Bee sting
| Bee sting | |
|---|---|
| Other names: Bee bite | |
 | |
| The stinger of a honey bee separated from the body and attached to a protective dressing | |
| Specialty | Emergency medicine |
| Symptoms | Sharp pain followed by redness and swelling[1] |
| Complications | Anaphylaxis[1] |
| Diagnostic method | Based on history of events[2] |
| Differential diagnosis | Cellulitis, folliculitis[1][2] |
| Prevention | DEET[1] |
| Treatment | Remove stinger, pain medication, apply cold, antihistamines, epinephrine[1] |
| Prognosis | Generally resolve in hours to days[1] |
| Frequency | Relatively common[2] |
| Deaths | <100/yr (USA)[3] |
A bee sting is an injury caused by the stinger of a female bee.[4] Symptoms include a sharp pain followed by redness, swelling, and itchiness.[1][2] Over the next day a blister may form and the area of redness may expand over 3 days.[2][5] This is generally followed by improvement over hours to days.[1] In more than 90% only a local reaction occurs; while in up to 9% of cases diffuse symptoms occur.[1] Complications may include anaphylaxis.[1] Secondary bacterial infection is uncommon.[5]
Honey bees generally only sting when threatened while the Africanized bee may sing without provocation.[1] Generally a bee is only able to sting once.[2] It is a type of hymenoptera sting, along with wasps, hornets, and fire ants.[2] Diagnosis is based on the history of events.[2]
Prevention includes the use of DEET.[1] Treatment generally involves removing the stinger, simple pain medication, application of cold, and antihistamines.[1] The stinger is best removed by scraping it off with an object such as a credit card.[2] Those with severe reactions may be treated with epinephrine or corticosteroids.[1] In those with a history of severe reactions, venom immunotherapy may be used.[1]
Bee stings are relatively common.[2] Children are more commonly affected than adults.[2] Less than 100 deaths occur a year in the United States due to bee, wasp, and hornet stings; of which 80% occur in males.[3] Bee stings were used by Hippocrates around 400 BCE for claimed health benefits.[6]
Signs and symptoms
Symptoms include a sharp pain followed by redness and swelling.[1] Generally this improves over hours to days.[1] In more than 90% only a local reaction occurs; while in up to 9% of cases diffuse symptoms occur.[1] In some people anaphylaxis can occur.[1]
 Bee sting. The stinger is torn off and left in the skin.
Bee sting. The stinger is torn off and left in the skin. 2 minutes later
2 minutes later 6 minutes later, after the stinger has been removed
6 minutes later, after the stinger has been removed 27 minutes later
27 minutes later A bee sting 1 day after
A bee sting 1 day after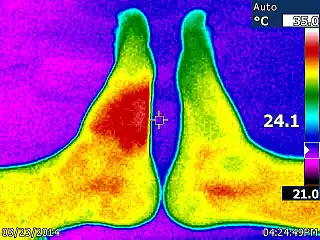 The left side of the image shows the ≈4 °C (7 °F) temperature increase (saturated red zone) caused by a bee sting after about 28 hours.
The left side of the image shows the ≈4 °C (7 °F) temperature increase (saturated red zone) caused by a bee sting after about 28 hours.
Cause

A honey bee that is away from the hive foraging for nectar or pollen will rarely sting, except when stepped on or roughly handled. Honey bees will actively seek out and sting when they perceive the hive to be threatened, often being alerted to this by the release of attack pheromones (below).
Although it is believed that a worker honey bee can sting only once, this is a partial misconception: although the stinger is in fact barbed so that it lodges in the person's skin, tearing loose from the bee's abdomen and leading to its death, this only happens if the skin is sufficiently thick, such as a mammal's.[7] Honey bees are the only hymenoptera with a strongly barbed sting, though yellow jackets and some other wasps have small barbs.
