Scarlet fever
| Scarlet fever | |
|---|---|
| Other names: Scarlatina[1] | |
 .jpg.webp) | |
| |
| Specialty | Infectious disease |
| Symptoms |
|
| Complications |
|
| Usual onset | School age children[3] |
| Duration | One week[1] |
| Causes | Strep throat, streptococcal skin infections[3] |
| Risk factors | Age 1 year to 15 years[3][5] |
| Diagnostic method | Throat swab, rapid streptococcal antigen test,[3] blood test for Anti-streptolysin O[2] |
| Differential diagnosis | Impetigo, erysipelas, measles, chickenpox, hand-foot-and-mouth disease, Kawasaki disease, toxic shock syndrome[2][6] |
| Prevention | Handwashing, not sharing personal items, staying away from sick people[3] |
| Treatment | Antibiotics, antipyretics[3] |
| Medication | Penicillin, amoxicillin, clindamycin, erythromycin[2][6] |
| Prognosis | Typically good[2] |
| Frequency | More common in low and middle income countries, males=females[6] |
| Deaths | Less than 1%[6] |
Scarlet fever is a widespread rash that occurs during a group A strep (GAS) infection.[1] It typically begins with a sore throat, fever, headache, body ache, nausea, and abdominal pain.[1] In addition to large tonsils and a red throat, small red spots on the roof of the mouth may be visible.[2] Glands in the neck may be enlarged and tender.[1] The rash is generally first noticed on the neck and torso before spread to the arms and legs.[7] It generally looks red on white skin; though, might be difficult to see on dark skin.[1] It typically feels like sandpaper and can be itchy.[8] The palms and soles are typically not involved.[7] A more intense redness may be noticed in skin folds.[6] The tongue may be red and bumpy and the cheeks flushed.[2][3] It takes around a week for the main rash to disappear, following which the skin sheds in fine flakes.[1] Symptoms begin 2 to 5 days after contact with the infection.[9]
It typically follows strep throat and less frequently from streptococcal skin infections, such as following an infected burn or surgical wound.[2] The bacteria are usually spread by coughing or sneezing.[3] It can also be spread when a person touches a contaminated object then touches their mouth or nose.[3] The rash occurs as a result of capillary damage by erythrogenic toxin-producing GAS.[10] Diagnosis may be confirmed by a throat swab or by rapid streptococcal antigen test.[11] A blood test showing a raised anti-streptolysin O confirms recent infection.[2] It may appear similar to Kawasaki disease, toxic shock syndrome, impetigo, erysipelas, measles, chickenpox, and hand-foot-and-mouth disease.[2][6] Scarlet fever during pregnancy is not known to harm the baby.[4]
There is no vaccine.[3] Prevention is by handwashing, not sharing personal items, and staying away from people who are sick.[3] Up to 80% of children develop lifelong immunity by the age of 10 years.[11] Treatment is with antibiotics, which prevent most complications.[3] Generally, 10 days of penicillin is the first choice of treatment.[1] Alternatives include amoxicillin, first-generation cephalosporin, clindamycin, or erythromycin.[2][6] Drinking cool water, eating soft foods, taking medications for fever, and applying calamine lotion to the skin may help with symptoms.[4] Outcomes are good if treated.[2] Long-term complications may include rheumatic heart disease, kidney disease, or arthritis.[3]
Scarlet fever most commonly affects children age 1 to 15 years.[3][5] Low and middle income countries see a greater number of cases.[6] It is seen more frequently when children are in school and in the winter.[1] Males and females are affected equally frequently.[6] Since 2011, mainland China, Hong Kong, South Korea, Taiwan, Singapore, Vietnam, and the United Kingdom have seen outbreaks.[12] It was possibly described as early as 400BC by Hippocrates.[13] In the early 20th century it was a leading cause of death in children, but its severity was already declining before the Second World War and the introduction of antibiotics, possibly as a result of better living conditions, introduction of control measures, and a lower virulence of the bacteria.[14][15]
Signs and symptoms
Scarlet fever typically begins with a sudden onset of sore throat, fever, headache, body ache, nausea, vomiting and abdominal pain.[1] A characteristic rash usually appears one to two days later but may appear before or up to seven days following feeling sick.[3] It generally hurts to swallow.[3] A cough, hoarseness, runny nose, diarrhea, and conjunctivitis are typically absent; their presence more likely to represent a viral cause.[16] Children younger than 3 years old can present with nasal congestion and a lower grade fever.[17] Infants may present with symptoms of increased irritability and decreased appetite.[17]
Mouth
