Tetanus
| Tetanus | |
|---|---|
| Other names: Lockjaw | |
 | |
| Muscle spasms (specifically opisthotonos) in a person with tetanus. Painting by Sir Charles Bell, 1809. | |
| Specialty | Infectious disease |
| Symptoms | Muscle spasms, fever, headache[1] |
| Usual onset | 3–21 days following exposure[1] |
| Duration | Months[1] |
| Causes | Clostridium tetani[2] |
| Risk factors | Break in the skin[3] |
| Diagnostic method | Based on symptoms[1] |
| Prevention | Tetanus vaccine[1] |
| Treatment | Tetanus immune globulin, muscle relaxants, mechanical ventilation[1][4] |
| Prognosis | 10% risk of death[1] |
| Frequency | 209,000 (2015)[5] |
| Deaths | 56,700 (2015)[6] |
Tetanus, also known as lockjaw, is a bacterial infection characterized by muscle spasms.[1] In the most common type, the spasms begin in the jaw and then progress to the rest of the body.[1] Each spasm usually lasts a few minutes.[1] Spasms occur frequently for three to four weeks.[1] Some spasms may be severe enough to fracture bones.[7] Other symptoms of tetanus may include fever, sweating, headache, trouble swallowing, high blood pressure, and a fast heart rate.[1][7] Onset of symptoms is typically three to twenty-one days following infection.[1] Recovery may take months.[1] About ten percent of cases prove fatal.[1]
Tetanus is caused by an infection with the bacterium Clostridium tetani.[2] The organism is commonly found in soil, saliva, dust, and manure.[3] Illness generally occurs through a break in the skin such as a cut or puncture wound by a contaminated object.[3] Toxins secreted by C. tetani interfere with normal muscle contractions.[4] Diagnosis is based on the presenting signs and symptoms.[1] The disease does not spread between people.[1]
Tetanus can be prevented by immunization with the tetanus vaccine.[1] In those who have a significant wound and have had fewer than three doses of the vaccine, both vaccination and tetanus immune globulin are recommended.[1] The wound should be cleaned and any dead tissue should be removed.[1] In those who are infected, tetanus immune globulin or, if unavailable, intravenous immunoglobulin (IVIG) is used.[1] Muscle relaxants may be used to control spasms.[4] Mechanical ventilation may be required if a person's breathing is affected.[4]
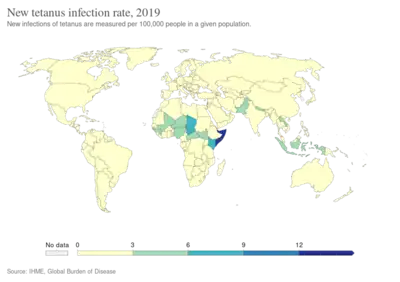
Tetanus occurs in all parts of the world but is most frequent in hot and wet climates where the soil has a high organic content.[1] In 2015 there were about 209,000 infections and about 59,000 deaths globally.[5][6] This is down from 356,000 deaths in 1990.[8] In the US there are about 30 cases per year, almost all of which have not been vaccinated.[9] An early description of the disease was made by Hippocrates in the 5th century BC.[1] The cause of the disease was determined in 1884 by Antonio Carle and Giorgio Rattone at the University of Turin, and a vaccine was developed in 1924.[1]
Signs and symptoms
Tetanus often begins with mild spasms in the jaw muscles—also known as lockjaw or trismus. The spasms can also affect the facial muscles resulting in an appearance called risus sardonicus. Chest, neck, back, abdominal muscles, and buttocks may be affected. Back muscle spasms often cause arching, called opisthotonos. Sometimes the spasms affect muscles that help with breathing, which can lead to breathing problems.[10]
Prolonged muscular action causes sudden, powerful, and painful contractions of muscle groups, which is called "tetany". These episodes can cause fractures and muscle tears. Other symptoms include fever, headache, restlessness, irritability, feeding difficulties, breathing problems, burning sensation during urination, urinary retention and loss of stool control.[11]
Even with treatment, about 10% of people who contract tetanus die.[1] The mortality rate is higher in unvaccinated people and people over 60 years of age.[1]
Incubation period
