Aedes aegypti
| Yellow fever mosquito | |
|---|---|
 | |
| Adult | |
 | |
| Larva | |
| Scientific classification | |
| Kingdom: | Animalia |
| Phylum: | Arthropoda |
| Class: | Insecta |
| Order: | Diptera |
| Family: | Culicidae |
| Genus: | Aedes |
| Subgenus: | Stegomyia |
| Species: | A. aegypti |
| Binomial name | |
| Aedes aegypti (Linnaeus in Hasselquist, 1762) [1] | |
.png.webp) | |
| Global Aedes aegypti predicted distribution in 2015, (blue=absent, red=present) | |
| Synonyms[1] | |
| |
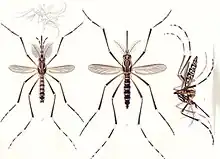
Aedes aegypti, the yellow fever mosquito, is a mosquito that can spread dengue fever, chikungunya, Zika fever, Mayaro and yellow fever viruses, and other disease agents. The mosquito can be recognized by white markings on its legs and a marking in the form of a lyre on the upper surface of its thorax. This mosquito originated in Africa,[2] but is now found in tropical, subtropical and temperate regions[3] throughout the world.[4]
Spread of disease and prevention methods
Aedes aegypti is a vector for transmitting several tropical fevers. Only the female bites for blood, which she needs to mature her eggs. To find a host, these mosquitoes are attracted to chemical compounds emitted by mammals, including ammonia[5] carbon dioxide[6] lactic acid, and octenol.[7] Scientists at The United States Department of Agriculture (USDA) Agricultural Research Service have studied the specific chemical structure of octenol to better understand why this chemical attracts the mosquito to its host.[8] They found the mosquito has a preference for "right-handed" (dextrorotatory) octenol molecules.
The yellow fever mosquito can also contribute to the spread of reticular cell sarcoma among Syrian hamsters.[9]
The Centers for Disease Control and Prevention traveler's page on preventing dengue fever suggests using mosquito repellents that contain DEET (N, N-diethylmetatoluamide, 20% to 30%). It also suggests:
- Although Aedes aegypti mosquitoes most commonly feed at dusk and dawn, indoors, in shady areas, or when the weather is cloudy, "they can bite and spread infection all year long and at any time of day."[10][11]
- Once a week, scrub off eggs sticking to wet containers, seal and/or discard them. The mosquitoes prefer to breed in areas of stagnant water, such as flower vases, uncovered barrels, buckets, and discarded tires, but the most dangerous areas are wet shower floors and toilet tanks, as they allow the mosquitos to breed in the residence. Research has shown that certain chemicals emanating from bacteria in water containers stimulate the female mosquitoes to lay their eggs. They are particularly motivated to lay eggs in water containers that have the correct amounts of specific fatty acids associated with bacteria involved in the degradation of leaves and other organic matter in water. The chemicals associated with the microbial stew are far more stimulating to discerning female mosquitoes than plain or filtered water in which the bacteria once lived.[12]
- Wear long-sleeved clothing and long trousers when outdoors during the day and evening.
- Use mosquito netting over the bed if the bedroom is not air conditioned or screened, and for additional protection, treat the mosquito netting with the insecticide permethrin.
