Kyasanur Forest disease
| Kyasanur forest disease | |
|---|---|
| Other names: Monkey disease, monkey fever | |
 | |
| Virus ecology | |
| Specialty | Infectious disease |
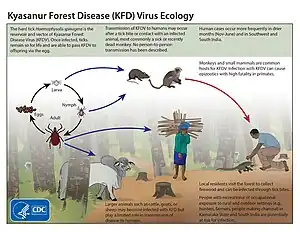
Kyasanur forest disease (KFD) is a tick-borne viral haemorrhagic fever endemic to South-western part of India.[1] The disease is caused by a virus belonging to the family Flaviviridae. KFDV is transmitted to humans through the bite of infected hard ticks (Haemaphysalis spinigera) which act as a reservoir of KFDV.
Signs and symptoms
The symptoms of the disease include a high fever with frontal headaches, chills, severe muscle pain, vomiting, and other gastrointestinal symptoms. Bleeding problems may occur 3–4 days after initial symptom onset. Patients may experience abnormally low blood pressure, and low platelet, red blood cell, and white blood cell count. After 1–2 weeks of symptoms, some patients recover without complication. However, the illness is biphasic for a subset of patients (10-20%) who experience a second wave of symptoms at the beginning of the third week. These symptoms include fever and signs of neurological manifestations, such as severe headache, mental disturbances, tremors, and vision deficits.[2][3][4] The convalescent period is typically very long, lasting several months. Muscle aches and weakness also occur during this period, and the patient is unable to engage in physical activities.
Cause
Virology
| Kyasanur Forest disease virus | |
|---|---|
 | |
| Flavivirus structure and genome | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Kitrinoviricota |
| Class: | Flasuviricetes |
| Order: | Amarillovirales |
| Family: | Flaviviridae |
| Genus: | Flavivirus |
| Species: | Kyasanur Forest disease virus |
| Synonyms[5] | |
|
Kyasanur Forest virus | |
The KFD virus is a typical flavivirus measuring about 40-60 nm in diameter. The genome of KFDV consists of 10,774 nucleotides of single-stranded, positive-sense RNA encoding a single polyprotein that is cleaved post-translationally into three structural (C, prM/M and E) and seven non-structural (NS1, NS2a, NS2b, NS3, NS4a, NS4b and NS5) proteins.[6][7][8] The genome of KFDV is very similar (>92% homologous) to that of Alkhurma Hemorrhagic Fever Virus which is primarily found in Saudi Arabia. These two species both belong to the family Flaviviridae and diverged over 700 years ago and have thus remained geographically separated.[9]
Transmission
.jpg.webp)
A variety of animals are thought to be reservoir hosts for the disease, including porcupines, rats, squirrels, mice, and shrews.[2] Monkeys are the main amplifying hosts for KFD virus and they are also affected by the virus. The surili Presbytis entellus and the bonnet macaque are very susceptible to the KFD virus. They develop tremendous viremia and infect the ticks. The vector for disease transmission is Haemaphysalis spinigera, a forest tick.[10] Humans contract infection from the bite of nymphs of the tick. Man is a terminal host and there no human-to-human transmission because the human domestic environment does not sustain the ticks.
Risk factors
The spill-over of Kyasanur forest disease happens at the crossroads of the animal-human interaction, especially villages adjoining forest areas and inter-state borders.[11] People who frequently visit the forest areas of the Western Ghats region such as forest guards and officials, range forest officer (RFO), forest watchers, shepherds, firewood collectors, dry leaf collectors, hunters, people who handle dead animal carcasses, travelers who camp in the forest areas, tribal communities living inside the forest areas (Jenu kurubas and Betta kurubas), cashew nut workers especially those who engage in cleaning the dry leaves before the harvest season (seen in Pali and Mauxi outbreaks, North Goa), and areca nut farm workers working in infected tick areas will have a high risk of acquiring KFD infection. People who live in the KFD endemic areas and refuse to take KFD vaccination are at risk in contracting the infection.
