Eastern equine encephalitis
| Eastern equine encephalitis | |
|---|---|
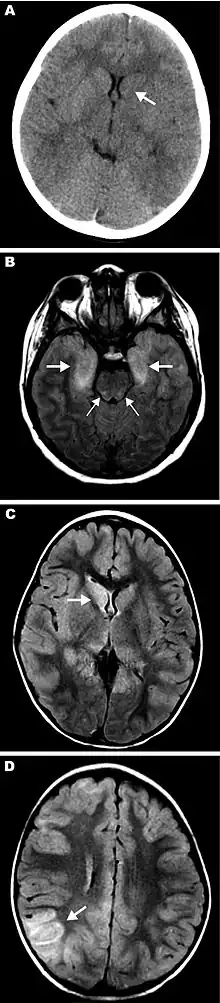
 | |
| a-c)Eastern equine encephalitis virus (EEEV) colocalized with neurons in study of eastern equine encephalitis (EEE) | |
| Symptoms | high fever, muscle pain, altered mental status, headache, meningeal irritation, photophobia, and seizures |
| Causes | Eastern equine encephalitis virus |
| Risk factors | People over the age of 50 or younger than the age of 16 are at greatest risk of developing severe disease. |
| Diagnostic method | Brain tissue examination |
| Prognosis | ≈33% risk of death[1] |
| Eastern equine encephalitis virus | |
|---|---|
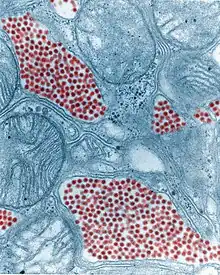 | |
| Colourised TEM micrograph of a mosquito salivary gland: The virus particles (virions) are coloured red. (83,900x magnification) | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Kitrinoviricota |
| Class: | Alsuviricetes |
| Order: | Martellivirales |
| Family: | Togaviridae |
| Genus: | Alphavirus |
| Species: | Eastern equine encephalitis virus |
Eastern equine encephalitis (EEE), commonly called Triple E or sleeping sickness (not to be confused with African trypanosomiasis), is a disease caused by a zoonotic mosquito vectored Togavirus that is present in North, Central, and South America, and the Caribbean. EEE was first recognized in Massachusetts, United States, in 1831, when 75 horses died mysteriously of viral encephalitis. Epizootics in horses have continued to occur regularly in the United States. It can also be identified in donkeys and zebras. Due to the rarity of the disease, its occurrence can cause economic impact beyond the cost of horses and poultry.[2]
EEE is found today in the eastern part of the United States and is often associated with coastal plains. It can most commonly be found in East Coast and Gulf Coast states.[1] In Florida, about one to two human cases are reported a year, although over 60 cases of equine encephalitis are reported. In years in which conditions are favorable for the disease, the number of equine cases is over 200.[3] Diagnosing equine encephalitis is challenging because many of the symptoms are shared with other illnesses and patients can be asymptomatic. Confirmations may require a sample of cerebral spinal fluid or brain tissue, although CT scans and MRI scans are used to detect encephalitis. This could be an indication that the need to test for EEE is necessary. If a biopsy of the cerebral spinal fluid is taken, it is sent to a specialized laboratory for testing.[4]
Eastern equine encephalitis virus (EEEV) is closely related to Venezuelan equine encephalitis virus and western equine encephalitis virus.
Signs and symptoms
The incubation period for Eastern equine encephalitis virus (EEEV) disease ranges from 4 to 10 days. The illness can progress either systematically or encephalitically, depending on the person's age. Encephalitic disease involves swelling of the brain and can be asymptomatic, while the systemic illness occurs very abruptly. Those with the systemic illness usually recover within 1–2 weeks. While the encephalitis is more common among infants, in adults and children, it usually manifests after experiencing the systemic illness.[1] Symptoms include high fever, muscle pain, altered mental status, headache, meningeal irritation, photophobia, and seizures, which occur 3–10 days after the bite of an infected mosquito. Due to the virus's effect on the brain, affected individuals who survive can be left with mental and physical impairments, such as personality disorders, paralysis, seizures, and intellectual impairment.[1][5]
Cause
The causative agent, later identified as a togavirus, was first isolated from infected horse brains in 1933. In 1938, the first confirmed human cases were identified when 30 children died of encephalitis in the Northeastern United States. These cases coincided with outbreaks in horses in the same regions. The fatality rate in humans is 33%, and currently no cure is known for human infections. This virus has four variations in the types in lineage. The most common to the human disease is group 1, which is considered to be endemic in North America and the Caribbean, while the other three lineages, groups IIA, IIB, and III, are typically found in Central and South America, causing equine illness.[1]
These two clades may actually be distinct viruses.[6] The North American strains appear to be monotypic with a mutation rate of 2.7 × 10−4 substitutions/site/year (s/s/y). It appears to have diverged from the other strains 922 to 4,856 years ago. The other strains are divided into two main clades and a third smaller one. The two main clades diverged between 577 and 2,927 years ago. The mutation rate in the genome has been estimated to be 1.2 × 10−4 s/s/y.