Insect repellents containing DEET (particularly concentrated products) or p-menthane-3,8-diol (from lemon eucalyptus) were effective in repelling Ae. aegypti mosquitoes, while others were less effective or ineffective in a scientific study.[13] The Centers for Disease Control and Prevention article on "Protection against Mosquitoes, Ticks, & Other Arthropods" notes that "Studies suggest that concentrations of DEET above approximately 50% do not offer a marked increase in protection time against mosquitoes; DEET efficacy tends to plateau at a concentration of approximately 50%".[14] Other insect repellents recommended by the CDC include Picaridin (KBR 3023/icaridin), IR3535, and 2-undecanone.[15]
Although the lifespan of an adult Ae. aegypti is two to four weeks depending on conditions,[16] the eggs can be viable for over a year in a dry state, which allows the mosquito to re-emerge after a cold winter or dry spell.[17]
The preference for biting humans is dependent on expression of the odorant receptor AaegOr4.[18]
New research is looking into the use of a bacterium called Wolbachia as a method of biocontrol. Studies show that invasion of Ae. aegypti by the endosymbiotic bacteria allows mosquitos to be resistant to the certain arboviruses such as dengue fever and Zika virus strains currently circulating.[19][20]
Distribution
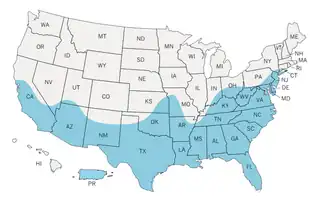
The yellow fever mosquito's distribution has increased in the past two to three decades worldwide, and it is considered to be among the most widespread mosquito species.[21] Signs of Zika virus-capable mosquito populations have been found adapting for persistence in warm temperate climates. Such a population has been identified to exist in parts of Washington, DC, and genetic evidence suggests they survived at least the last four winters in the region. One of the study researchers noted, " ...some mosquito species are finding ways to survive in normally restrictive environments by taking advantage of underground refugia".[22] As the world's climate becomes predictably warmer, the range of Aedes aegypti and a hardier species originating in Asia, the tiger mosquito Aedes albopictus, which can expand its range to relatively cooler climates, will inexorably spread north and south. Sadie Ryan of the University of Florida was the lead author in a 2019 study published in PLOS Neglected Tropical Diseases that estimated the vulnerability of naïve populations in geographic regions that currently do not harbor vectors i.e., for Zika in the Old World. Ryan's co-author, Georgetown University's Colin Carlson remarked,"Plain and simple, climate change is going to kill a lot of people."[23] The Northern Territory Government Australia and the Darwin City Council have recommended tropical cities initiate rectification programs to rid their cities of potential mosquito breeding stormwater sumps.[24] A 2019 study published in Nature Microbiology found that accelerating urbanization and human movement would also contribute to the spread of Aedes mosquitoes.[25]
Population control efforts
Insecticides
Pyrethroids are commonly used.[26]
Insecticide resistance
Knockdown resistance (kdr) mutations are common due to widespread use of pyrethroids and DDT. Despite the widespread use of pyrethroids and therefore the importance of kdr almost no research has been done on the fitness implications. There have been studies by Alvarez-Gonzalez et al 2017 on deltamethrin in Venezuela, Jaramillo-O et al 2014 on λ-cyhalothrin in Colombia, Kumar et al 2009 on deltamethrin in India and Plernsub et al 2013 on permethrin in Thailand however these are all substantially confounded. This leaves us especially without an understanding of selective pressure under withdrawal of insecticide.[26]
Genetic modification
Ae. aegypti has been genetically modified to suppress its own species in an approach similar to the sterile insect technique, thereby reducing the risk of disease. The mosquitoes, known as OX513A, were developed by Oxitec, a spinout of Oxford University. Field trials in the Cayman Islands, Jacobina (a municipality in Brazil), and Panama have shown that the OX513A mosquitoes reduced the target mosquito populations by more than 90%.[27][28] This mosquito suppression effect is achieved by a self-limiting gene that prevents the offspring from surviving. Male modified mosquitoes, which do not bite or spread disease, are released to mate with the pest females. Their offspring inherit the self-limiting gene and die before reaching adulthood—before they can reproduce or spread disease. The OX513A mosquitoes and their offspring also carry a fluorescent marker for simple monitoring. To produce more OX513A mosquitoes for control projects, the self-limiting gene is switched off (using the Tet-Off system) in the mosquito production facility using an antidote (the antibiotic tetracycline), allowing the mosquitoes to reproduce naturally. In the environment, the antidote is unavailable to rescue mosquito reproduction, so the pest population is suppressed.[29]
The mosquito control effect is nontoxic and species-specific, as the OX513A mosquitoes are Ae. aegypti and only breed with Ae. aegypti. The result of the self-limiting approach is that the released insects and their offspring die and do not persist in the environment.[30][31]
In Brazil, the modified mosquitoes were approved by the National Biosecurity Technical Commission for releases throughout the country. Insects were released into the wild populations of Brazil, Malaysia, and the Cayman Islands in 2012.[32][33] In July 2015, the city of Piracicaba, São Paulo, started releasing the OX513A mosquitoes.[34][35] In 2015, the UK House of Lords called on the government to support more work on genetically modified insects in the interest of global health.[36] In 2016, the United States Food and Drug Administration granted preliminary approval for the use of modified mosquitoes to prevent the spread of the Zika virus.[37]
This approach could also be applied to control Aedes albopictus and the Anopheles mosquitoes that spread malaria.[38]
Another proposed method consists in using radiation to sterilize male larvae so that when they mate, they produce no progeny.[39] Male mosquitoes do not bite or spread disease.