Pathology
The pathogenesis of KFDV is not completely understood. Research using mice models found that KFDV primarily replicated in the brain.[12] Other research has expanded on this by described neurological changes that occurred within infected organisms. This experiment was completed by using KFDV-infected mice and discovered that KFDV caused gliosis, inflammation, and cell death in the brain. They posited that KFDV could be primarily a neuropathic disease and other symptoms are due to this pathogenesis.[13]
Diagnosis
In earlier days suspected case were confirmed in a laboratory by serum inoculation into suckling mice (Swiss Albino mice) and subsequent death of mice was leveled as KFD Positive case. Other methods of diagnosis included hemagglutination inhibition (HI), complement fixation, neutralization tests.[14] However, new research has introduced more efficient molecular based methods to diagnose KFDV. These methods include: RT-PCR, nested RT-PCR, TaqMan-based real-time RT-PCR, Immunoglobin M antibodies and Immunoglobin G detection by ELISA. The two methods involving RT-PCR are able to function by attaching a primer to the NS-5 gene, which is highly conserved among the genus to which KFDV belongs. PCR positivity is limited to 8–10 days from the onset of symptoms. The ELISA based methods allows for the detections of anti-KFDV antibodies in patients typically from 5th day of onset of symptoms up to 3 months.[15]
Prevention
Prevention is by vaccination, as well as preventive measures such as protective clothing and tick population control. The vaccine for KFDV consists of formalin-inactivated KFDV. The vaccine has a 62.4% effectiveness rate for individuals who receive two doses. For individuals who receive an additional dose, the effectiveness increases to 82.9%.[16]
Management
Specific antiviral treatments are not available as of 2022.[17]
Epidemiology
The disease has a fatality rate of 3-10%, and it affects 400-500 people annually.[10][15]
The disease was first noted at Kyasanur village near Sagar in Shivamogga district of Karnataka. The virus has been detected in monkeys in parts of Bandipur National Park (Chamarajnagar) and parts of the Nilgiris. Human infection occurred in Bandipur through handling of dead monkeys that were infected. A human carrier was also detected in Wayanad (Kerala).[18] The disease has shown its presence in the adjacent states of Karnataka including Kerala, Maharashtra, Goa, Tamil Nadu and Gujarat.[19][20][21]
Affected states in India
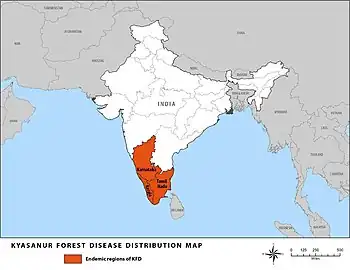
The disease initially reported from Shimoga district of Karnataka which is a primitive sylvan territory in Western Ghats of India. The disease spread out to other districts of Karnataka involving districts of Chikkamagalore, Uttara Kannada, Dakshina Kannada, Udupi, Chamarajanagar (2012), Belagavi (2016). In 2013, KFDV was detected in monkey autopsies from Nilgiris district of Tamil Nadu state. Monkey deaths and human cases have now been reported from three neighbouring states bordering Karnataka, i.e., Wayanad (2013) and Malappuram districts of Kerala (2014), North Goa district of Goa state (2015), and Sindhudurg district of Maharashtra (2016).[22]
Serological evidence for KFD
There are reported serological evidence for KFD detected in humans in other parts of India, namely Kutch and Saurashtra regions of Gujarat state, Kingaon and Parbatpur of West Bengal state.[23] A seroprevalence study in Andaman and Nicobar islands in 2002 revealed a high prevalence of hemagglutination inhibition (HI) antibodies against KFDV.[24]
History
The disease was first reported from Kattinakere village forest which is in the Kyasanur forest range of Karnataka in India in March 1957. When the officials visited the Kattinakere forest and discovered the diseases they noticed a sign board informing that this was the Kyasanur forest range. Hence the name. The disease first manifested as an epizootic outbreak among monkeys, killing several of them in the year 1957. Hence the disease is also locally known as "monkey disease" or "monkey fever".[25] The similarity with Russian spring-summer encephalitis was noted and the possibility of migratory birds carrying the disease was raised.[26] Studies began to look for the possible species that acted as reservoirs for the virus and the agents responsible for transmission. Subsequent studies failed to find any involvement of migratory birds, although the possibility of their role in initial establishment was not ruled out. The virus was found to be quite distinctive and not closely related to the Russian virus strains. Antigenic relatedness is, however, close to many other strains including the Omsk hemorrhagic fever (OHF) and birds from Siberia have been found to show an antigenic response to KFD virus. Sequence based studies note the distinctiveness of OHF.[27] Early studies in India were conducted in collaboration with the US Army Medical Research Unit and this led to controversy and conspiracy theories.[28][29]
Subsequent studies based on sequencing found that the Alkhurma virus found in Saudi Arabia is closely related.[30] In 1989 a patient in Nanjianin, China was found with fever symptoms and in 2009 its viral gene sequence was found to exactly match with that of the KFD reference virus of 1957. This has been questioned, though, since the Indian virus shows variations in sequence over time and the exact match with the virus sequence of 1957 and the Chinese virus of 1989 is not expected. This study also found using immune response tests that birds and humans in the region appeared to have been exposed to the virus.[31] Another study has suggested that the virus is recent in origin dating the nearest common ancestor of it and related viruses to around 1942, based on the estimated rate of sequence substitutions. The study also raises the possibility of bird involvement in long-distance transfer.[32] It appears that these viruses diverged 700 years ago.[33]
A recent outbreak in 2020, claimed two lives in Siddapura, Karnataka. The peak season for this disease in Malnad is from March till May but has been observed to peak earlier in the year as well. There were a total of 55 reported cases in Shivamogga district, Karntaka.[34][35]
References
- ↑ EA Gould; T Solomon (February 9, 2008). "Pathogenic flaviviruses". The Lancet. 371 (961): 500–509. doi:10.1016/S0140-6736(08)60238-X. ISSN 0140-6736. PMID 18262042. S2CID 205949828.
