Acute limb ischaemia
| Acute limb ischaemia | |
|---|---|
| Other names: Acute limb ischemia, acute arterial occlusion | |
 | |
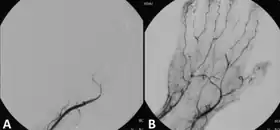
| Acute embolism to the right femoral artery resulting in ischemia | |
| Specialty | Vascular surgery |
| Symptoms | Pale, painful, numb, immobile, pulseless, cool limb[1] |
| Complications | Compartment syndrome[1] |
| Usual onset | Hours to days[2] |
| Types | Stage I, IIa, IIb, III[3] |
| Causes | Thrombosis, embolism, dissection, trauma[2] |
| Risk factors | Smoking, diabetes, obesity, sedentary lifestyle, family history, high cholesterol, high blood pressure, atrial fibrillation[1][2] |
| Diagnostic method | Based on symptoms, confirmed by CT angiogram[1] |
| Differential diagnosis | Chronic limb ischemia[2] |
| Treatment | Surgery, thrombolysis[1] |
| Medication | Unfractionated heparin, pain management[1] |
| Frequency | 15 to 22 per 100,000 per year[1][3] |
Acute limb ischaemia (ALI) occurs when there is a sudden decrease in blood flow to a limb.[3] Symptoms classically include a pale, painful, numb, immobile, pulseless, and cool limb.[1] While any limb may be involves, the legs are most commonly affected.[1] Complications may include compartment syndrome.[1]
The most common cause is a thrombosis, often in the setting of peripheral artery disease (PAD).[1] Other causes may include embolism, dissection, or trauma.[2] Risk factors include smoking, diabetes, obesity, sedentary lifestyle, family history, high cholesterol, and high blood pressure.[1] Diagnosis may be suspected based on symptoms and confirmed by CT angiogram.[1] In contrast, chronic limb threatening ischemia develops more gradually, and while there may be no pulse, symptoms are present for more than 2 weeks.[4]
Treatment is generally by prompt surgery; which may include surgical bypass, endarterectomy, or embolectomy.[1] Catheter-directed thrombolysis may be another option.[1] While awaiting surgery unfractionated heparin and pain management is frequently provided.[1] If treatment is delayed amputation may be required.[1] About 15% of people die within a year, often due to associated health problems.[2]
ALI occur in about 15 to 22 per 100,000 people per year.[1][3] Males and females are affected equally frequently.[1] The typical age of onset is 75.[1] Successful surgery to manage acute limb ischemia was first performed in 1911.[5] The word ischemia is from the Greek ischein meaning "to hold" and haima meaning "blood".[6]
Signs and symptoms
Symptoms of acute limb ischaemia include:
- Pain
- Pallor (pale appearance of the limb)
- Paresthesias (abnormal sensations in the limb)
- Perishingly cold
- Pulselessness
- Paralysis
These symptoms are called "the six P's'";[7][8][9] they are commonly mis-attributed to compartment syndrome. One more symptom would be the development of gangrene. Immediate medical attention should be sought with any of the symptoms.[10]
In late stages, paresthesia is replaced by anesthesia (numbness) due to death of nerve cells.
In some cases, gangrene can occur within six hours of ischaemia.