Alphabet, Inc. has started the Debug Project to infect males of this species with Wolbachia bacteria, interrupting the reproductive cycle of these animals.[40]
The recent invention of CRISPR/Cas9 based genome editing tool have significantly expanded the scope of genome editing research in Aedes aegypti mosquito. Several scientists across the globe have already attempted this technique to engineer the genome of vector mosquitoes. The genes like ECFP (enhanced cyan fluorescent protein), Nix (male-determining factor gene), Aaeg-wtrw (Ae. aegypti water witch locus), Kmo (kynurenine 3-monoxygenase), loqs (loquacious), r2d2 (r2d2 protein), ku70 (ku heterodimer protein gene) and lig4 (ligase4) were targeted to modify the genome of Aedes aegypti using CRISPR/Cas9 tool to obtain a new mutant, which will become incapable of pathogen transmission or result in population control.[41]
Genomics
The genome of this species of insect was sequenced and analyzed by a consortium including scientists at The Institute for Genomic Research (now part of the J. Craig Venter Institute), the European Bioinformatics Institute, the Broad Institute, and the University of Notre Dame, and published in 2007. The effort in sequencing its DNA was intended to provide new avenues for research into insecticides and possible genetic modification to prevent the spread of virus. This was the second mosquito species to have its genome sequenced in full (the first was Anopheles gambiae). The published data included the 1.38 billion base pairs containing the insect's estimated 15,419 protein-encoding genes. The sequence indicates the species diverged from Drosophila melanogaster (the common fruit fly) about 250 million years ago, and Anopheles gambiae and this species diverged about 150 million years ago.[42][43] Matthews et al 2018 finds A. aegypti to carry a large and diverse number of transposable elements. Their analysis suggests this is common to all mosquitoes.[44]
Hosts
Hosts include domesticated horses, and feral and wild horses and equids more generally. A. aegypti is a vector of African horse sickness to all equids.[45] Birds are also hosts.[46] Lyimo and Ferguson 2009 find birds to be the best food supply for Ae. aegypti among all taxa.[46]
Scientific name
The species was first named (as Culex aegypti) in 1757 by Fredric Hasselquist in his treatise Iter Palaestinum.[47] Hasselquist was provided with the names and descriptions by his mentor, Carl Linnaeus. This work was later translated into German and published in 1762 as Reise nach Palästina.[48] Since the latter is an uncritical reproduction of the former, they are both considered to antedate the starting point for zoological nomenclature in 1758. Nonetheless, the name Aedes aegypti was frequently used, starting with H. G. Dyar in 1920.

To stabilise the nomenclature, a petition to the International Commission on Zoological Nomenclature was made by P. F. Mattingly, Alan Stone, and Kenneth L. Knight in 1962.[49] It also transpired that, although the name Aedes aegypti was universally used for the yellow fever mosquito, Linnaeus had actually described a species now known as Aedes (Ochlerotatus) caspius.[49] In 1964, the commission ruled in favour of the proposal, validating Linnaeus' name, and transferring it to the species for which it was in general use.[50]
The yellow fever mosquito belongs to the tribe Aedini of the dipteran family Culicidae and to the genus Aedes and subgenus Stegomyia. According to one recent analysis, the subgenus Stegomyia of the genus Aedes should be raised to the level of genus.[51] The proposed name change has been ignored by most scientists;[52] at least one scientific journal, the Journal of Medical Entomology, has officially encouraged authors dealing with aedile mosquitoes to continue to use the traditional names, unless they have particular reasons for not doing so.[53] The generic name comes from the Ancient Greek ἀηδής, aēdēs, meaning "unpleasant"[54] or "odious".
References
- 1 2 Neal L. Evenhuis; Samuel M. Gon III (2007). "22. Family Culicidae" (PDF). In Neal L. Evenhuis (ed.). Catalog of the Diptera of the Australasian and Oceanian Regions. Bishop Museum. pp. 191–218. Retrieved February 4, 2012.