Strep throat is usually associated with fatigue and a fever of over 39 °C (102.2 °F).[16] A red throat may be seen associated with small red spots on the hard and soft palate.[6] The uvula can look red and swollen.[1] The tonsils may appear red and enlarged and may be covered in exudate.[2] 30% to 60% of cases have associated enlarged and tender lymph nodes in the the neck.[1] During the first two days of illness the tongue may have a whitish coating from which red swollen papillae protrude, giving the appearance of a "white strawberry tongue"; after 4 to 5 days when the white coating sheds it becomes a "red strawberry tongue".[1]
 Large red tonsils with exudate
Large red tonsils with exudate Tonsillitis with exudate
Tonsillitis with exudate Red throat, red uvula, with red spots on soft palate
Red throat, red uvula, with red spots on soft palate
 White coating on tongue: white strawberry tongue
White coating on tongue: white strawberry tongue White coating sheds: strawberry tongue
White coating sheds: strawberry tongue Complete shedding of white coating: red strawberry tongue
Complete shedding of white coating: red strawberry tongue
Rash
The scarlet fever rash begins 1–2 days following the onset of sore throat, fever, fatigue.[2] It may begin on the neck or torso and then the arms and legs, or it might be first noticed on the trunk.[1] It generally looks red on white and pale skin, and might be difficult to visualise on brown or black skin, in whom the small bumps are typically larger.[1] It is made up of many fine small bumps over the body, which do not merge and therefore typically feel rough like sandpaper.[1] It can be mildly itchy, but not painful.[1] The palms and soles are typically not involved.[6] This characteristic rash has been denoted as "scarlatiniform," and may resemble goose bumps.[1][5] The reddened skin will blanch when pressure is applied to it.[1] Tiny red bumps merged together in a linear pattern on the inside of elbows, groin, neck or other skin folds might be noticed as a more intense redness.[1]
- Characteristic rash
 Intense redness in skin folds
Intense redness in skin folds Scarlet fever rash
Scarlet fever rash.jpg.webp) Scarlet fever rash on trunk
Scarlet fever rash on trunk Rash of scarlet fever in dark skin
Rash of scarlet fever in dark skin Facial flushing and classic rash of scarlet fever on white skin
Facial flushing and classic rash of scarlet fever on white skin
- Facial flushing
 Red cheeks and pale area around the mouth in scarlet fever
Red cheeks and pale area around the mouth in scarlet fever.jpg.webp) Facial redness
Facial redness
Skin peeling
Within one week of onset, the rash begins to fade followed by a longer process of desquamation, or shedding of the outer layer of skin.[1] It is typically shed in fine flakes of skin, directly proportionate to the extent of the rash and typically from the neck downwards.[1] This frequently last several weeks.[18] The desquamation process usually begins on the face and progresses downward on the body.[1] After the desquamation, the skin will be left with a sunburned appearance.[19] Sometimes, this peeling is the only sign that scarlet fever occurred.[2]
 Peeling of finger tip skin
Peeling of finger tip skin Peeling of hands
Peeling of hands Peeling of hands
Peeling of hands Skin peeling at elbow
Skin peeling at elbow.jpg.webp) Peeling of toes
Peeling of toes.jpg.webp) Peeling of toes
Peeling of toes
Complications
The complications, which can arise from scarlet fever when left untreated or inadequately treated, can be divided into suppurative and nonsuppurative.[6]
Suppurative complications: These are rare complications that arise either from direct spread to structures that are close to the primary site of infection, or spread through the lymphatic system or blood. In the first case, scarlet fever may spread to the pharynx. Possible problems from this method of spread include peritonsillar or retropharyngeal abscesses, cellulitis, mastoiditis or sinusitis. In the second case, the streptococcal infection may spread through the lymphatic system or the blood to areas of the body further away from the pharynx. A few examples of the many complications that can arise from those methods of spread include endocarditis, pneumonia, or meningitis.[20]
Nonsuppurative complications: These complications arise from certain subtypes of group A streptococci that cause an autoimmune response in the body through what has been termed molecular mimicry. In these cases, the antibodies which the person's immune system developed to attack the group A streptococci are also able to attack the person's own tissues. The following complications result, depending on which tissues in the person's body are targeted by those antibodies.[21]