The incubation period of tetanus may be up to several months, but is usually about ten days.[12][13] In general, the farther the injury site is from the central nervous system, the longer the incubation period. The shorter the incubation period, the more severe the symptoms.[14] In neonatal tetanus (trismus nascentium), symptoms usually appear from 4 to 14 days after birth, averaging about 7 days. On the basis of clinical findings, four different forms of tetanus have been described.[1]
Generalized tetanus
Generalized tetanus is the most common type of tetanus, representing about 80% of cases. The generalized form usually presents with a descending pattern. The first sign is trismus, or lockjaw, and the facial spasms called risus sardonicus, followed by stiffness of the neck, difficulty in swallowing, and rigidity of pectoral and calf muscles. Other symptoms include elevated temperature, sweating, elevated blood pressure, and episodic rapid heart rate. Spasms may occur frequently and last for several minutes with the body shaped into a characteristic form called opisthotonos. Spasms continue for up to four weeks, and complete recovery may take months.[1]
Neonatal tetanus
Neonatal tetanus (trismus nascentium) is a form of generalized tetanus that occurs in newborns, usually those born to mothers who themselves have not been vaccinated. If the mother has been vaccinated against tetanus, the infants acquire passive immunity and are thus protected.[15] It usually occurs through infection of the unhealed umbilical stump, particularly when the stump is cut with a non-sterile instrument. As of 1998 neonatal tetanus was common in many developing countries and was responsible for about 14% (215,000) of all neonatal deaths.[16] In 2010 the worldwide death toll was 58,000 newborns. As the result of a public health campaign, the death toll from neonatal tetanus was reduced by 90% between 1990 and 2010, and by 2013 the disease had been largely eliminated from all but 25 countries.[17] Neonatal tetanus is rare in developed countries.
Local tetanus
Local tetanus is an uncommon form of the disease, in which people have persistent contraction of muscles in the same anatomic area as the injury. The contractions may persist for many weeks before gradually subsiding. Local tetanus is generally milder; only about 1% of cases are fatal, but it may precede the onset of generalized tetanus.[1]
Cephalic tetanus
Cephalic tetanus is the rarest form of the disease (0.9–3% of cases)[18] and is limited to muscles and nerves in the head.[19] It usually occurs after trauma to the head area, including skull fracture,[20] laceration,[20] eye injury,[19] dental extraction,[21] and otitis media,[22] but it has been observed from injuries to other parts of the body.[23] Paralysis of the facial nerve is most frequently implicated, which may cause lockjaw, facial palsy, or ptosis, but other cranial nerves can also be affected.[21][24] Cephalic tetanus may progress to a more generalized form of the disease.[18][24] Due to its rarity, clinicians may be unfamiliar with the clinical presentation and may not suspect tetanus as the illness.[19] Treatment can be complicated as symptoms may be concurrent with the initial injury that caused the infection.[20] Cephalic tetanus is more likely than other forms of tetanus to be fatal, with the progression to generalized tetanus carrying a 15–30% case fatality rate.[18][20][24]
Cause
Tetanus is caused by the tetanus bacterium Clostridium tetani.[1] Tetanus is an international health problem, as C. tetani endospores are ubiquitous. Endospores can be introduced into the body through a puncture wound (penetrating trauma). Due to C. tetani being an anaerobic bacterium, it and its endospores thrive in environments that lack oxygen, such as a puncture wound.
The disease occurs almost exclusively in persons inadequately immunized.[25] It is more common in hot, damp climates with soil rich in organic matter. Manure-treated soils may contain spores, as they are widely distributed in the intestines and feces of many animals such as horses, sheep, cattle, dogs, cats, rats, guinea pigs, and chickens.[1] In agricultural areas, a significant number of human adults may harbor the organism.