- ↑ Laurence Mousson; Catherine Dauga; Thomas Garrigues; Francis Schaffner; Marie Vazeille; Anna-Bella Failloux (August 2005). "Phylogeography of Aedes (Stegomyia) aegypti (L.) and Aedes (Stegomyia) albopictus (Skuse) (Diptera: Culicidae) based on mitochondrial DNA variations". Genetics Research. 86 (1): 1–11. doi:10.1017/S0016672305007627. PMID 16181519.
- ↑ Eisen, L.; Moore, C. G. (2013). "Aedes (Stegomyia) aegypti in the Continental United States: A Vector at the Cool Margin of Its Geographic Range". Journal of Medical Entomology. 50 (3): 467–478. doi:10.1603/ME12245. PMID 23802440.
- ↑ M. Womack (1993). "The yellow fever mosquito, Aedes aegypti". Wing Beats. 5 (4): 4.
- ↑ Geier, Martin; Bosch, Oliver J.; Boeckh, Jürgen (1 December 1999). "Ammonia as an Attractive Component of Host Odour for the Yellow Fever Mosquito, Aedes aegypti". Chemical Senses. 24 (6): 647–653. doi:10.1093/chemse/24.6.647. ISSN 0379-864X. PMID 10587497.
- ↑ Ghaninia, Majid; Majeed, Shahid; Dekker, Teun; Hill, Sharon R.; Ignell, Rickard (30 December 2019). "Hold your breath – Differential behavioral and sensory acuity of mosquitoes to acetone and carbon dioxide". PLOS ONE. 14 (12): e0226815. doi:10.1371/journal.pone.0226815. ISSN 1932-6203. PMC 6936819. PMID 31887129.
- ↑ Bohbot, Jonathan D.; Durand, Nicolas F.; Vinyard, Bryan T.; Dickens, Joseph C. (2013). "Functional Development of the Octenol Response in Aedes aegypti". Frontiers in Physiology. 4: 39. doi:10.3389/fphys.2013.00039. PMC 3590643. PMID 23471139.
- ↑ Dennis O'Brien (March 9, 2010). "ARS Study Provides a Better Understanding of How Mosquitoes Find a Host". U.S. Department of Agriculture. Archived from the original on 8 October 2010. Retrieved 2010-08-27.
- ↑ Banfield, William G.; Woke, P. A.; MacKay, C. M.; Cooper, H. L. (28 May 1965). "Mosquito Transmission of a Reticulum Cell Sarcoma of Hamsters". Science. 148 (3674): 1239–1240. Bibcode:1965Sci...148.1239B. doi:10.1126/science.148.3674.1239. PMID 14280009. S2CID 12611674.
- ↑ "Travelers' Health Outbreak Notice". Centers for Disease Control and Prevention. June 2, 2010. Archived from the original on 26 August 2010. Retrieved 2010-08-27.
- ↑ "Dengue Virus: Vector And Transmission". 2009-08-07. Retrieved 19 October 2012.
- ↑ "Lay Your Eggs Here". Newswise, Inc. July 3, 2008. Retrieved 2010-08-27.
- ↑ Rodriguez Stacy D.; Drake Lisa L.; Price David P.; Hammond John I.; Hansen Immo A. (2015). "The Efficacy of Some Commercially Available Insect Repellents for Aedes aegypti (Diptera: Culicidae) and Aedes albopictus (Diptera: Culicidae)". Journal of Insect Science. 15: 140. doi:10.1093/jisesa/iev125. PMC 4667684. PMID 26443777.
- ↑ "Protection against Mosquitoes, Ticks, & Other Arthropods - Chapter 2 - 2016 Yellow Book | Travelers' Health | CDC". wwwnc.cdc.gov. Retrieved 2016-12-08.
- ↑ "Prevent Tick and Mosquito Bites | Division of Vector-Borne Diseases | NCEZID | CDC". www.cdc.gov. 2019-10-07. Retrieved 2020-04-30.
- ↑ Catherine Zettel; Phillip Kaufman. "Yellow fever mosquito Aedes aegypti". University of Florida, Institute of Food and Agricultural Sciences. Retrieved 2010-08-27.
- ↑ Roland Mortimer. "Aedes aegypti and dengue fever". Onview.net Ltd, Microscopy-UK. Retrieved 2010-08-27.