- Acute rheumatic fever: This can affect the heart, skin, joints and brain.[22] This is a complication that results 2–6 weeks after a group A streptococcal infection of the upper respiratory tract.[19] It presents in developing countries, where antibiotic treatment of streptococcal infections is less common, as a febrile illness with several clinical manifestations, which are organized into what is called the Jones criteria. These criteria include arthritis, carditis, neurological issues, and skin findings.[17] Diagnosis also depends on evidence of a prior group A streptococcal infection in the upper respiratory tract (as seen in streptococcal pharyngitis and scarlet fever).[17] The carditis is the result of the immunologic response targeting the person's heart tissue, and it is the most serious sequelae that develops from acute rheumatic fever. When this involvement of the heart tissue occurs, it is called rheumatic heart disease.[17] In most cases of rheumatic heart disease, the mitral valve is affected, ultimately leading to mitral stenosis.[17]
- Poststreptococcal glomerulonephritis: This is inflammation of the kidney, which presents 1–2 weeks after a group A streptococcal pharyngitis. It can also develop after an episode of Impetigo or any group A streptococcal infection in the skin (this differs from acute rheumatic fever which only follows group A streptococcal pharyngitis).[19][23] It is the result of the autoimmune response to the streptococcal infection affecting part of the kidney. Persons present with what is called acute nephritic syndrome, in which they have high blood pressure, swelling, and urinary abnormalities. Urinary abnormalities include blood and protein found in the urine, as well as less urine production overall.[19] While the risk of this side effect has often been stated to not be reduced by the use of antibiotics, others have stated that antibiotics may decrease the risk.[24]
- Poststreptococcal reactive arthritis: The presentation of arthritis after a recent episode of group A streptococcal pharyngitis raises suspicion for acute rheumatic fever, since it is one of the Jones criteria for that separate complication. But, when the arthritis is an isolated symptom, it is referred to as poststreptococcal reactive arthritis. This arthritis can involve a variety of joints throughout the body, unlike the arthritis of acute rheumatic fever, which primarily affects larger joints such as the knee joints. It can present less than 10 days after the group A streptococcal pharyngitis.[19]
Cause
The characteristic rash of scarlet fever occurs as a result of capillary damage by erythrogenic toxin-producing GAS.[10] It typically follows a strep throat and less frequently from streptococcal skin infections such as following a burn or surgical wound.[2] Spread occurs mainly when an infected person is in close contact with another person, allowing direct transmission of large droplets containing the bacteria; usually by coughing or sneezing.[1] It can also be spread via contaminated surfaces; a person touches an object that has GAS on it and then touches their mouth or nose.[3] People can transmit the bacteria before they show symptoms, and may have no symptoms for 12 hours to 7 days.[1] In a household with an affected case, around half of family members become infected.[1] Around 15% to 20% of children are asymptomatic carriers.[7]
One in ten children who are infected with group A streptococcal pharyngitis will develop scarlet fever.[18]
Pathophysiology
The characteristic rash is due to capillary damage by erythrogenic toxin-producing GAS.[10] These toxin-producing strains cause scarlet fever in people who do not already have antitoxin antibodies. Streptococcal pyrogenic exotoxins A, B, and C (speA, speB, and speC) have been identified. The pyrogenic exotoxins are also called erythrogenic toxins and cause the erythematous rash of scarlet fever.[19] The strains of group A streptococcus that cause scarlet fever need specific bacteriophages in order for there to be pyrogenic exotoxin production. Specifically, bacteriophage T12 is responsible for the production of speA.[25] Streptococcal Pyrogenic Exotoxin A, speA, is the one which is most commonly associated with cases of scarlet fever which are complicated by the immune-mediated sequelae acute rheumatic fever and post-streptococcal glomerulonephritis.[2]
These toxins are also known as “superantigens” because they are able to cause an extensive immune response within the body through activation of some of the main cells responsible for the person's immune system.[12] The body responds to these toxins by making antibodies to those specific toxins. However, those antibodies do not completely protect the person from future group A streptococcal infections, because there are 12 different pyrogenic exotoxins possible.[19]
Microbiology
The disease is caused by secretion of pyrogenic exotoxins by the infecting Streptococcus bacteria.[26][27] Streptococcal pyrogenic exotoxin A (speA) is probably the best studied of these toxins. It is carried by the bacteriophage T12 which integrates into the streptococcal genome from where the toxin is transcribed. The phage itself integrates into a serine tRNA gene on the chromosome.[28]
The T12 virus itself has not been placed into a taxon by the International Committee on Taxonomy of Viruses. It has a double-stranded DNA genome and on morphological grounds appears to be a member of the Siphoviridae.