The spores can also be found on skin surfaces and in contaminated heroin.[1] Heroin users, particularly those who inject the drug subcutaneously, appear to be at high risk of contracting tetanus.[1] Rarely, tetanus can be contracted through surgical procedures, intramuscular injections, compound fractures, and dental infections.[1] Animal bites can transmit tetanus.[1]
Tetanus is often associated with rust, especially rusty nails. Although rust itself does not cause tetanus, objects that accumulate rust are often found outdoors or in places that harbor anaerobic bacteria. Additionally, the rough surface of rusty metal provides crevices for dirt containing C. tetani, while a nail affords a means to puncture skin and deliver endospores deep within the body at the site of the wound.[26] An endospore is a non-metabolizing survival structure that begins to metabolize and cause infection once in an adequate environment. Hence, stepping on a nail (rusty or not) may result in a tetanus infection, as the low-oxygen (anaerobic) environment may exist under the skin, and the puncturing object can deliver endospores to a suitable environment for growth.[27] It is a common misconception that rust itself is the cause and that a puncture from a rust-free nail is not a risk.[28][29]
 Photomicrograph of Gram-positive, Clostridium tetani bacteria. Note that several of these organisms had entered their endospore phase, assuming the characteristic tennis racket-type morphology.
Photomicrograph of Gram-positive, Clostridium tetani bacteria. Note that several of these organisms had entered their endospore phase, assuming the characteristic tennis racket-type morphology. Clostridium tetani is durable due to its endospores. Pictured is the bacterium alone, with a spore being produced, and the spore alone.
Clostridium tetani is durable due to its endospores. Pictured is the bacterium alone, with a spore being produced, and the spore alone.
Pathophysiology
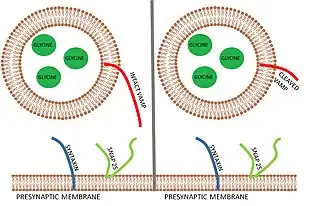
Tetanus neurotoxin (TeNT) binds to the presynaptic membrane of the neuromuscular junction, is internalized and is transported back through the axon until it reaches the central nervous system.[30] Here, it selectively binds to and is transported into inhibitory neurons via endocytosis.[31] It then leaves the vesicle for the neuron cytosol where it cleaves vesicle associated membrane protein (VAMP) synaptobrevin, which is necessary for membrane fusion of small synaptic vesicles (SSV's).[30] SSV's carry neurotransmitter to the membrane for release, so inhibition of this process blocks neurotransmitter release.
Tetanus toxin specifically blocks the release of the neurotransmitters GABA and glycine from inhibitory neurons. These neurotransmitters keep overactive motor neurons from firing and also play a role in the relaxation of muscles after contraction. When inhibitory neurons are unable to release their neurotransmitters, motor neurons fire out of control and muscles have difficulty relaxing. This causes the muscle spasms and spastic paralysis seen in tetanus infection.[30]
The tetanus toxin, tetanospasmin, is made up of a heavy chain and a light chain. There are three domains, each of which contributes to the pathophysiology of the toxin.[32] The heavy chain has two of the domains. The N-terminal side of the heavy chain helps with membrane translocation, and the C-terminal side helps the toxin locate the specific receptor site on the correct neuron. The light chain domain cleaves the VAMP protein once it arrives in the inhibitory neuron cytosol.[32]
There are four main steps tetanus's mechanism of action: binding to the neuron, internalization of the toxin, membrane translocation, and cleavage of the target VAMP.
Neurospecific binding
The toxin travels from the wound site to the neuromuscular junction through the bloodstream where it binds to the presynaptic membrane of a motor neuron. The heavy chain C-terminal domain aids in the binding to the correct site, recognizing and binding to the correct glycoproteins and glycolipids in the presynaptic membrane. The toxin binds to a site that will be taken into the neuron as an endocytic vesicle that will travel all the way down the axon, past the cell body, and down the dendrites to the dendritic terminal at the spine and central nervous system. Here it will be released into the synaptic cleft and allowed to bind with the presynaptic membrane of inhibitory neurons in a similar manner seen with the binding to the motor neuron.[31]
Internalization
Tetanus toxin is then internalized again via endocytosis, this time in an acidic vesicle.[32] In a mechanism not well understood, depolarization caused by the firing of the inhibitory neuron causes the toxin to be pulled into the neuron inside vesicles.