Lifecycle
EEEV is capable of infecting a wide range of animals, including mammals, birds, reptiles, and amphibians. The virus is maintained in nature through a bird—mosquito cycle. Two mosquito species are primarily involved in this portion of the cycle; they are Culiseta melanura and Culiseta morsitans. These mosquitoes feed on the blood of birds. The frequency of the virus found in nature increases throughout the summer as more birds and more mosquitoes become infected.
Transmission of EEEV to mammals (including humans) occurs via other mosquito species, which feed on the blood of both birds and mammals. These other mosquitoes are referred to as "bridge vectors" because they carry the virus from the avian hosts to other types of hosts, particularly mammals. The bridge vectors include Aedes taeniorhynchus[7], Aedes vexans, Coquillettidia perturbans, Ochlerotatus canadensis, and Ochlerotatus sollicitans. Ochlerotatus canadensis also frequently bites turtles.Humans, horses, and most other infected mammals do not circulate enough viruses in their blood to infect additional mosquitoes. Some cases of EEE have been contracted through laboratory exposures or from exposure of the eyes, lungs, or skin wounds to brain or spinal cord matter from infected animals.
Diagnosis
In terms of the evaluation of EEE we find the following is done:[8]
- PCR analysis (blood or CSF)
- MRI
- Immunoassay
Prevention
The disease can be prevented in horses with the use of vaccinations, which are usually given with vaccinations for other diseases, most commonly western equine encephalitis virus, Venezuelan equine encephalitis virus, and tetanus. Most vaccinations for EEE consist of the killed virus. For humans, no vaccine for EEE is available; prevention involves reducing the risk of exposure. Using insect repellent, wearing protective clothing, and reducing the amount of standing water is the best means for prevention.[1]
Treatment
No cure for EEE has been found. Treatment consists of corticosteroids, anticonvulsants, and supportive measures (treating symptoms)[9] such as intravenous fluids, tracheal intubation, and antipyretics. About 4% of humans known to be infected develop symptoms, with a total of about six cases per year in the US.[9] A third of these cases die, and many survivors suffer permanent brain damage.[10]
Epidemiology
United States
Several states in the Northeast U.S. have had increased virus activity since 2004. Between 2004 and 2006, at least ten human cases of EEE were reported in Massachusetts. In 2006, about 500,000 acres (2,000 km2) in southeastern Massachusetts were treated with mosquito adulticides to reduce the risk of humans contracting EEE. Several human cases were reported in New Hampshire, as well.[11][12]
On 19 July 2012, the virus was identified in a mosquito of the species Coquillettidia perturbans in Nickerson State Park on Cape Cod, Massachusetts. On 28 July 2012, the virus was found in mosquitos in Pittsfield, Massachusetts.[13]
As of September 2019, a notable uptick in cases erupted in New England and Michigan, prompting some health departments to declare an outbreak.[14][15][16][17][18][19][20] As of 31 October 2019, five people died in Michigan,[21][22] three people died in Connecticut,[23] one person died in Rhode Island,[20] one person died in Alabama,[24] one person died in Indiana,[25] and three people died in Massachusetts.[26][27][28] The virus was also found in goats,[29] in turkeys,[30] in deer,[30] and in horses.[31][22][32][20][30]
As of September 9, 2020, there were 5 confirmed human cases between Massachusetts and Wisconsin.[33] As of October 9, 2020, one person died in Michigan,[34] and one person died in Wisconsin.[35]
Europe
In October 2007, a citizen of Livingston, West Lothian, Scotland became the first European victim of this disease. The man had visited New Hampshire during the summer of 2007, on a fishing vacation, and was diagnosed as having EEE on 13 September 2007. He fell ill with the disease on 31 August 2007, just one day after flying home, and later fell into a coma.[36] He later awoke from the coma with severe brain injuries.[37]
Biological weapon
EEEV was one of more than a dozen agents that the United States researched as potential biological weapons before the nation suspended its biological-weapons program in 1969, a few years before signing (1972) and then ratifying (1975) the Biological Weapons Convention.[38]
Other animals
After inoculation by the vector, the virus travels via lymphatics to lymph nodes, and replicates in macrophages and neutrophils, resulting in lymphopenia, leukopenia, and fever. Subsequent replication occurs in other organs, leading to viremia. Symptoms in horses occur 1–3 weeks after infection, and begin with a fever that may reach as high as 106 °F (41 °C). The fever usually lasts for 24–48 hours.