The speA gene was cloned and sequenced in 1986.[29] It is 753 base pairs in length and encodes a 29.244 kiloDalton (kDa) protein. The protein contains a putative 30- amino-acid signal peptide; removal of the signal sequence gives a predicted molecular weight of 25.787 kDa for the secreted protein. Both a promoter and a ribosome binding site (Shine-Dalgarno sequence) are present upstream of the gene. A transcriptional terminator is located 69 bases downstream from the translational termination codon. The carboxy terminal portion of the protein exhibits extensive homology with the carboxy terminus of Staphylococcus aureus enterotoxins B and C1.
Streptococcal phages other than T12 may also carry the speA gene.[30]
Diagnosis
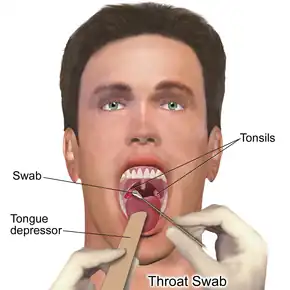
Although the presentation of scarlet fever can be clinically diagnosed, further testing may be required to distinguish it from other illnesses.[1] Also, history of a recent exposure to someone with strep throat can be useful in diagnosis.[19] There are two methods used to confirm suspicion of scarlet fever; rapid antigen detection test and throat culture.[17]
The rapid antigen detection test is a very specific test but not very sensitive. This means that if the result is positive (indicating that the group A strep antigen was detected and therefore confirming that the person has a group A strep pharyngitis), then it is appropriate to treat the patient with antibiotics. But, if the rapid antigen detection test is negative (indicating that they do not have group A strep pharyngitis), then a throat culture is required to confirm, as the first test could have yielded a false negative result.[31] In the early 21st century, the throat culture is the current "gold standard" for diagnosis.[17]
Serologic testing seeks evidence of the antibodies that the body produces against the streptococcal infection, including antistreptolysin-O and antideoxyribonuclease B. It takes the body 2–3 weeks to make these antibodies, so this type of testing is not useful for diagnosing a current infection. But, it is useful when assessing a person who may have one of the complications from a previous streptococcal infection.[18][17]
Throat cultures done after antibiotic therapy can show if the infection has been removed. These throat swabs, however, are not indicated, because up to 25% of properly treated individuals can continue to carry the streptococcal infection while being asymptomatic.[23]
Differential diagnosis
Scarlet fever presents with varying severities and symptoms.[1] Not all cases present with a fever, the degree of tiredness varies, the sore throat and tongue changes might be slight or absent, and the rash can be patchy in some.[1] Scarlet fever might appear similar to Kawasaki disease, which has a characteristic red but not white strawberry tongue, and staphylococcal scarlatina which does not have the strawberry tongue at all.[2] Other conditions that might appear similar include impetigo, erysipelas, measles, chickenpox, and hand-foot-and-mouth disease, and may be distinguished by the pattern of symptoms.[6]
- Viral exanthem: Viral infections are often accompanied by a rash which can be described as morbilliform or maculopapular. This type of rash is accompanied by a prodromal period of cough and runny nose in addition to a fever, indicative of a viral process.[21]
- Allergic or contact dermatitis: The erythematous appearance of the skin will be in a more localized distribution rather than the diffuse and generalized rash seen in scarlet fever.[18]
- Drug eruption: These are potential side effects of taking certain drugs such as penicillin. The reddened maculopapular rash which results can be itchy and be accompanied by a fever.[32]
- Kawasaki disease: Children with this disease also present a strawberry tongue and undergo a desquamative process on their palms and soles. However, these children tend to be younger than 5 years old, their fever lasts longer (at least five days), and they have additional clinical criteria (including signs such as conjunctival redness and cracked lips), which can help distinguish this from scarlet fever.[33]