Membrane translocation
The toxin then needs a way to get out of the vesicle and into the neuron cytosol in order for it to act on its target. The low pH of the vesicle lumen causes a conformational change in the toxin, shifting it from a water-soluble form to a hydrophobic form.[31] With the hydrophobic patches exposed, the toxin is able to slide into the vesicle membrane. The toxin forms an ion channel in the membrane that is nonspecific for Na+, K+, Ca2+, and Cl- ions.[30] There is a consensus among experts that this new channel is involved in the translocation of the toxin's light chain from the inside of the vesicle to the neuron cytosol, but the mechanism is not well understood or agreed upon. It has been proposed that the channel could allow the light chain (unfolded from the low pH environment) to leave through the toxin pore,[33] or that the pore could alter the electrochemical gradient enough, by letting in or out ions, to cause osmotic lysis of the vesicle, spilling the vesicle's contents.[34]
Enzymatic target cleavage
The light chain of the tetanus toxin is a zinc-dependent protease. It shares a common zinc protease motif (His-Glu-Xaa-Xaa-His) that researchers hypothesized was essential for target cleavage until this was more recently confirmed by experiment: when all zinc was removed from the neuron with heavy metal chelators, the toxin was inhibited, only to be reactivated when the zinc was added back in.[30] The light chain binds to VAMP and cleaves it between Gln76 and Phe77. Without VAMP, vesicles holding the neurotransmitters needed for motor neuron regulation (GABA and Glycine) cannot be released, causing the above-mentioned deregulation of motor neurons and muscle tension.[35]
Diagnosis
There are currently no blood tests for diagnosing tetanus. The diagnosis is based on the presentation of tetanus symptoms and does not depend upon isolation of the bacterium, which is recovered from the wound in only 30% of cases and can be isolated from people without tetanus. Laboratory identification of C. tetani can be demonstrated only by production of tetanospasmin in mice.[1] Having recently experienced head trauma may indicate cephalic tetanus if no other diagnosis has been made.
The "spatula test" is a clinical test for tetanus that involves touching the posterior pharyngeal wall with a soft-tipped instrument and observing the effect. A positive test result is the involuntary contraction of the jaw (biting down on the "spatula") and a negative test result would normally be a gag reflex attempting to expel the foreign object. A short report in The American Journal of Tropical Medicine and Hygiene states that, in an affected subject research study, the spatula test had a high specificity (zero false-positive test results) and a high sensitivity (94% of infected people produced a positive test).[36]
Prevention
Unlike many infectious diseases, recovery from naturally acquired tetanus does not usually result in immunity to tetanus. This is due to the extreme potency of the tetanospasmin toxin. Tetanospasmin will likely be lethal before it will provoke an immune response.
Tetanus can be prevented by vaccination with tetanus toxoid.[37] The CDC recommends that adults receive a booster vaccine every ten years,[1] and standard care practice in many places is to give the booster to any person with a puncture wound who is uncertain of when he or she was last vaccinated, or if he or she has had fewer than three lifetime doses of the vaccine. The booster may not prevent a potentially fatal case of tetanus from the current wound, however, as it can take up to two weeks for tetanus antibodies to form.[38]
In children under the age of seven, the tetanus vaccine is often administered as a combined vaccine, DPT/DTaP vaccine, which also includes vaccines against diphtheria and pertussis. For adults and children over seven, the Td vaccine (tetanus and diphtheria) or Tdap (tetanus, diphtheria, and acellular pertussis) is commonly used.[37]
The World Health Organization certifies countries as having eliminated maternal or neonatal tetanus. Certification requires at least two years of rates of less than 1 case per 1000 live births. In 1998 in Uganda, 3,433 tetanus cases were recorded in newborn babies; of these, 2,403 died. After a major public health effort, Uganda in 2011 was certified as having eliminated tetanus.[39]
Post-exposure prophylaxis
Tetanus toxoid can be given in case of a suspected exposure to tetanus. In such cases, it can be given with or without tetanus immunoglobulin (also called tetanus antibodies or tetanus antitoxin[40]). It can be given as intravenous therapy or by intramuscular injection.