- 1 2 Gerhard Dobler (27 January 2010). "Zoonotic tick-borne flaviviruses". Veterinary Microbiology. 140 (3–4, Zoonoses: Advances and Perspectives): 221–228. doi:10.1016/j.vetmic.2009.08.024. ISSN 0378-1135. PMID 19765917.
- ↑ Dobler, Gerhard (2010). "Zoonotic tick-borne flaviviruses". Veterinary Microbiology. 140 (3/4): 221–228. doi:10.1016/j.vetmic.2009.08.024. PMID 19765917.
- ↑ Mourya, Devendra; Yadav, Pragya; Sandhya, V; Reddy, Shivanna (2013). "Spread of Kyasanur Forest Disease, Bandipur Tiger Reserve, India, 2012-2013". Emerging Infectious Diseases. 19 (9): 1540–1541. doi:10.3201/eid1909.121884. PMC 3810911. PMID 23977946.
- ↑ ICTV 2nd Report Fenner, F (1976). "Classification and nomenclature of viruses. Second report of the International Committee on Taxonomy of Viruses" (PDF). Intervirology. 7 (1–2): 1–115. doi:10.1159/000149938. PMID 826499. Archived (PDF) from the original on 2023-02-17. Retrieved 2023-03-22.
- ↑ Cook, Bradley W. M.; Cutts, Todd A.; Court, Deborah A.; Theriault, Steven (February 2012). "The generation of a reverse genetics system for Kyasanur Forest Disease Virus and the ability to antagonize the induction of the antiviral state in vitro". Virus Research. 163 (2): 431–438. doi:10.1016/j.virusres.2011.11.002. ISSN 1872-7492. PMID 22100401.
- ↑ Cook, Bradley; Ranadheera, Charlene; Nikiforuk, Aidan; Cutts, Todd; Kobasa, Darwyn; Court, Deborah; Theriault, Steven (2016). "Limited Effects of Type I Interferons on Kyasanur Forest Disease Virus in Cell Culture". PLOS Neglected Tropical Diseases. 10 (8): e0004871. doi:10.1371/journal.pntd.0004871. PMC 4968803. PMID 27479197.
- ↑ Dodd, Kimberly; Bird, Brian; Khristova, Marina; Albariño, César; Carroll, Serena; Comer, James; Erickson, Bobbie; Rollin, Pierre; Nichol, Stuart (2011). "Ancient Ancestry of KFDV and AHFV Revealed by Complete Genome Analyses of Viruses Isolated from Ticks and Mammalian Hosts". PLOS Neglected Tropical Diseases. 5 (10): e1352. doi:10.1371/journal.pntd.0001352. PMC 3186760. PMID 21991403.
- ↑ Dodd, Kimberly; Bird, Brian; Jones, Megan; Nichol, Stuart; Spiropoulou, Christina (2014). "Kyasanur Forest Disease Virus Infection in Mice Is Associated with Higher Morbidity and Mortality than Infection with the Closely Related Alkhurma Hemorrhagic Fever Virus". PLOS ONE. 9 (6): e100301. Bibcode:2014PLoSO...9j0301D. doi:10.1371/journal.pone.0100301. PMC 4065072. PMID 24950196.
- 1 2 Holbrook, Michael (2012). "Kyasanur forest disease". Antiviral Research. 96 (3): 353–362. doi:10.1016/j.antiviral.2012.10.005. PMC 3513490. PMID 23110991.
- ↑ Davison, Catherine (16 March 2023). "Why areca nut plantations are driving 'monkey fever'". BBC. Archived from the original on 2023-03-17. Retrieved 2023-03-17.