- Toxic shock syndrome: Both streptococcal and staphylococcal bacteria can cause this syndrome. Clinical manifestations include diffuse rash and desquamation of the palms and soles. It can be distinguished from scarlet fever by low blood pressure, lack of sandpaper texture for the rash, and multi-organ system involvement.[34]
- Staphylococcal scalded skin syndrome: This is a disease that occurs primarily in young children due to a toxin-producing strain of the bacteria Staphylococcus aureus. The abrupt start of the fever and diffused sunburned appearance of the rash can resemble scarlet fever. However, this rash is associated with tenderness and large blister formation. These blisters easily pop, followed by causing the skin to peel.[35]
- Staphylococcal scarlet fever: The rash is identical to the streptococcal scarlet fever in distribution and texture, but the skin affected by the rash will be tender.[1]
Prevention
One method is long-term use of antibiotics to prevent future group A streptococcal infections. This method is only indicated for people who have had complications like recurrent attacks of acute rheumatic fever or rheumatic heart disease. Antibiotics are limited in their ability to prevent these infections since there are a variety of subtypes of group A streptococci that can cause the infection.[19]
The vaccine approach has a greater likelihood of effectively preventing group A streptococcal infections because vaccine formulations can target multiple subtypes of the bacteria.[19] A vaccine developed by George and Gladys Dick in 1924 was discontinued due to poor efficacy and the introduction of antibiotics. Difficulties in vaccine development include the considerable strain variety of group A streptococci present in the environment and the amount of time and number of people needed for appropriate trials for safety and efficacy of any potential vaccine.[36] There have been several attempts to create a vaccine in the past few decades. These vaccines, which are still in the development phase, expose the person to proteins present on the surface of the group A streptococci to activate an immune response that will prepare the person to fight and prevent future infections.[37]
Treatment
Treatment is with antibiotics; to reduce transmission of the bacteria to others and to reduce suppurative and nonsuppurative complications, especially acute rheumatic fever.[1] Generally, 10 days of penicillin is the first choice.[1] Alternative medicines include amoxicillin, a first-generation cephalosporin, clindamycin, and erythromycin.[6] Another option is dicloxacillin.[2] Drinking cool water, eating soft foods, taking antipyretics for fever and applying calamine lotion to the skin for itch, may help to feel better.[4] Outcomes with scarlet fever are good if treated.[2] Peeling of the outer layer of skin, however, will happen despite treatment.[1]
As long as antibiotics are started within nine days, it is very unlikely for the child to develop acute rheumatic fever.[19] An infected individual is most likely to pass on the infection to another person during the first 2 weeks.[23] A child is no longer contagious (able to pass the infection to another child) after 24 hours of antibiotics.[19] Benzathine Penicillin G can be given as a one time intramuscular injection as another alternative if swallowing is not possible.[38]
Antibiotic resistance
A drug-resistant strain of scarlet fever, resistant to macrolide antibiotics such as erythromycin, but retaining drug-sensitivity to beta-lactam antibiotics such as penicillin, emerged in Hong Kong in 2011, accounting for at least two deaths in that city—the first such in over a decade.[39] About 60% of circulating strains of the group A streptococcus that cause scarlet fever in Hong Kong are resistant to macrolide antibiotics, says Professor Kwok-yung Yuen, head of Hong Kong University's microbiology department. Previously, observed resistance rates had been 10–30%; the increase is likely the result of overuse of macrolide antibiotics in recent years.