- ↑ McBride, Carolyn S.; Baier, Felix; Omondi, Aman B.; Spitzer, Sarabeth A.; Lutomiah, Joel; Sang, Rosemary; Ignell, Rickard; Vosshall, Leslie B. (12 November 2014). "Evolution of mosquito preference for humans linked to an odorant receptor". Nature. 515 (7526): 222–227. Bibcode:2014Natur.515..222M. doi:10.1038/nature13964. PMC 4286346. PMID 25391959.
- ↑ Dutra, HL; Rocha, MN; Dias, FB; Mansur, SB; Caragata, EP; Moreira, LA (June 8, 2016). "Wolbachia Blocks Currently Circulating Zika Virus Isolates in Brazilian Aedes aegypti Mosquitoes". Cell Host & Microbe. 19 (6): 771–774. doi:10.1016/j.chom.2016.04.021. PMC 4906366. PMID 27156023 – via PMC.
- ↑ Hancock, Penelope A.; White, Vanessa L.; Callahan, Ashley G.; Godfray, Charles H. J.; Hoffmann, Ary A.; Ritchie, Scott A.; Clough, Yann (June 2016). "Density‐dependent population dynamics in Aedes aegypti slow the spread of wMel Wolbachia". Journal of Applied Ecology. 53 (3): 785–793. doi:10.1111/1365-2664.12620.
- ↑ "Aedes aegypti". European Centre for Disease Prevention and Control.
- ↑ "Mosquitoes capable of carrying Zika virus found in Washington, D.C." University of Notre Dame. 2016.
- ↑ Climate Crisis Could Expose Half a Billion More People to Tropical Mosquito-Borne Diseases by 2050, Common Dreams, Jessica Corbett, March 29, 2019. Retrieved March 31, 2019.
- ↑ Warchot, Allan; Whelan, Peter; Brown, John; Vincent, Tony; Carter, Jane; Kurucz, Nina (2020). "The Removal of Subterranean Stormwater Drain Sumps as Mosquito Breeding Sites in Darwin, Australia". Tropical Medicine and Infectious Disease. 5 (1): 9. doi:10.3390/tropicalmed5010009. PMC 7157592. PMID 31936813.
- ↑ Kraemer, Moritz U. G.; Reiner, Robert C.; Brady, Oliver J.; Messina, Jane P.; Gilbert, Marius; Pigott, David M.; Yi, Dingdong; Johnson, Kimberly; Earl, Lucas; Marczak, Laurie B.; Shirude, Shreya; Davis Weaver, Nicole; Bisanzio, Donal; Perkins, T. Alex; Lai, Shengjie; Lu, Xin; Jones, Peter; Coelho, Giovanini E.; Carvalho, Roberta G.; Van Bortel, Wim; Marsboom, Cedric; Hendrickx, Guy; Schaffner, Francis; Moore, Chester G.; Nax, Heinrich H.; Bengtsson, Linus; Wetter, Erik; Tatem, Andrew J.; Brownstein, John S.; Smith, David L.; Lambrechts, Louis; Cauchemez, Simon; Linard, Catherine; Faria, Nuno R.; Pybus, Oliver G.; Scott, Thomas W.; Liu, Qiyong; Yu, Hongjie; Wint, G. R. William; Hay, Simon I.; Golding, Nick (4 March 2019). "Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus". Nature Microbiology. 4 (5): 854–863. doi:10.1038/s41564-019-0376-y. PMC 6522366. PMID 30833735.
- 1 2 Scott, Jeffrey G. (2019-01-07). "Life and Death at the Voltage-Sensitive Sodium Channel: Evolution in Response to Insecticide Use". Annual Review of Entomology. Annual Reviews. 64 (1): 243–257. doi:10.1146/annurev-ento-011118-112420. ISSN 0066-4170.
- ↑ Danilo O. Carvalho; Andrew R. McKemey; Luiza Garziera; Renaud Lacroix; Christl A. Donnelly; Luke Alphey; Aldo Malavasi; Margareth L. Capurro (July 2015). "Suppression of a Field Population of Ae. aegypti in Brazil by Sustained Release of Transgenic Male Mosquitoes". PLOS Neglected Tropical Diseases. 9 (7): e0003864. doi:10.1371/journal.pntd.0003864. PMC 4489809. PMID 26135160.