The guidelines for such events in the United States for non-pregnant people 11 years and older are as follows:[1]
| Vaccination status | Clean, minor wounds | All other wounds |
|---|---|---|
| Unknown or less than 3 doses of tetanus toxoid containing vaccine | Tdap and recommend catch-up vaccination | Tdap and recommend catch-up vaccination Tetanus immunoglobulin |
| 3 or more doses of tetanus toxoid containing vaccine AND less than 5 years since last dose | No indication | No indication |
| 3 or more doses of tetanus toxoid containing vaccine AND 5–10 years since last dose | No indication | Tdap preferred (if not yet received) or Td |
| 3 or more doses of tetanus toxoid containing vaccine AND more than 10 years since last dose | Tdap preferred (if not yet received) or Td | Tdap preferred (if not yet received) or Td |
Treatment
Mild tetanus
Mild cases of tetanus can be treated with:[41]
- tetanus immunoglobulin (TIG),[1] also called tetanus antibodies or tetanus antitoxin.[40] It can be given as intravenous therapy or by intramuscular injection.
- metronidazole IV for 10 days
- diazepam oral or IV
Severe tetanus
Severe cases will require admission to intensive care. In addition to the measures listed above for mild tetanus:[41]
- Human tetanus immunoglobulin injected intrathecally (increases clinical improvement from 4% to 35%)
- Tracheotomy and mechanical ventilation for 3 to 4 weeks. Tracheotomy is recommended for securing the airway because the presence of an endotracheal tube is a stimulus for spasm
- Magnesium sulfate, as an intravenous (IV) infusion, to control spasm and autonomic dysfunction
- Diazepam as a continuous IV infusion
- The autonomic effects of tetanus can be difficult to manage (alternating hyper- and hypotension hyperpyrexia/hypothermia) and may require IV labetalol, magnesium, clonidine, or nifedipine
Drugs such as diazepam or other muscle relaxants can be given to control the muscle spasms. In extreme cases it may be necessary to paralyze the person with curare-like drugs and use a mechanical ventilator.
In order to survive a tetanus infection, the maintenance of an airway and proper nutrition are required. An intake of 3,500 to 4,000 calories and at least 150 g of protein per day is often given in liquid form through a tube directly into the stomach (percutaneous endoscopic gastrostomy), or through a drip into a vein (parenteral nutrition). This high-caloric diet maintenance is required because of the increased metabolic strain brought on by the increased muscle activity. Full recovery takes 4 to 6 weeks because the body must regenerate destroyed nerve axon terminals.
The antibiotic of choice is metronidazole. It can be given as intravenously, by mouth, or by rectum.[42][41] Of likewise efficiency is penicillin, but some raise the concern of provoking spasms because it inhibits GABA receptor, which is already affected by tetanospasmin.[43]
Epidemiology

In 2013 it caused about 59,000 deaths – down from 356,000 in 1990.[8] Tetanus – in particular, the neonatal form – remains a significant public health problem in non-industrialized countries with 59,000 newborns worldwide dying in 2008 as a result of neonatal tetanus.[44][45] In the United States, from 2000 through 2007 an average of 31 cases were reported per year.[1] Nearly all of the cases in the United States occur in unimmunized individuals or individuals who have allowed their inoculations to lapse.[1]

History
Tetanus was well known to ancient people who recognized the relationship between wounds and fatal muscle spasms.[46] In 1884, Arthur Nicolaier isolated the strychnine-like toxin of tetanus from free-living, anaerobic soil bacteria. The etiology of the disease was further elucidated in 1884 by Antonio Carle and Giorgio Rattone, two pathologists of the University of Turin, who demonstrated the transmissibility of tetanus for the first time. They produced tetanus in rabbits by injecting pus from a person with fatal tetanus into their sciatic nerves.[1]
In 1891, C. tetani was isolated from a human victim by Kitasato Shibasaburō, who later showed that the organism could produce disease when injected into animals, and that the toxin could be neutralized by specific antibodies. In 1897, Edmond Nocard showed that tetanus antitoxin induced passive immunity in humans, and could be used for prophylaxis and treatment. Tetanus toxoid vaccine was developed by P. Descombey in 1924, and was widely used to prevent tetanus induced by battle wounds during World War II.[1]
Etymology
The word tetanus comes from the Ancient Greek: τέτανος, romanized: tetanos, lit. 'taut', which is further from the Ancient Greek: τείνειν, romanized: teinein, lit. 'to stretch'.[47]
Research
There is insufficient evidence to recommending treating or preventing tetanus with vitamin C.[48]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 Atkinson, William (May 2012). Tetanus Epidemiology and Prevention of Vaccine-Preventable Diseases (12 ed.). Public Health Foundation. pp. 291–300. ISBN 9780983263135. Archived from the original on February 13, 2015. Retrieved 12 February 2015.