Epidemiology
Scarlet fever occurs equally in both males and females.[6] Children are most commonly infected, typically between 5–15 years old.[6] Although streptococcal infections can happen at any time of year, infection rates peak in the winter and spring months, typically in temperate climates.[6]
The morbidity and mortality of scarlet fever has declined since the 18th and 19th century when there were epidemics caused by this disease.[40] Around 1900 the mortality rate in multiple places reached 25%.[41] The improvement in prognosis can be attributed to the use of penicillin in the treatment of this disease.[16] The frequency of scarlet fever cases has also been declining over the past century. There have been several reported outbreaks of the disease in various countries in the past decade.[42] The reason for these recent increases remains unclear in the medical community. Between 2013 and 2016 population rates of scarlet fever in England increased from 8.2 to 33.2 per 100,000 and hospital admissions for scarlet fever increased by 97%.[43]
History
It was possibly described as early as 400BC by Hippocrates.[13] The first description of the disease in the medical literature appeared in the 1553 book De Tumoribus praeter Naturam by the Sicilian anatomist and physician Giovanni Filippo Ingrassia, where he referred to it as rossalia.[13] He also made a point to distinguish that this presentation had different characteristics to measles.[13] It was redescribed by Johann Weyer during an epidemic in lower Germany between 1564 and 1565; he referred to it as scalatina anginosa.[13] The first unequivocal description of scarlet fever appeared in a book by Joannes Coyttarus of Poitiers, De febre purpura epidemiale et contagiosa libri duo, which was published in 1578 in Paris.[13] Daniel Sennert of Wittenberg described the classical 'scarlatinal desquamation' in 1572 and was also the first to describe the early arthritis, scarlatinal dropsy, and ascites associated with the disease.[13]
In 1675 the term that has been commonly used to refer to scarlet fever, "scarlatina", was written by Thomas Sydenham, an English physician.[13] In 1827, Richard Bright was the first to recognize the involvement of the renal system in scarlet fever. The association between streptococci and disease was first described in 1874 by Theodor Billroth, discussing people with skin infections.[13] Billroth also coined the genus name Streptococcus.[13] In 1884 Friedrich Julius Rosenbach edited the name to its current one, Streptococcus pyogenes, after further looking at the bacteria in the skin lesions.[13] The organism was first cultured in 1883 by the German surgeon Friedrich Fehleisen from erysipelas lesions.[13] In 1884, the German physician Friedrich Loeffler was the first to show the presence of streptococci in the throats of people with scarlet fever. Because not all people with pharyngeal streptococci developed scarlet fever, these findings remained controversial for some time. The association between streptococci and scarlet fever was confirmed by Alphonse Dochez and George and Gladys Dick in the early 1900s.[44]
Scarlet fever serum from horses' blood was used in the treatment of children beginning in 1900 and reduced mortality rates significantly.
In 1906, the Austrian pediatrician Clemens von Pirquet postulated that disease-causing immune complexes were responsible for the nephritis that followed scarlet fever.[45]
Bacteriophages were discovered in 1915 by Frederick Twort. His work was overlooked and bacteriophages were later rediscovered by Felix d'Herelle in 1917. The specific association of scarlet fever with the group A streptococci had to await the development of Lancefield's streptococcal grouping scheme in the 1920s. George and Gladys Dick showed that cell-free filtrates could induce the erythematous reaction characteristic of scarlet fever, proving that this reaction was due to a toxin. Karelitz and Stempien discovered that extracts from human serum globulin and placental globulin can be used as lightening agents for scarlet fever and this was used later as the basis for the Dick test. The association of scarlet fever and bacteriophages was described in 1926 by Cantucuzene and Boncieu.[46]
An antitoxin for scarlet fever was developed in 1924.
There used to be a diphtheria scarlet fever vaccine.[47] It was, however, found not to be effective.[48] This product was discontinued by the end of World War II.