Bees with barbed stingers can often sting other insects without harming themselves. Queen honeybees and bees of many other species, including bumblebees and many solitary bees, have smoother stingers with smaller barbs, and can sting mammals repeatedly.[7]
The sting's injection of apitoxin into the person is accompanied by the release of alarm pheromones, a process which is accelerated if the bee is fatally injured. The release of alarm pheromones near a hive may attract other bees to the location, where they will likewise exhibit defensive behaviors until there is no longer a threat, typically because the person has either fled or been killed. A bee swarm, seen as a mass of bees flying or clumped together, is generally not hostile; it has deserted its hive and has no comb or young to defend. These pheromones do not dissipate or wash off quickly, and if their target enters water, bees will resume their attack as soon as it leaves the water. The alarm pheromone emitted when a bee stings another animal smells like a banana.[8][9]
Drone bees, the males, are larger and do not have stingers. The female bees (worker bees and queens) are the only ones that can sting, and their stinger is a modified ovipositor. The queen bee has a barbed but smoother stinger and can, if need be, sting skin-bearing creatures multiple times, but the queen does not leave the hive under normal conditions. Her sting is not for defense of the hive; she only uses it for dispatching rival queens, ideally before they can emerge from their cells. Queen breeders who handle multiple queens and have the queen odor on their hands are sometimes stung by a queen.
The stinger consists of three parts: a stylus and two barbed slides (or lancets), one on either side of the stylus. The bee does not push the stinger in but it is drawn in by the barbed slides. The slides move alternately up and down the stylus so when the barb of one slide has caught and retracts, it pulls the stylus and the other barbed slide into the wound. When the other barb has caught, it also retracts up the stylus pulling the sting further in. This process is repeated until the sting is fully in and even continues after the sting and its mechanism is detached from the bee's abdomen. When a female honey bee stings a person, it cannot pull the barbed stinger back out, but rather leaves behind not only the stinger, but also part of its abdomen and digestive tract, plus muscles and nerves. This massive abdominal rupture kills the honey bee. Honey bees are the only bees to die after stinging.[10]
Pathophysiology
The main component of bee venom responsible for pain in vertebrates is the toxin melittin; histamine and other biogenic amines may also contribute to pain and itching.[11]
The venom of the honeybee contains histamine, mast cell degranulating peptide, melittin, phospholipase A2, hyaluronidase and acid phosphatase. The three proteins in honeybee venom which are important allergens are phospholipase A2, hyaluronidase and acid phosphatase. In addition, the polypeptide melittin is also antigenic. Bumblebee venom appears to be chemically and antigenically related to honeybee venom.[12]
Treatment
The first step in treatment following a honey bee sting is removal of the stinger itself. The stinger should be removed as quickly as possible without regard to method: a study has shown the amount of venom delivered does not differ whether the sting is pinched or scraped off and even a delay of a few seconds leads to more venom being injected.[13] Once the stinger is removed, pain and swelling should be reduced with a cold compress.[14] A topical anesthetic containing benzocaine will relieve pain quickly and menthol is an effective anti-itch treatment.[15] Itching can also be relieved by antihistamine or by a topical steroid cream.[16]
Many traditional remedies have been suggested for bee stings.[17] No interventions have been proven to be effective in scientific studies and a randomized trial of aspirin paste and topical ice packs showed that aspirin was not effective in reducing the duration of swelling or pain in bee and wasp stings, and significantly increased the duration of redness.[14] The study concluded that ice alone is a better treatment for bee and wasp stings than aspirin.[14]
For about 2 percent of people, a hypersensitivity can develop after being stung, creating a more severe reaction. This sensitisation may happen after a single sting, or after a series of stings. An allergic person may suffer anaphylactic shock from certain proteins in the venom, which can be life-threatening and requires emergency treatment.[18] People known to be highly allergic may carry around epinephrine (adrenaline) in the form of a self-injectable EpiPen for the treatment of an anaphylactic shock. For people who experience severe or life-threatening reactions to insect stings, allergy injections composed of increasing concentrations of naturally occurring venom may provide protection against future insect stings.[19]
Society and culture
Apitherapy
As alternative medicine, apitherapy, bee venom has been used in arthritis and other painful conditions.[20] Evidence supporting this practice is either anecdotal, animal studies, or preliminary, most of which has poor methodology.[21] Apitherapy is not currently accepted as a medical treatment for any condition or disease; the risk of allergic reaction and anaphylaxis outweighs any benefits. According to the American Cancer Society, there is no scientific evidence that apitherapy or bee venom therapy can treat or change the course of cancer or any other disease.[22] Clinical trials have shown that apitherapy is ineffective in treating multiple sclerosis or any other disease, and can exacerbate multiple sclerosis symptoms.[23]
See also
- Characteristics of common wasps and bees
- Hornet stings
- Schmidt sting pain index
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 "Bee and wasp stings | DermNet NZ". dermnetnz.org. Archived from the original on 12 August 2021. Retrieved 21 June 2022.