- ↑ Sawatsky, Bevan; McAuley, Alexander; Holbrook, Michael; Bente, Dennis (2014). "Comparative Pathogenesis of Alkhumra Hemorrhagic Fever and Kyasanur Forest Disease Viruses in a Mouse Model". PLOS Neglected Tropical Diseases. 8 (6): e2934. doi:10.1371/journal.pntd.0002934. PMC 4055546. PMID 24922308.
- ↑ Basu, Atanu; Yadav, Pragya; Prasad, Sharda; Badole, Sachin; Patil, Dilip; Kohlapure, Rajendra; Mourya, Devendra (2016). "An Early Passage Human Isolate of Kyasanur Forest Disease Virus Shows Acute Neuropathology in Experimentally Infected CD-1 Mice". Vector Borne & Zoonotic Diseases. 16 (7): 496–498. doi:10.1089/vbz.2015.1917. PMID 27171207.
- ↑ Upadhyaya, S.; Narasimha Murthy, D. P.; Yashodhara Murthy, B. K. (July 1975). "Viraemia studies on the Kyasanur Forest Disease human cases of 1966". The Indian Journal of Medical Research. 63 (7): 950–953. ISSN 0971-5916. PMID 175006.
- 1 2 Mourya, Devendra; Yadav, Pragya; Mehla, Rajeev; Barde, Pradip; Yergolkar, Prasanna; Kumar, Sandeep; Thakare, Jyotsna; Mishra, Akhilesh (2012). "Diagnosis of Kyasanur forest disease by nested RT-PCR, real-time RT-PCR and IgM capture ELISA". Journal of Virological Methods. 186 (1/2): 49–54. doi:10.1016/j.jviromet.2012.07.019. PMID 22874757.
- ↑ Kasabi, Gudadappa; Murhekar, Manoj; Sandhya, Vijay; Raghunandan, Ramappa; Kiran, Shivani; Channabasappa, Gowdra; Mehendale, Sanjay (2013). "Coverage and Effectiveness of Kyasanur Forest Disease (KFD) Vaccine in Karnataka, South India, 2005-10". PLOS Neglected Tropical Diseases. 7 (1): e2025. doi:10.1371/journal.pntd.0002025. PMC 3554520. PMID 23359421.
- ↑ Gupta N, Wilson W, Neumayr A, Saravu K. Kyasanur forest disease: a state-of-the-art review. QJM. 2022 Jun 7;115(6):351-358. doi:10.1093/qjmed/hcaa310 PMID 33196834
- ↑ Mourya DT, Yadav PD, Sandhya VK, Reddy S (2013). "Spread of Kyasanur Forest disease, Bandipur Tiger Reserve, India, 2012–2013 [letter]". Emerging Infectious Diseases. 19 (9): 1540–1541. doi:10.3201/eid1909.121884. PMC 3810911. PMID 23977946.
- ↑ Awate, P.; Yadav, P.; Patil, D.; Shete, A.; Kumar, V.; Kore, P.; Dolare, J.; Deshpande, M.; Bagde, S.; Sapkal, G.; Gurav, Y.; Mourya, D.T. (2016). "Outbreak of Kyasanur Forest disease (monkey fever) in Sindhudurg, Maharashtra State, India, 2016". Journal of Infection. 72 (6): 759–761. doi:10.1016/j.jinf.2016.03.006. PMID 26997635.
- ↑ Patil, D.Y.; Yadav, P.D.; Shete, A.M.; Nuchina, J.; Meti, R.; Bhattad, D.; Someshwar, S.; Mourya, D.T. (2017). "Occupational exposure of cashew nut workers to Kyasanur Forest disease in Goa, India". International Journal of Infectious Diseases. 61: 67–69. doi:10.1016/j.ijid.2017.06.004. PMID 28627428.
- ↑ Sadanandane, C.; Elango, A.; Marja, Noonu; Sasidharan, P.V; Raju, K.H.K; Jambulingam, P. (2017). "An outbreak of Kyasanur forest disease in the Wayanad and Malappuram districts of Kerala, India". Ticks and Tick-borne Diseases. 8 (1): 25–30. doi:10.1016/j.ttbdis.2016.09.010. PMID 27692988.
- ↑ Mourya, D. T.; Yadav, P. D. (2016-02-03). "Recent Scenario of Emergence of Kyasanur Forest Disease in India and Public Health Importance". Current Tropical Medicine Reports. 3 (1): 7–13. doi:10.1007/s40475-016-0067-1. ISSN 2196-3045. S2CID 87259702.