- ↑ Kate Kelland (16 December 2015). "Lawmakers call for British trials of genetically modified insects". Reuters. Retrieved 2015-12-16.
- ↑ Zoe Curtis; Kelly Matzen; Marco Neira Oviedo; Derric Nimmo; Pamela Gray; Peter Winskill; Marco A. F. Locatelli; Wilson F. Jardim; Simon Warner; Luke Alphey; Camilla Beech (August 2015). "Assessment of the Impact of Potential Tetracycline Exposure on the Phenotype of Aedes aegypti OX513A: Implications for Field Use". PLOS Neglected Tropical Diseases. 9 (8): e0003999. doi:10.1371/journal.pntd.0003999. PMC 4535858. PMID 26270533.
- ↑ Kevin Gorman; Josué Young; Lleysa Pineda; Ricardo Márquez; Nestor Sosa; Damaris Bernal; Rolando Torres; Yamilitzel Soto; Renaud Lacroix; Neil Naish; Paul Kaiser; Karla Tepedino; Gwilym Philips; Cecilia Kosmann; Lorenzo Cáceres (September 2015). "Short-term suppression of Aedes aegypti using genetic control does not facilitate Aedes albopictus". Pest Management Science. 72 (3): 618–628. doi:10.1002/ps.4151. PMC 5057309. PMID 26374668.
- ↑ Oreenaiza Nordin; Wesley Donald; Wong Hong Ming; Teoh Guat Ney; Khairul Asuad Mohamed; Nor Azlina Abdul Halim; Peter Winskill; Azahari Abdul Hadi; Zulkamal Safi'in Muhammad; Renaud Lacroix; Sarah Scaife; Andrew Robert McKemey; Camilla Beech; Murad Shahnaz; Luke Alphey; Derric David Nimmo; Wasi Ahmed Nazni; Han Lim Lee (March 2013). "Oral Ingestion of Transgenic RIDL Ae. aegypti Larvae Has No Negative Effect on Two Predator Toxorhynchites Species". PLOS One. 8 (3): e58805. Bibcode:2013PLoSO...858805N. doi:10.1371/journal.pone.0058805. PMC 3604150. PMID 23527029.
- ↑ Was Zika outbreak caused by release of genetically modified mosquitoes in Brazil?
- ↑ Can GM mosquitoes rid the world of a major killer?
- ↑ Justine Alford via IFLScience (25 July 2014). "Brazil To Unleash Genetically Modified Mosquitoes". Huffington Post. Retrieved 2014-07-25.
- ↑ no by-line (30 April 2015). "Modified mosquitoes enter the war against dengue in São Paulo". G1. Retrieved 2015-04-30.
- ↑ "Release potential of GM insects to fight disease and pests". Parliament UK. House of Lords Science and Technology Select Committee. 17 December 2015. Retrieved 2015-12-17.
- ↑ "Preliminary Finding of No Significant Impact (FONSI) In Support of an Investigational Field Trial of OX513A Aedes aegypti Mosquitoes" (PDF). US FDA. March 2016. Retrieved 14 March 2016.
- ↑ Clive Cookson (23 April 2015). "'Lethal' gene to combat malaria relies on laws of attraction". Financial Times. Retrieved 2015-04-23.
- ↑ Tirone, Jonathan (12 February 2016). "UN Readies Nuclear Solution to Destroy the Zika Virus". Bloomberg. Retrieved 2016-02-13.
- ↑ "Let's Stop Bad Bugs With Good Bugs". De Bug Project. Verily Life Sciences LLC. Retrieved 16 July 2017.
- ↑ Reegan AD; Ceasar SA; Paulraj MG; Ignacimuthu S; Al-Dhabi NA (January 2017). "Current status of genome editing in vector mosquitoes: A review". BioScience Trends. 10 (6): 424–432. doi:10.5582/bst.2016.01180. PMID 27990003.
- ↑ Heather Kowalski (May 17, 2007). "Scientists at J. Craig Venter Institute publish draft genome sequence from Aedes aegypti, mosquito responsible for yellow fever, dengue fever". J. Craig Venter Institute. Archived from the original on 2007-07-15. Retrieved 2007-05-18.