Nervous signs appear during the fever that include sensitivity to sound, periods of excitement, and restlessness. Brain lesions appear, causing drowsiness, drooping ears, circling, aimless wandering, head pressing, inability to swallow, and abnormal gait. Paralysis follows, causing the horse to have difficulty raising its head. The horse usually suffers complete paralysis and death 2–4 days after symptoms appear. Mortality rates among horses with the eastern strain range from 70 to 90%.
See also
- Western equine encephalitis virus
- Venezuelan equine encephalitis virus
References
- 1 2 3 4 5 6 "Eastern Equine Encephalitis". Centers for Disease Control and Prevention (CDC). Archived from the original on 10 March 2020. Retrieved 30 April 2017.
- ↑ "Eastern Equine Encephalomyelitis" (PDF). United States Department of Agriculture Animal and Plant Health Inspection Service. United States Department of Agriculture (USDA). Archived from the original (PDF) on 3 February 2017. Retrieved 1 May 2017.
- ↑ "Eastern Equine Encephalitis". Florida Health. Florida Health. Archived from the original on 8 October 2019. Retrieved 30 April 2017.
- ↑ Deresiewicz RL, Thaler SJ, Hsu L, Zamani AA (1997). "Clinical and neuroradiographic manifestations of eastern equine encephalitis". N. Engl. J. Med. 336 (26): 1867–74. doi:10.1056/NEJM199706263362604. PMID 9197215.
- ↑ Bleck, Thomas P.; Damon, Inger K. (2020). "359. Arboviruses affecting the central nervous system". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. p. 2230. ISBN 978-0-323-53266-2. Archived from the original on 10 September 2023. Retrieved 9 September 2023.
- ↑ Arrigo NC, Adams AP, Weaver SC (January 2010). "Evolutionary patterns of eastern equine encephalitis virus in North versus South America suggest ecological differences and taxonomic revision". J. Virol. 84 (2): 1014–25. doi:10.1128/JVI.01586-09. PMC 2798374. PMID 19889755.
- ↑ Kelser, R.A. (1937). "Transmission of the Virus of Equine Encephalomy-elîtis by Aëdes taeniorhynchus". Science (Washington). 85–2198 (2198): 178. Bibcode:1937Sci....85..178K. doi:10.1126/science.85.2198.178. PMID 17732932. Archived from the original on 15 April 2020. Retrieved 26 September 2022 – via cabdirect.org.
- ↑ Banda, Cecilia; Samanta, Debopam (2022). "Eastern Equine Encephalitis". StatPearls. StatPearls Publishing. Archived from the original on 30 October 2022. Retrieved 30 October 2022.
- 1 2 "Eastern Equine Encephalitis". Centers for Disease Control and Prevention (CDC). 16 August 2010. Archived from the original on 10 March 2020. Retrieved 7 August 2012.
- ↑ "Eastern Equine Encephalitis Fact Sheet". Centers for Disease Control and Prevention (CDC). 16 August 2010. Archived from the original on 10 March 2020. Retrieved 30 August 2015.
- ↑ Zheng Y (16 August 2008). "Mosquito-borne virus infects 2d in Mass". The Boston Globe. Archived from the original on 3 March 2016. Retrieved 26 September 2022.
- ↑ Zheng Y (31 August 2006). "Middleborough boy with EEE dies". The Boston Globe. Archived from the original on 2 September 2006. Retrieved 31 August 2006.
- ↑ Kane T (27 July 2012). "Rare, deadly virus found in mosquitoes in Pittsfield". News10. Archived from the original on 30 July 2012.
- ↑ Andersen T, McDonald D (6 September 2019). "Two more EEE human cases reported, raising the state's count to seven". The Boston Globe. Archived from the original on 14 November 2019. Retrieved 6 September 2019.
- ↑ "Why Is EEE Highest In Southeastern Massachusetts?". CBS Boston. 22 August 2019. Archived from the original on 23 August 2019. Retrieved 22 August 2019.