Related conditions
When a limb is ischaemic in the non-acute (chronic) setting, the condition is alternatively called peripheral artery disease or critical limb ischaemia, rather than ALI. In addition to limb ischaemia, other organs can become ischaemic, causing:
- Renal ischemia (nephric ischaemia)
- Mesenteric ischaemia
- Cerebral ischaemia
- Cardiac ischaemia
Cause
People who smoke tobacco cigarettes and have diabetes mellitus are at a higher risk of developing acute limb ischaemia. Most cases involve people with atherosclerosis problems.[11]
The major cause of acute limb ischaemia is arterial embolism (80%), while arterial thrombosis is responsible for 20% of cases. In rare instances, arterial aneurysm of the popliteal artery has been found to create a blood clot or embolism resulting in ischaemia.[12]
Diagnosis

In order to treat acute limb ischaemia there are a series of things that can be done to determine where the occlusion is located, the severity, and what the cause was. To find out where the occlusion is located one of the things that can be done is simply a pulse examination to see where the heart rate can be detected and where it stops being sensed. Also there is a lower body temperature below the occlusion as well as paleness. A Doppler evaluation is used to show the extent and severity of the ischaemia by showing flow in smaller arteries. Other diagnostical tools are duplex ultrasonography, computed tomography angiography (CTA), and magnetic resonance angiography (MRA). The CTA and MRA are used most often because the duplex ultrasonography although non-invasive is not precise in planning revascularization. CTA uses radiation and may not pick up on vessels for revascularization that are distal to the occlusion, but it is much quicker than MRA.[10] In treating acute limb ischaemia time is everything.
Differential
In contrast, chronic limb threatening ischemia develops gradually, and while there may be no pulse, the limb is typically warm and pink due to developed collateral arteries. It may not need emergency intervention, but surgery should be timely.[4]
Treatment
Treatment depends on many factors, including:[13]
- Location of lesions
- Anatomy of lesions
- Individual risk factors
- Procedural risk
- Presentation of symptoms
- Duration of symptoms
Surgery
The primary intervention in acute limb ischaemia is emergency embolectomy using a Fogarty Catheter, providing the limb is still viable within the 4-6h timeframe.[14] Other options include a vascular bypass to route blood flow around the clot.[15]
Medication
Those unsuitable for surgery may receive thrombolytics. In the past, streptokinase was the main thrombolytic chemical. More recently, drugs such as tissue plasminogen activator, urokinase, and anisterplase have been used in its place. Mechanical methods of injecting the thrombolytic compounds have improved with the introduction of pulsed spray catheters—which allow for a greater opportunity for patients to avoid surgery.[13][16] Pharmacological thrombolysis requires a catheter to be inserted into the affected area, attached to the catheter is often a wire with holes to allow for a wider dispersal area of the thrombolytic agent. These agents lyse the ischemia-causing thrombus quickly and effectively.[17] However, the efficacy of thrombolytic treatment is limited by hemorrhagic complications. Plasma fibrinogen level has been proposed as a predictor of these hemorrhagic complications. However, based on a systematic review of the available literature until January 2016, the predictive value of plasma is unproven.[18]
Mechanical thrombolysis
Another type of thrombolysis disrupts the clot mechanically using either saline jets or, more recently, ultrasound waves. Saline jets dislodge the clot using the Bernoulli effect. Ultrasound waves, emitted at low frequency, create a physical fragmentation of the thrombus.[19]
Outcomes
In the worst cases acute limb ischaemia results in death or limb loss. Early detection and steps towards fixing the problem with limb-sparing techniques can salvage the limb. Compartment syndrome can occur because of acute limb ischaemia because of the biotoxins that accumulate distal to the occlusion resulting in edema.[10]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Smith, DA; Lilie, CJ (January 2021). "Acute Arterial Occlusion". PMID 28722881.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 Creager, Mark A.; Kaufman, John A.; Conte, Michael S. (2012). "Acute Limb Ischemia". New England Journal of Medicine. 366 (23): 2198–2206. doi:10.1056/NEJMcp1006054. PMID 22670905.
- 1 2 3 4 Santistevan, JR (November 2017). "Acute Limb Ischemia: An Emergency Medicine Approach". Emergency medicine clinics of North America. 35 (4): 889–909. doi:10.1016/j.emc.2017.07.006. PMID 28987435.
- 1 2 Farber, A (12 July 2018). "Chronic Limb-Threatening Ischemia". The New England Journal of Medicine. 379 (2): 171–180. doi:10.1056/NEJMcp1709326. PMID 29996085.