- ↑ Vishvanath Nene; Jennifer R. Wortman; Daniel Lawson; Brian Haas; Chinnappa Kodira; et al. (June 2007). "Genome sequence of Aedes aegypti, a major arbovirus vector". Science. 316 (5832): 1718–1723. Bibcode:2007Sci...316.1718N. doi:10.1126/science.1138878. PMC 2868357. PMID 17510324.
- ↑ Cosby, Rachel L.; Chang, Ni-Chen; Feschotte, Cédric (2019-09-01). "Host–transposon interactions: conflict, cooperation, and cooption". Genes & Development. Cold Spring Harbor Laboratory Press & The Genetics Society. 33 (17–18): 1098–1116. doi:10.1101/gad.327312.119. ISSN 0890-9369.
- ↑ Carpenter, Simon; Mellor, Philip S.; Fall, Assane G.; Garros, Claire; Venter, Gert J. (2017-01-31). "African Horse Sickness Virus: History, Transmission, and Current Status". Annual Review of Entomology. Annual Reviews. 62 (1): 343–358. doi:10.1146/annurev-ento-031616-035010. ISSN 0066-4170.
- 1 2 Takken, Willem; Verhulst, Niels O. (2013-01-07). "Host Preferences of Blood-Feeding Mosquitoes". Annual Review of Entomology. Annual Reviews. 58 (1): 433–453. doi:10.1146/annurev-ento-120811-153618. ISSN 0066-4170.
- ↑ Hasselquist, Fredrik, Carl von Linné (1757): Iter Palæstinum, Eller, Resa til Heliga Landet, Förrättad Infrån år 1749 til 1752
- ↑ Reise nach Palästina
- 1 2 P. F. Mattingly; Alan Stone; Kenneth L. Knight (1962). "Culex aegypti Linnaeus, 1762 (Insecta, Diptera); proposed validation and interpretation under the plenary powers of the species so named. Z.N.(S.) 1216" (PDF). Bulletin of Zoological Nomenclature. 19 (4): 208–219. Archived from the original (PDF) on 2012-03-01.
- ↑ International Commission on Zoological Nomenclature (1964). "Culex aegypti Linnaeus, 1762 (Insecta, Diptera): validated and interpreted under the plenary powers". Bulletin of Zoological Nomenclature. 21 (4): 246–248.
- ↑ John F. Reinert; Ralph E. Harbach; Ian J. Kitching (2004). "Phylogeny and classification of Aedini (Diptera: Culicidae), based on morphological characters of all life stages". Zoological Journal of the Linnean Society. 142 (3): 289–368. doi:10.1111/j.1096-3642.2004.00144.x.
- ↑ Andrew Polaszek (January 2006). "Two words colliding: resistance to changes in the scientific names of animals – Aedes vs Stegomyia". Trends in Parasitology. 22 (1): 8–9. doi:10.1016/j.pt.2005.11.003. PMID 16300998.
- ↑ "Journal of Medical Entomology Policy on Names of Aedine Mosquito Genera and Subgenera". Entomological Society of America. Retrieved August 31, 2011.
- ↑ "Etymologia: Aedes aegypti". Emerg Infect Dis. 22 (10): 1807. October 2016. doi:10.3201/eid2210.ET2210. PMC 5038420.
External links
| Wikimedia Commons has media related to Aedes aegypti. |
- VectorBase's genomic resource for Aedes aegypti Archived 2019-08-01 at the Wayback Machine
- Aedes aegypti page from University of Sydney, Australia
- Aedes aegypti and dengue fever
- United States CDC page on dengue fever containing information on prevalence of Aedes aegypti worldwide and past efforts to eradicate it
- Aedes aegypti on the UF / IFAS Featured Creatures Web site
- Walter Reed Hospital Distribution, taxonomy, references etc. Excellent image.
- Aedes aegypti at GeoChemBio/MetaPathogen/mosqito/aedes: taxonomy, life cycle, facts
- THE ECOLOGY AND BIOLOGY OF Aedes aegypti (L.) AND Aedes albopictus (Skuse) (DIPTERA: CULICIDAE) AND THE RESISTANCE STATUS OF Aedes albopictus (FIELD STRAIN) AGAINST ORGANOPHOSPHATES IN PENANG, MALAYSIA
- The Monte Verde Story (Honduras): Community Eradication of Aedes aegypti