- ↑ "Second Human Case Of EEE Confirmed In Mass.; 10 More Towns Now At Critical Risk". CBS Boston. 16 August 2019. Archived from the original on 19 August 2019. Retrieved 22 August 2019.
- ↑ Seltz J (13 August 2019). "It's code red for EEE in nine communities south of Boston". The Boston Globe. Archived from the original on 15 August 2019. Retrieved 22 August 2019.
- ↑ Congi S (13 August 2019). "Massachusetts man infected with EEE now in coma, family says". WCVB-TV. Archived from the original on 23 August 2019. Retrieved 22 August 2019.
- ↑ LaPook J (21 September 2019). "7 dead from rare disease spread by mosquitoes". CBS News. Archived from the original on 21 September 2019. Retrieved 21 September 2019.
- 1 2 3 Almasy S (2 October 2019). "Connecticut Eastern equine encephalitis death is 10th nationwide". CNN. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ Miller K (2 October 2019). "Fourth person dies from mosquito-borne illness in Michigan". mlive. Archived from the original on 17 August 2022. Retrieved 3 October 2019.
- 1 2 Mahieu D (15 October 2019). "Fifth person in Michigan dies from Eastern Equine Encephalitis". UpNorthLive. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ Cuda A (1 September 2019). "Third person in state dies from EEE". Connecticut Post. Archived from the original on 17 October 2019. Retrieved 16 October 2019.
- ↑ Gore L (28 October 2019). "Mosquito-borne virus kills 1 in Alabama: What to know about EEE". al. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ "1st Eastern Equine Encephalitis Human Death Reported in Indiana". News18. 20 October 2019. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ Klein A (26 September 2019). "Mass. Health Officials Say 12th Person Has EEE, 1 Fewer Death". NBC10 Boston. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ Pescaro M, Klein A (25 September 2019). "UPDATE: Mass. Health Officials Give New Info on EEE-Related Deaths". NBC10 Boston. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ "Mass. retracts number of EEE deaths; confirms 12th human case of virus". The Boston Globe. 26 September 2019. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ Anderson DJ (17 August 2019). "A 2nd Person In Mass. Is Diagnosed With Mosquito-Linked EEE Disease". WBUR-FM. Archived from the original on 23 August 2019. Retrieved 22 August 2019.
- 1 2 3 "Pennsylvania Game Commission advises hunters to take precautions against EEE virus". Pittsburgh Tribune-Review. 22 October 2019. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ "18 Louisiana Horses Confirmed Positive for EEE or WNV". The Horse. 21 August 2019. Archived from the original on 21 August 2019. Retrieved 22 August 2019.
- ↑ Mulder J (1 October 2019). "Eastern equine encephalitis kills another horse in Oswego County". syracuse. Archived from the original on 14 November 2019. Retrieved 14 November 2019.
- ↑ "Michiganders urged to stay indoors as officials race to stop the spread of a dangerous mosquito-borne disease". CNN. Archived from the original on 9 December 2021. Retrieved 26 October 2020.
- ↑ "West Michigan resident with EEE dies". mlive. 2 October 2020. Archived from the original on 17 August 2022. Retrieved 26 October 2020.
- ↑ "Wisconsin woman dies of rare disease carried by mosquitoes". Milwaukee Journal Sentinel. Archived from the original on 28 September 2021. Retrieved 25 October 2020.
- ↑ "Man in coma after mosquito bite". BBC News Online. 8 October 2007. Archived from the original on 15 October 2007. Retrieved 26 September 2022.
- ↑ "Family thrilled by recovery of killer virus victim". The Scotsman. 22 December 2007. Archived from the original on 4 February 2020. Retrieved 4 February 2020.
- ↑ "Chemical and Biological Weapons: Possession and Programs Past and Present" (PDF). James Martin Center for Nonproliferation Studies, Middlebury College. March 2008. Archived (PDF) from the original on 27 March 2022. Retrieved 26 September 2022.
Further reading
- "Eastern Equine Encephalitis". Centers for Disease Control and Prevention (CDC). 17 December 2018. Archived from the original on 1 October 2022. Retrieved 26 September 2022.
- Source for a portion of this information: Evans, J.W.; Borton, A.; Hintz, H.F.; Van Vleck, L.D. (1977). The Horse. W.H. Freeman. ISBN 978-0716704911.
External links
| Classification |
|---|
- "Togaviridae". Virus Pathogen Database and Analysis Resource (ViPR).