Tick paralysis
| Tick paralysis | |
|---|---|
 | |
| Australian paralysis tick before and after feeding | |
| Specialty | Emergency medicine |
| Symptoms | Tiredness, poor ability to walk, muscle weakness[1] |
| Complications | Respiratory failure[1] |
| Usual onset | 2 to 7 days with an attached tick[2][1] |
| Duration | Until a few hours to days after removal[1] |
| Causes | Certain types of tick bites[1] |
| Diagnostic method | Thorough examination[1] |
| Differential diagnosis | Guillain-Barre syndrome, botulism, poliomyelitis, myasthenia gravis, hypokalemia[1][3] |
| Treatment | Supportive care, removing the tick[1] |
| Prognosis | Good with treatment[1] |
| Frequency | Rare[3] |
Tick paralysis is a neurological condition that begins with tiredness, and progresses to poor ability to walk and muscle weakness as a result of certain tick bites.[1] Weakness starts in the legs and moves up the body.[1] Fever and rash do not generally occur.[1] Onset generally requires the tick to be attached for two to seven days.[1][2] Complications can include respiratory failure.[1]
While more than 40 types of type ticks are implicated, in North America the American dog tick and Rocky Mountain wood tick are most commonly involved while in Australia it is the Australian paralysis tick.[1] The underlying mechanism involves neurotoxin produced in female tick's salivary gland.[1] Diagnosis is by a thorough examination to find the tick.[1] It is a type of tick-borne illness.[1]
Treatment involves supportive care and removing the tick.[1] Supportive care may include mechanical ventilation.[1] Prevention is by avoiding tick bites such as by applying permethrin to clothing and using DEET.[1] Full recovery occurs within a few hours to days of the ticks removal.[1]
Tick paralysis is rare.[3] Cases, when they do occur, are most frequent in North America and Australia.[1] Children are more commonly affected than adults.[1] The condition was first described in the 1800s.[1] Other animals may also be affected.[1]
Signs and symptoms
Onset of symptoms requires the tick to be attached for 2–7 days. Symptoms begin with weakness in both legs that progresses to paralysis. The paralysis ascends to the trunk, arms, and head within hours and may lead to respiratory failure and death. The disease can present as acute ataxia without muscle weakness.
Patients may report minor sensory symptoms, such as local numbness, but constitutional signs are usually absent. Deep tendon reflexes are usually decreased or absent, and ophthalmoplegia and bulbar palsy can occur.
Electromyographic (EMG) studies usually show a variable reduction in the amplitude of compound muscle action potentials, but no abnormalities of repetitive nerve stimulation studies. These appear to result from a failure of acetylcholine release at the motor nerve terminal level. There may be subtle abnormalities of motor nerve conduction velocity and sensory action potentials.
Cause
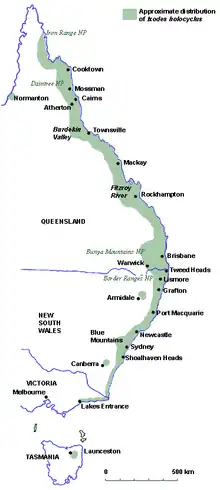
The two ticks most commonly associated with North American tick paralysis are the Rocky Mountain wood tick (Dermacentor andersoni) and the American dog tick (Dermacentor variabilis); however, 43 tick species have been implicated in human disease around the world.[4] Most North American cases of tick paralysis occur from April to June, when adult Dermacentor ticks emerge from hibernation and actively seek hosts.[5] In Australia, tick paralysis is caused by the tick Ixodes holocyclus. Prior to 1989, 20 fatal cases were reported in Australia.[6]
Pathogenesis
Tick paralysis is believed to be due to toxins found in the tick's saliva that enter the bloodstream while the tick is feeding.
Tick paralysis occurs when an engorged and gravid (egg-laden) female tick produces a neurotoxin in its salivary glands and transmits it to its host during feeding. Experiments have indicated that the greatest amount of toxin is produced between the fifth and seventh day of attachment (often initiating or increasing the severity of symptoms), although the timing may vary depending on the species of tick.
Unlike Lyme disease, ehrlichiosis, and babesiosis, which are caused by parasites in their hosts long after the offending tick is gone, tick paralysis is chemically induced by the tick and therefore usually only continues in its presence. Once the tick is removed, symptoms usually diminish rapidly. However, in some cases, profound paralysis can develop and even become fatal before anyone becomes aware of a tick's presence.