 This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention. - 1 2 Barlow, Gavin; Irving, William L.; Moss, Peter J. (2020). "20. Infectious disease". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. pp. 546–547. ISBN 978-0-7020-7870-5. Archived from the original on 2023-01-14. Retrieved 2023-01-14.
- 1 2 3 "Tetanus Causes and Transmission". www.cdc.gov. January 9, 2013. Archived from the original on 12 February 2015. Retrieved 12 February 2015.
- 1 2 3 4 "Tetanus For Clinicians". cdc.gov. January 9, 2013. Archived from the original on 12 February 2015. Retrieved 12 February 2015.
- 1 2 Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- 1 2 Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- 1 2 "Tetanus Symptoms and Complications". cdc.gov. January 9, 2013. Archived from the original on 12 February 2015. Retrieved 12 February 2015.
- 1 2 Naghavi M, Wang H, Lozano R, Davis A, Liang X, Zhou M, et al. (GBD 2013 Mortality and Causes of Death Collaborators) (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ "About Tetanus". Centers for Disease Control and Prevention. United States Government. Archived from the original on 11 November 2014. Retrieved 4 August 2019.
- ↑ "Tetanus - Epidemiology of Vaccine Preventable Diseases". CDC. 2020-05-10. Archived from the original on 2020-05-10. Retrieved 2020-05-18.
Laryngospasm (spasm of the vocal cords) and/or spasm of the muscles of respiration leads to interference with breathing.
- ↑ Schleiss, Mark R. (2020). "Chapter 238: Tetanus". In Kliegman, Robert (ed.). Nelson Textbook of Pediatrics. Elsevier. p. 6253. ISBN 978-0-323-52950-1.
- ↑ Vandelaer J, Birmingham M, Gasse F, Kurian M, Shaw C, Garnier S (July 2003). "Tetanus in developing countries: an update on the Maternal and Neonatal Tetanus Elimination Initiative". Vaccine. 21 (24): 3442–5. doi:10.1016/S0264-410X(03)00347-5. PMID 12850356.
- ↑ Brauner JS, Vieira SR, Bleck TP (July 2002). "Changes in severe accidental tetanus mortality in the ICU during two decades in Brazil". Intensive Care Med. 28 (7): 930–5. doi:10.1007/s00134-002-1332-4. PMID 12122532. Archived from the original on 2021-08-29. Retrieved 2020-01-31.
- ↑ Farrar JJ, Yen LM, Cook T, Fairweather N, Binh N, Parry J, Parry CM (September 2000). "Tetanus". J. Neurol. Neurosurg. Psychiatry. 69 (3): 292–301. doi:10.1136/jnnp.69.3.292. PMC 1737078. PMID 10945801.
- ↑ "Tetanus and neonatal tetanus (NT)". WHO Western Pacific Region. Archived from the original on 2014-05-03.
- ↑ "Maternal and Neonatal Tetanus Elimination by 2005" (PDF). UNICEF. November 2000. Archived (PDF) from the original on 2007-01-11. Retrieved 2007-01-26.
- ↑ "Elimination of Maternal and Neonatal Tetanus". UNICEF. Archived from the original on 21 February 2014. Retrieved 17 February 2014.
- 1 2 3 Doshi A, Warrell C, Dahdaleh D, Kullmann D (February 2014). "Just a graze? Cephalic tetanus presenting as a stroke mimic". Pract Neurol. 14 (1): 39–41. doi:10.1136/practneurol-2013-000541. PMID 24052566.
- 1 2 3 Del Pilar Morales E, Bertrán Pasarell J, Cardona Rodriguez Z, Almodovar Mercado JC, Figueroa Navarro A (2014). "Cephalic tetanus following penetrating eye trauma: a case report". Bol Asoc Med P R. 106 (2): 25–9. PMID 25065047.