- ↑ Pattnaik, Priyabrata (May 2006). "Kyasanur forest disease: an epidemiological view in India". Reviews in Medical Virology. 16 (3): 151–165. doi:10.1002/rmv.495. ISSN 1052-9276. PMID 16710839. S2CID 32814428.
- ↑ Padbidri, V. S.; Wairagkar, N. S.; Joshi, G. D.; Umarani, U. B.; Risbud, A. R.; Gaikwad, D. L.; Bedekar, S. S.; Divekar, A. D.; Rodrigues, F. M. (December 2002). "A serological survey of arboviral diseases among the human population of the Andaman and Nicobar Islands, India". The Southeast Asian Journal of Tropical Medicine and Public Health. 33 (4): 794–800. ISSN 0125-1562. PMID 12757228.
- ↑ Nichter, Mark (1987). "Kyasanur Forest Disease: An Ethnography of a Disease of Development". Medical Anthropology Quarterly. New Series. 1 (4): 406–423. doi:10.1525/maq.1987.1.4.02a00040.
- ↑ Work, Telford H.; Roderiguez, FR; Bhatt, PN (1959). "Virological Epidemiology of the 1958 Epidemic of Kyasanur Forest Disease" (PDF). American Journal of Public Health. 49 (7): 869–874. doi:10.2105/AJPH.49.7.869. PMC 1372906. PMID 13661478. Archived from the original on 2023-07-01. Retrieved 2023-03-22.
- ↑ Lin D, Li L, Dick D, Shope RE, Feldmann H, Barrett AD, Holbrook MR (2003). "Analysis of the complete genome of the tick-borne flavivirus Omsk hemorrhagic fever virus". Virology. 313 (1): 81–90. doi:10.1016/S0042-6822(03)00246-0. PMID 12951023.
- ↑ Harry Hoogstraal; Makram N. Kaiser; Melvin A. Traylor; Ezzat Guindy; Sobhy Gaber (1963). "Ticks (Ixodidae) on birds migrating from Europe and Asia to Africa, 1959-61". Bull. World Health Organ. 28 (2): 235–262. PMC 2554471. PMID 13961632.
- ↑ Lewis, Michael (2002). "Scientists or Spies? Ecology in a Climate of Cold War Suspicion". Economic and Political Weekly. 37 (24): 2324–32. JSTOR 4412243.
- ↑ Charrel RN, Zaki AM, Attoui H, Fakeeh M, Billoir F, Yousef AI, de Chesse R, De Micco P, Gould EA, de Lamballerie X (2001). "Complete coding sequence of the Alkhurma virus, a tick-borne Flavivirus causing severe hemorrhagic fever in humans in Saudi Arabia". Biochem. Biophys. Res. Commun. 287 (2): 455–61. doi:10.1006/bbrc.2001.5610. PMID 11554750.
- ↑ Jinglin Wang; Hailin Zhang; Shihong Fu; Huanyu Wang; Daxin Ni; Roger Nasci; Qing Tang; Guodong Liang (2009). "Isolation of Kyasanur Forest Disease Virus from Febrile Patient, Yunnan, China". Emerg. Infect. Dis. 15 (2): 326–328. doi:10.3201/eid1502.080979. PMC 2657630. PMID 19193286.
- ↑ Rajeev Mehla; Sandeep R.P. Kumar; Pragya Yadav; Pradip V. Barde; Prasanna N. Yergolkar; Bobbie R. Erickson; Serena A. Carroll; Akhilesh C. Mishra; Stuart T. Nichol; Devendra T. Mourya (2009). "Recent Ancestry of Kyasanur Forest Disease Virus". Emerging Infectious Diseases. 15 (9): 1431–1437. doi:10.3201/eid1509.080759. PMC 2819879. PMID 19788811.
- ↑ Dodd KA, Bird BH, Khristova ML, Albariño CG, Carroll SA, Comer JA, Erickson BR, Rollin PE, Nichol ST (2011). "Ancient ancestry of KFDV and AHFV revealed by complete genome analyses of viruses isolated from ticks and mammalian hosts". PLOS Negl Trop Dis. 5 (10): e1352. doi:10.1371/journal.pntd.0001352. PMC 3186760. PMID 21991403.
- ↑ "Monkey Fever or Kyasanur Forest Disease". Educationphile. Archived from the original on 2020-03-02. Retrieved 2020-03-02.
- ↑ "Monkey fever claims second victim in Karnataka". Deccan Herald. 2020-03-01. Archived from the original on 2020-03-02. Retrieved 2020-03-02.
External links
| Classification | |
|---|---|
| External resources |
|