Diagnosis
Diagnosis is based on symptoms and upon finding an embedded tick, usually on the scalp.
In the absence of a tick, the differential diagnosis includes Guillain–Barré syndrome. Early signs of tick poisoning could be a change of an animals' ‘voice’, weakness in the back legs or vomiting.
Prevention
No human vaccine is currently available for any tick-borne disease, except for tick-borne encephalitis. Individuals should therefore take precautions when entering tick-infested areas, particularly in the spring and summer months. Preventive measures include avoiding trails that are overgrown with bushy vegetation, wearing light-coloured clothes that allow one to see the ticks more easily, and wearing long pants and closed-toe shoes. Tick repellents containing DEET (N,N, diethyl-m-toluamide) are only marginally effective and can be applied to skin or clothing. Rarely, severe reactions can occur in some people who use DEET-containing products. Young children may be especially vulnerable to these adverse effects. Permethrin, which can only be applied to clothing, is much more effective in preventing tick bites. Permethrin is not a repellent but rather an insecticide; it causes ticks to curl up and fall off the protected clothing.
Treatment
Removal of the offending tick usually results in resolution of symptoms within several hours to days. The tick is best removed by grasping it as close to the skin as possible and pulling in a firm steady manner.[7] Because the toxin lies in the tick's salivary glands, care must be taken to remove the entire tick (including the head), or symptoms may persist.
 a) Paralysis tick attached to right temporal bulbar conjunctiva b)surgical removal of the larval tick
a) Paralysis tick attached to right temporal bulbar conjunctiva b)surgical removal of the larval tick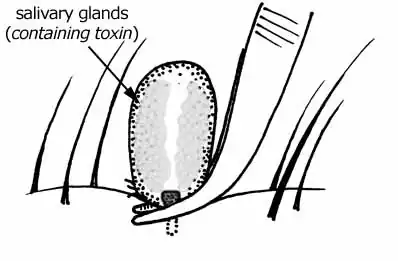 Tick removal. Compressing the body of the tick could cause more toxins to be injected into the host.
Tick removal. Compressing the body of the tick could cause more toxins to be injected into the host.
Prognosis
If the tick is not removed, the toxin can be fatal. A 1969 study of children reported mortality rates of 10 – 12 percent,[8] mostly due to respiratory paralysis.
Unlike the toxin of other tick species, the toxin of Ixodes holocyclus (Australian paralysis tick) may still be fatal even if the tick is removed.
Epidemiology
Although tick paralysis is of concern in domestic animals and livestock in the United States, human cases are rare and usually occur in children under the age of 10.
Society and culture
In the TV show, Hart of Dixie, Season 1, Episode 2, a patient is diagnosed with tick paralysis who has been deer hunting.
In the TV show, Emergency!, Season 5, Episode 4, "Equipment" (first aired Oct. 4, 1975), Dr. Joe Early diagnoses a young boy who has fallen from a tree with tick paralysis, after eliminating polio as a cause.[9]
In the TV show, House, Season 2, Episode 16, "Safe", Dr House diagnoses a patient (played by Michelle Trachtenberg) with tick paralysis.[10]
In the TV show, Remedy, Season 1 Episode 7, "Tomorrow, the Green Grass", Rebecca is diagnosed with tick paralysis.
In the TV show, Royal Pains, Season 1 Episode 3, "Strategic Planning", a US Senator's teenage son is diagnosed with and overcomes tick paralysis.
In the TV show, Chicago Med, Season 3, Episode 5, "Mountains and Molehills", a young girl returning from Australia with increasing paralysis is diagnosed with tick paralysis.
Other animals
For affected animals, food and water intake can worsen the outcome, as the toxin can prevent the animal from swallowing properly. People who find a tick on their animal, are advised to remove it immediately and seek veterinary assistance if the animal shows any signs of illness. The tick can be placed in a tightly sealed plastic bag and taken to a veterinarian for identification.[11][12]
Research
Although several attempts have been made to isolate and identify the neurotoxin since the first isolation in 1966, the exact structure of the toxin has still not been published.[13] The 40-80 kDa protein fraction contains the toxin.[14]
The neurotoxin structure and gene, at least for the tick species Ixodes holocyclus have since been identified and are called holocyclotoxins after the species. At least three members (HT-1,[15] HT-3,[16] and HT-12[17]) trigger paralysis by presynaptic inhibition of neurotransmitter release via a calcium dependent mechanism resulting in a reduction of quantal content, and loss of effective neuromuscular synaptic transmission.[18]
See also
- Polyneuropathy in dogs and cats for tick paralysis in dogs
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Simon, LV; West, B; McKinney, WP (January 2022). "Tick Paralysis". PMID 29262244.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Pecina, CA (November 2012). "Tick paralysis". Seminars in neurology. 32 (5): 531–2. doi:10.1055/s-0033-1334474. PMID 23677663.