- 1 2 3 4 Adeleye AO, Azeez AL (October 2012). "Fatal tetanus complicating an untreated mild open head injury: a case-illustrated review of cephalic tetanus". Surgical Infections. 13 (5): 317–20. doi:10.1089/sur.2011.023. PMID 23039234.
- 1 2 Ajayi E, Obimakinde O (July 2011). "Cephalic tetanus following tooth extraction in a Nigerian woman". J Neurosci Rural Pract. 2 (2): 201–2. doi:10.4103/0976-3147.83597. PMC 3159367. PMID 21897694.
- ↑ Ugwu GI, Okolugbo NE (2012). "Otogenic tetanus: case series". West Afr J Med. 31 (4): 277–9. PMID 23468033.
- ↑ Kwon JC, Park Y, Han ZA, Song JE, Park HS (January 2013). "Trismus in cephalic tetanus from a foot injury". Korean J. Intern. Med. 28 (1): 121. doi:10.3904/kjim.2013.28.1.121. PMC 3543954. PMID 23346010.
- 1 2 3 Seo DH, Cho DK, Kwon HC, Kim TU (February 2012). "A case of cephalic tetanus with unilateral ptosis and facial palsy". Ann Rehabil Med. 36 (1): 167–70. doi:10.5535/arm.2012.36.1.167. PMC 3309317. PMID 22506253.
- ↑ Wells CL, Wilkins TD (1996). "Clostridia: Sporeforming Anaerobic Bacilli". In Baron S (ed.). Baron's Medical Microbiology. Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. Archived from the original on 2009-02-06.
- ↑ Edmonds, Molly (2009-07-29). "Causes of Tetanus". HowStuffWorks. Archived from the original on 22 November 2015. Retrieved 9 November 2015.
- ↑ Todar, Kenneth. "Tetanus". Lectures in Microbiology. University of Wisconsin, Madison - Dept. of Bacteriology. Archived from the original on 2013-03-11.
- ↑ O'Connor, Anahad (February 22, 2005), "The Claim: Stepping on a Rusty Nail Can Cause Tetanus", The New York Times, archived from the original on April 27, 2018, retrieved April 26, 2018
- ↑ Jennings K (2013-10-08). Because I Said So!: The Truth Behind the Myths, Tales, and Warnings Every Generation Passes Down to Its Kids. Simon and Schuster. pp. 13–. ISBN 978-1-4767-0696-2. Archived from the original on 2021-04-27. Retrieved 2018-04-26.
- 1 2 3 4 5 Pellizzari R, Rossetto O, Schiavo G, Montecucco C (February 1999). Clementi F, Fesce R, Meldolesi J, Valtorta F (eds.). "Tetanus and botulinum neurotoxins: mechanism of action and therapeutic uses". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 354 (1381): 259–68. doi:10.1098/rstb.1999.0377. PMC 1692495. PMID 10212474.
- 1 2 3 Montecucco C, Schiavo G (July 1994). "Mechanism of action of tetanus and botulinum neurotoxins". Molecular Microbiology. 13 (1): 1–8. doi:10.1111/j.1365-2958.1994.tb00396.x. PMID 7527117.
- 1 2 3 Masuyer G, Conrad J, Stenmark P (August 2017). "The structure of the tetanus toxin reveals pH-mediated domain dynamics". EMBO Reports. 18 (8): 1306–1317. doi:10.15252/embr.201744198. PMC 5538627. PMID 28645943.
- ↑ Beise J, Hahnen J, Andersen-Beckh B, Dreyer F (January 1994). "Pore formation by tetanus toxin, its chain and fragments in neuronal membranes and evaluation of the underlying motifs in the structure of the toxin molecule". Naunyn-Schmiedeberg's Archives of Pharmacology. 349 (1): 66–73. doi:10.1007/BF00178208. PMID 8139702. Archived from the original on 2021-08-29. Retrieved 2020-01-31.
- ↑ Cabiaux V, Lorge P, Vandenbranden M, Falmagne P, Ruysschaert JM (April 1985). "Tetanus toxin induces fusion and aggregation of lipid vesicles containing phosphatidylinositol at low pH". Biochemical and Biophysical Research Communications. 128 (2): 840–9. doi:10.1016/0006-291X(85)90123-8. PMID 3994725.