- 1 2 3 4 5 6 7 8 9 10 11 Arif, F; Williams, M (January 2022). "Hymenoptera Stings". PMID 30085514.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 "QuickStats: Number of Deaths from Hornet, Wasp, and Bee Stings, Among Males and Females — National Vital Statistics System, United States, 2000–2017". MMWR. Morbidity and Mortality Weekly Report. 2019. doi:10.15585/mmwr.mm6829a5. Archived from the original on 15 June 2022. Retrieved 21 June 2022.
- ↑ Wilson-Rich, Noah; Allin, Kelly; Carreck, Norman; Quigley, Andrea (24 July 2018). The Bee: A Natural History. Princeton University Press. p. 10. ISBN 978-0-691-18247-6. Archived from the original on 27 June 2022. Retrieved 21 June 2022.
- 1 2 "Bee, Wasp, Hornet, and Ant Stings - Injuries and Poisoning". Merck Manuals Consumer Version. Archived from the original on 4 December 2021. Retrieved 21 June 2022.
- ↑ Grassberger, Martin; Sherman, Ronald A.; Gileva, Olga S.; Kim, Christopher; Mumcuoglu, Kosta (4 June 2013). Biotherapy - History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease using Living Organisms. Springer Science & Business Media. p. 79. ISBN 978-94-007-6585-6. Archived from the original on 27 June 2022. Retrieved 21 June 2022.
- 1 2 How Bees Work Archived 2013-06-28 at the Wayback Machine – howstuffworks.com. Retrieved 22 January 2013.
- ↑ "Analysis of Honeybee Aggression". Archived from the original on 2019-09-14. Retrieved 2022-03-21.
- ↑ Bortolotti, Laura; Costa, Cecilia (2014). "Chemical Communication in the Honey Bee Society". In Mucignat-Caretta, C (ed.). Neurobiology of Chemical Communication. Taylor & Francis. ISBN 978-1-4665-5341-5. PMID 24830041. Archived from the original on 2021-05-03. Retrieved 2022-03-21.
- ↑ Urban Bee Gardens Archived 2010-05-01 at the Wayback Machine Urban Bee Legends – by Jaime Pawelek
- ↑ Meier J, White J (1995). Clinical toxicology of animal venoms and poisons. CRC Press. ISBN 0-8493-4489-1.
- ↑ Rook's textbook of dermatology (Ninth ed.). p. 34.15. ISBN 9781118441190.
- ↑ Visscher P, Vetter R, Camazine S (1996). "Removing bee stings". Lancet. 348 (9023): 301–2. doi:10.1016/S0140-6736(96)01367-0. PMID 8709689. S2CID 43667134.
- 1 2 3 Balit C, Isbister G, Buckley N (2003). "Randomized controlled trial of topical aspirin in the treatment of bee and wasp stings". J. Toxicol. Clin. Toxicol. 41 (6): 801–8. doi:10.1081/CLT-120025345. PMID 14677790. S2CID 35809173.
- ↑ "Bites, Stings and Venomous Things". National Agricultural Safety Database. May 2009. Archived from the original on 22 July 2015. Retrieved 1 September 2015.
- ↑ "Insect Bites and Stings". patient.info. Archived from the original on 22 January 2019. Retrieved 15 February 2015.
- ↑ Beverly Sparks, "Stinging and Biting Pests of People" Archived 2007-02-14 at the Wayback Machine Extension Entomologist of the University of Georgia College of Agricultural & Environmental Sciences Cooperative Extension Service.
- ↑ Thor Lehnert, "Hymenopterous Insect Stings" Archived 2018-02-01 at the Wayback Machine Beekeeping in the United States – USDA – Agricultural HandBook Number 335
- ↑ Resiman, R (August 1994). "Insect Stings". New England Journal of Medicine. 331 (8): 523–7. doi:10.1056/NEJM199408253310808. PMID 8041420.
- ↑ Phillip Terc. "Report about a Peculiar Connection Between the Bee stings and Rheumatism", 1888.
- ↑ Frick, Lisa (2005). "Apitherapy". Encyclopedia.com. HighBeam Research. Archived from the original on 2 October 2016. Retrieved 28 September 2016.
- ↑ American Cancer Society's Guide to complementary and alternative cancer methods. Atlanta, Georgia: American Cancer Society. 2000. ISBN 978-0-944235-29-4.
- ↑ "Bee Venom Therapy – Grassroots Medicine". Science-Based Medicine. 26 November 2008. Archived from the original on 25 March 2015. Retrieved 28 September 2016.
External links
| Classification |
|---|