- ↑ Lanzer, Peter; Topol, Eric J. (2002). Pan Vascular Medicine: Integrated Clinical Management. Springer Science & Business Media. p. 1353. ISBN 978-3-540-41484-1. Archived from the original on 2021-08-27. Retrieved 2021-03-04.
- ↑ "Definition of ISCHEMIA". www.merriam-webster.com. Archived from the original on 23 September 2020. Retrieved 4 March 2021.
- ↑ Brearley, S (May 8, 2013). "Acute leg ischaemia". BMJ (Clinical Research Ed.). 346: f2681. doi:10.1136/bmj.f2681. PMID 23657181.
- ↑ "CKS is only available in the UK". NICE. Archived from the original on 2016-09-18. Retrieved 2020-10-15.
- ↑ "Acute Limb Ischaemia - Clinical Features - Management". TeachMeSurgery. Archived from the original on 2020-09-25. Retrieved 2020-10-15.
- 1 2 3 Walker T. Gregory (2009). "Acute Limb Ischemia". Techniques in Vascular and Interventional Radiology. 12 (2): 117–129. doi:10.1053/j.tvir.2009.08.005. PMID 19853229.
- ↑ Brooks Marcus; Jenkins Michael P (2008). "Acute and chronic ischaemia of the limb". Surgery (Oxford). 26 (1): 17–20. doi:10.1016/j.mpsur.2007.10.012.
- ↑ Mitchell ME, Carpenter JP. Overview of acute arterial occlusion of the extremities (acute limb ischemia). In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. https://www.uptodate.com/contents/overview-of-acute-arterial-occlusion-of-the-extremities-acute-limb-ischemia?source=search_result&search=Classification%20of%20acute%20extremity%20ischemia&selectedTitle=1∼90#H506059593 Archived 2021-08-27 at the Wayback Machine. Last updated May 31, 2016. Accessed December 13, 2016.
- 1 2 Andaz S.; Shields D.A.; Scurr J.H.; Smith P.D. Coleridge (1993). "Thrombolysis in acute lower limb ischaemia". European Journal of Vascular Surgery. 7 (6): 595–603. doi:10.1016/S0950-821X(05)80702-9. PMID 8270059.
- ↑ Goldberg, Andrew (2012). Surgical Talk: Lecture Notes in Undergraduate Surgery. Imperial College Press. p. 234. ISBN 978-1-84816-6141.
- ↑ Bowley, Douglas, and Andrew Kingsnorth, eds. Fundamentals of Surgical Practice: A Preparation Guide for the Intercollegiate Mrcs Examination. 3rd ed. N.p.: Cambridge University Press, 2011. 506-11. Web. 20 Apr. 2012.
- ↑ ABC of Arterial and Venous Disease: Acute Limb Ischaemia Ken Callum and Andrew Bradbury BMJ: British Medical Journal, Vol. 320, No. 7237 (Mar. 18, 2000), pp. 764-767
- ↑ Wardlaw J.M.; Warlow C.P. (1992). "Thrombolysis in acute ischemic stroke: does it work?". Stroke. 23 (12): 1826–1839. doi:10.1161/01.str.23.12.1826.
- ↑ Poorthuis, Michiel H. F.; Brand, Eelco C.; Hazenberg, Constantijn E. V. B.; Schutgens, Roger E. G.; Westerink, Jan; Moll, Frans L.; de Borst, Gert J. (2017-03-05). "Plasma fibrinogen level as a potential predictor of hemorrhagic complications after catheter-directed thrombolysis for peripheral arterial occlusions". Journal of Vascular Surgery. 65 (5): 1519–1527.e26. doi:10.1016/j.jvs.2016.11.025. ISSN 1097-6809. PMID 28274749.
- ↑ Sean P. Lyden, Endovascular Treatment of Acute Limb Ischemia: Review of Current Plasminogen Activators and Mechanical Thrombectomy Devices PERSPECT VASC SURG ENDOVASC THER December 2010 22: 219-222, first published on March 16, 2011
External links
| Classification |
|---|