- 1 2 3 "Tick Paralysis - Injuries; Poisoning". Merck Manuals Professional Edition. Archived from the original on 30 October 2021. Retrieved 13 July 2022.
- ↑ Gothe R, Kunze K, Hoogstraal H (1979). "The mechanisms of pathogenicity in the tick paralyses". J Med Entomol. 16 (5): 357–69. doi:10.1093/jmedent/16.5.357. PMID 232161.
- ↑ Dworkin MS, Shoemaker PC, Anderson D (1999). "Tick paralysis: 33 human cases in Washington state, 1946–1996". Clin Infect Dis. 29 (6): 1435–9. doi:10.1086/313502. PMID 10585792.
- ↑ Masina S; Broady K. W. (1999). "Tick paralysis: development of a vaccine". International Journal for Parasitology. 29 (4): 535–541. doi:10.1016/S0020-7519(99)00006-5. PMID 10428629.
- ↑ Needham GR (1985). "Evaluation of five popular methods for tick removal". Pediatrics. 75 (6): 997–1002. doi:10.1542/peds.75.6.997. PMID 4000801. S2CID 23208238.
- ↑ Schmitt N, Bowmer EJ, Gregson JD (1969). "Tick paralysis in British Columbia". Can Med Assoc J. 100 (9): 417–21. PMC 1945728. PMID 5767835.
- ↑ "IMDB". IMDb. Archived from the original on 2021-11-26. Retrieved 2022-02-05.
- ↑ "House MD Episode Guide: Season Two #216 'Safe'". housemd-guide.com. Archived from the original on May 9, 2012. Retrieved August 11, 2012.
- ↑ Cannon, Michael. "Envenomation: Tick Paralysis" (PDF). Archived (PDF) from the original on May 16, 2018. Retrieved June 11, 2018.
- ↑ O’Keefe, Dr Janette. "Australian Paralysis Tick" (PDF). Archived (PDF) from the original on March 23, 2018. Retrieved June 9, 2018.
- ↑ Doube B. M. (1975). "Cattle and Paralysis Tick Ixodes-Holocyclus". Australian Veterinary Journal. 51 (11): 511–515. doi:10.1111/j.1751-0813.1975.tb06901.x. PMID 1220655.
- ↑ B. F. Stone; K. C. Binnington; M. Gauci; J. H. Aylward (1989). "Tick/host interactions forIxodes holocyclus: Role, effects, biosynthesis and nature of its toxic and allergenic oral secretions". Experimental and Applied Acarology. 7 (1): 59–69. doi:10.1007/BF01200453. PMID 2667920. S2CID 23861588.
- ↑ "Ixodes holocyclus holocyclotoxin-1 (HT1) mRNA, complete cds - Nucleotide - NCBI". www.ncbi.nlm.nih.gov. 27 October 2004. Archived from the original on 2018-07-29. Retrieved 2018-07-29.
- ↑ "Ixodes holocyclus holocyclotoxin 3 (HT3) mRNA, complete cds - Nucleotide - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 2018-07-29. Retrieved 2018-07-29.
- ↑ "Ixodes holocyclus holocyclotoxin 12 (HT12) mRNA, complete cds - Nucleotide - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 2018-07-29. Retrieved 2018-07-29.
- ↑ Chand, Kirat K.; Lee, Kah Meng; Lavidis, Nickolas A.; Rodriguez-Valle, Manuel; Ijaz, Hina; Koehbach, Johannes; Clark, Richard J.; Lew-Tabor, Ala; Noakes, Peter G. (2016-07-08). "Tick holocyclotoxins trigger host paralysis by presynaptic inhibition". Scientific Reports. 6 (1): 29446. Bibcode:2016NatSR...629446C. doi:10.1038/srep29446. ISSN 2045-2322. PMC 4937380. PMID 27389875.
External links
| Classification | |
|---|---|
| External resources |