- ↑ Foran P, Shone CC, Dolly JO (December 1994). "Differences in the protease activities of tetanus and botulinum B toxins revealed by the cleavage of vesicle-associated membrane protein and various sized fragments". Biochemistry. 33 (51): 15365–74. doi:10.1021/bi00255a017. PMID 7803399.
- ↑ Apte NM, Karnad DR (October 1995). "Short Report: The Spatula Test: A Simple Bedside Test to Diagnose Tetanus". American Journal of Tropical Medicine and Hygiene. 53 (4): 386–7. doi:10.4269/ajtmh.1995.53.386. PMID 7485691.
- 1 2 "Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures. Recommendations of the Immunization Practices Advisory committee (ACIP)". MMWR. Recommendations and Reports. 40 (RR-10): 1–28. August 1991. PMID 1865873.
- ↑ Porter JD, Perkin MA, Corbel MJ, Farrington CP, Watkins JT, Begg NT (1992). "Lack of early antitoxin response to tetanus booster". Vaccine. 10 (5): 334–6. doi:10.1016/0264-410X(92)90373-R. PMID 1574917.
- ↑ "Uganda announces elimination of Maternal and Neonatal Tetanus". Archived from the original on 2015-02-11. Retrieved 2011-07-14.
- 1 2 tetanus in Encyclopædia Britannica. Last Updated 7-17-2013
- 1 2 3 World Health Organization. "Current recommendations for treatment of tetanus during humanitarian emergencies". Disease Control in Humanitarian Emergencies (English). WHO. Archived from the original on 13 March 2014. Retrieved 12 June 2013.
- ↑ Thwaites, C. Louise; Yen, Lam Minh (13 August 2018). "Tetanus". In J. Larry Jameson (ed.). Harrison's Principles of Internal Medicine, Twentieth Edition (Vol.1 & Vol.2). Anthony S. Fauci, Dennis L. Kasper, Stephen L. Hauser, Dan L. Longo, Joseph Loscalzo. McGraw-Hill Education. p. 2884. ISBN 978-1-259-64403-0. Archived from the original on 28 April 2021. Retrieved 25 February 2020.
- ↑ Rodrigo, Chaturaka; Fernando, Deepika; Rajapakse, Senaka (2014). "Pharmacological management of tetanus: an evidence-based review". Critical Care. Springer Science and Business Media LLC. 18 (2): 217. doi:10.1186/cc13797. ISSN 1364-8535.
- ↑ "Maternal and Neonatal Tetanus Elimination Initiative" (PDF). Pampers UNICEF 2010 Campaign: 2. Archived (PDF) from the original on 2014-02-01.
- ↑ Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. (June 2010). "Global, regional, and national causes of child mortality in 2008: a systematic analysis". Lancet. 375 (9730): 1969–87. doi:10.1016/S0140-6736(10)60549-1. PMID 20466419. Archived from the original on 2021-08-29. Retrieved 2020-01-31.
- ↑ Pearce JM (1996). "Notes on tetanus (lockjaw)". Journal of Neurology, Neurosurgery, and Psychiatry. 60 (3): 332. doi:10.1136/jnnp.60.3.332. PMC 1073859. PMID 8609513.
- ↑ tetanus Archived 2012-06-26 at the Wayback Machine. CollinsDictionary.com. Collins English Dictionary - Complete & Unabridged 11th Edition. Retrieved October 01, 2012
- ↑ Hemilä, Harri; Koivula, Teija (2013-11-13). "Vitamin C for preventing and treating tetanus". The Cochrane Database of Systematic Reviews (11): CD006665. doi:10.1002/14651858.CD006665.pub3. hdl:10138/225863. ISSN 1469-493X. PMID 24226506.
External links
- Tetanus Information from Medline Plus Archived 2016-07-05 at the Wayback Machine
- Tetanus Surveillance -- United States, 1998-2000 (Data and Analysis) Archived 2017-06-19 at the Wayback Machine
- "Tetanus". MedlinePlus. U.S. National Library of Medicine. Archived from the original on 2020-05-03. Retrieved 2020-05-20.
| Classification | |
|---|---|
| External resources |