4] Despite being approved in Europe and available in Germany it is not sold in the United Kingdom as of 2021.[5]
Medical uses
In the US, tasimelteon is used for the treatment of non-24-hour sleep–wake disorder (Non-24) in adults and for the treatment of nighttime sleep disturbances in Smith-Magenis Syndrome (SMS) in people sixteen years of age and older.[6] Tasimelteon oral suspension is indicated for the treatment of nighttime sleep disturbances in SMS in children from 3 to 15 years of age.[6]
In Europe, tasimelteon capsules are indicated for the treatment of non-24-hour sleep–wake disorder (Non-24) in totally blind adults.[2]
As a treatment for N24HSWD, as with melatonin or other melatonin derivatives, people may experience improved sleep timing while taking the drug. Reversion to baseline sleep performance occurs within a month of discontinuation.[7]
Dosage
The typical dose is 20 mg taken once per day.[1]
The capsule and liquid suspension forms of tasimelteon are not interchangeable.[6]
Side effects
Experiments with rodents revealed fertility impairments, an increase in certain cancers, and serious adverse events during pregnancy at dosages in excess of what is considered the "human dose".[8][9]
Mechanism of action
Tasimelteon is a selective agonist for the melatonin receptors MT1 and MT2, similar to other members of the melatonin receptor agonist class of which ramelteon (2005) and agomelatine (2009) were the first approved.[10]
History
Tasimelteon (previously known as BMS-214,778) was developed for the treatment of insomnia and other sleep disorders. A phase II trial on circadian rhythm sleep disorders was concluded in March 2005.[11] A phase III insomnia trial was conducted in 2006.[12] A second phase III trial on insomnia, this time concerning primary insomnia, was completed in June 2008.[13] In 2010, the FDA granted orphan drug status to tasimelteon, then regarded as an investigational medication, for use in totally blind adults with N24HSWD.[14] (Through mechanisms such as easing the approval process and extending exclusivity periods, orphan drug status encourages development of drugs for rare conditions that otherwise might lack sufficient commercial incentive.)
On completion of Phase III trials, interpretations of the clinical trials by the research team concluded that the drug may have therapeutic potential for transient insomnia in circadian rhythm sleep disorders.[15] A year-long (2011–2012) study at Harvard tested the use of tasimelteon in blind subjects with non-24-hour sleep-wake disorder. The drug has not been tested in children nor in any non-blind people.
Approval
In 2013, Vanda Pharmaceuticals submitted a New Drug Application to the Food and Drug Administration for the treatment of non-24-hour sleep–wake disorder in totally blind people. It was approved by the FDA on January 31, 2014 under the brand name Hetlioz.[16] In the opinion of Public Citizen, an advocacy group, the FDA erroneously allowed it to be labelled without stating that it is only approved for use by totally blind people.[17] However, FDA updated its press release on Oct. 2, 2014 to clarify the approved use of Hetlioz, which includes both sighted and blind individuals. The update did not change the drug labeling (prescribing information).[18]
References
- 1 2 3 4 5 6 7 8 9 10 11 "Tasimelteon Monograph for Professionals". Drugs.com. Archived from the original on 4 November 2020. Retrieved 22 September 2021.
- 1 2 3 4 5 6 "Hetlioz EPAR". European Medicines Agency (EMA). Archived from the original on 3 November 2020. Retrieved 2 December 2020.
- ↑ "Tasimelteon Advisory Committee Meeting Briefing Materials" (PDF). Vanda Pharmaceuticals Inc. November 2013. Archived (PDF) from the original on 2013-11-25. Retrieved 2020-12-03.
- ↑ "Hetlioz Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 13 August 2021. Retrieved 22 September 2021.
- ↑ "Tasimelteon". SPS - Specialist Pharmacy Service. Archived from the original on 30 November 2020. Retrieved 22 September 2021.
- 1 2 3 "Hetlioz- tasimelteon capsule". DailyMed. Archived from the original on 2021-03-26. Retrieved 2020-12-03.
- ↑ Sack RL, Brandes RW, Kendall AR, Lewy AJ (October 2000). "Entrainment of free-running circadian rhythms by melatonin in blind people". The New England Journal of Medicine. 343 (15): 1070–7. doi:10.1056/NEJM200010123431503. PMID 11027741.
- ↑ "Side Effects Drug Center: Hetlioz Clinical Pharmacology". RxList. February 10, 2014. Archived from the original on October 27, 2016. Retrieved December 3, 2020.
- ↑ "Side Effects Drug Center: Hetlioz Warnings and Precautions". RxList. February 10, 2014. Archived from the original on October 27, 2016. Retrieved December 3, 2020.
In animal studies, administration of tasimelteon during pregnancy resulted in developmental toxicity (embryofetal mortality, neurobehavioral impairment, and decreased growth and development in offspring) at doses of up to 200 times greater than those used clinically.
- ↑ Vachharajani NN, Yeleswaram K, Boulton DW (April 2003). "Preclinical pharmacokinetics and metabolism of BMS-214778, a novel melatonin receptor agonist". Journal of Pharmaceutical Sciences. 92 (4): 760–72. doi:10.1002/jps.10348. PMID 12661062.
- ↑ Clinical trial number NCT00490945 for "Safety and Efficacy of VEC-162 on Circadian Rhythm in Healthy Adult Volunteers" at ClinicalTrials.gov
- ↑ Clinical trial number NCT00291187 for "VEC-162 Study in Healthy Adult Volunteers in a Model of Insomnia" at ClinicalTrials.gov
- ↑ Clinical trial number NCT00548340 for "VEC-162 Study in Adult Patients With Primary Insomnia" at ClinicalTrials.gov
- ↑ Lamberg L. "Improving Sleep and Alertness in the Blind (Part 5)". Matilda Ziegler Magazine for the Blind. Archived from the original on September 15, 2015. Retrieved May 15, 2014.
- ↑ Rajaratnam SM, Polymeropoulos MH, Fisher DM, Roth T, Scott C, Birznieks G, Klerman EB (February 2009). "Melatonin agonist tasimelteon (VEC-162) for transient insomnia after sleep-time shift: two randomised controlled multicentre trials". Lancet. 373 (9662): 482–91. doi:10.1016/S0140-6736(08)61812-7. PMID 19054552. S2CID 36568291.
- ↑ Food and Drug Administration (January 31, 2014). "FDA approves Hetlioz: first treatment for non-24 hour sleep-wake disorder" (Press release). FDA. Archived from the original on February 2, 2014. Retrieved December 3, 2020.
- ↑ Carome M (1 July 2015). "Outrage of the Month: FDA Makes Major Blunder After Approving Drug for Rare Sleep Disorder". Huffington Post. Archived from the original on 4 July 2015. Retrieved 8 July 2015.
- ↑ Food and Drug Administration (January 31, 2014). "FDA NEWS RELEASE: FDA approves Hetlioz: first treatment for non-24 hour sleep–wake disorder in blind individuals". FDA. Archived from the original on February 2, 2014. Retrieved December 3, 2020.
External links
| External sites: |
|
|---|---|
| Identifiers: |
|