The first toxin which causes this disease was cloned and sequenced in 1986 by Weeks and Ferretti.[29] The discovery of penicillin and its subsequent widespread use has significantly reduced the mortality of this once feared disease. Reports of cases of scarlet fever have been on the rise in countries including England, Wales, South Korea, Vietnam, China, and Hong Kong in recent years. Researchers are unsure as to what has caused the spike in cases of the disease.[49][50]
Dick test
The Dick test, invented in 1924 by George F. Dick and Gladys Dick, was used to identify those susceptible to scarlet fever.[51] The Dick test consisted of injecting a diluted strain of the streptococci known to cause scarlet fever into a person's skin. A local reaction in the skin at the site of injection appeared in people who were susceptible to developing scarlet fever. This reaction was most notable around 24 hours after the injection but could be seen as early as 4–6 hours. If there is no reaction seen in the skin, then that person was assumed to have already developed immunity to the disease and was not at risk of developing it.[52]
.jpg.webp) Otto Kalischer wrote a doctoral thesis on scarlet fever in 1891.
Otto Kalischer wrote a doctoral thesis on scarlet fever in 1891._(8211297109).jpg.webp) A 1930s American poster attempting to curb the spread of such diseases as scarlet fever by regulating milk supply
A 1930s American poster attempting to curb the spread of such diseases as scarlet fever by regulating milk supply.jpg.webp) Gladys Henry Dick (pictured) and George Frederick Dick developed an antitoxin and vaccine for scarlet fever in 1924 which were later eclipsed by penicillin in the 1940s.
Gladys Henry Dick (pictured) and George Frederick Dick developed an antitoxin and vaccine for scarlet fever in 1924 which were later eclipsed by penicillin in the 1940s.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 Michaels, Marian `G.; Williams, John V. (2023). "13. Infectious diseases". In Zitelli, Basil J.; McIntire, Sara C.; Nowalk, Andrew J.; Garrison, Jessica (eds.). Zitelli and Davis' Atlas of Pediatric Physical Diagnosis (8th ed.). Philadelphia: Elsevier. pp. 468–469. ISBN 978-0-323-77788-9. Archived from the original on 8 April 2023. Retrieved 29 June 2023.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "14. Bacterial infections". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 259-260. ISBN 978-0-323-54753-6. Archived from the original on 13 December 2022. Retrieved 11 December 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 "Scarlet Fever: All You Need to Know". Center for Disease Control and Prevention. 31 October 2022. Archived from the original on 8 December 2022. Retrieved 9 December 2022.
- 1 2 3 4 "Scarlet fever". nhs.uk. 19 October 2017. Archived from the original on 8 December 2022. Retrieved 9 December 2022.
- 1 2 3 Paller, Amy S.; Mancini, Anthony J. (2022). "16. Exanthemous diseases of childhood". Paller and Mancini - Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. St. Louis, Missouri: Elsevier. pp. 449–450. ISBN 978-0-323-54988-2. Archived from the original on 19 December 2022. Retrieved 19 December 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Pardo, Salvatore; Perera, Thomas B. (2022). "Scarlet Fever". StatPearls. StatPearls Publishing. PMID 29939666. Archived from the original on 23 March 2022. Retrieved 9 December 2022.
- 1 2 3 Stevens, Dennis L.; Bryant, Amy E.; Hagman, Melissa M. (2020). "274. Nonpneumococcal streptococcal infections and rheumatic fever". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. p. 1873. ISBN 978-0-323-55087-1. Archived from the original on 14 December 2022. Retrieved 14 December 2022.
- ↑ Denny, George O.; Cohen, Bernard A. (2022). "7. Reactive erythema". In Cohen, Bernard A. (ed.). Pediatric Dermatology. Philadelphia: Elsevier. p. 191-192. ISBN 978-0-7020-7963-4. Archived from the original on 14 December 2022. Retrieved 14 December 2022.
- ↑ "Scarlet fever: symptoms, diagnosis and treatment". GOV.UK. Archived from the original on 11 December 2022. Retrieved 11 December 2022.
- 1 2 3 Stevens, Dennis L.; Bryant, Amy E. (2022). "21. Life-threatening skin and soft tissue infections". In Jong, Elaine C.; Stevens, Dennis L. (eds.). Netter's Infectious Diseases (2nd ed.). Elsevier. p. 95. ISBN 978-0-323-71159-3. Archived from the original on 11 December 2022. Retrieved 11 December 2022.
- 1 2 "Scarlet fever: Causes, Treatment, and Outcome — DermNet". dermnetnz.org. Archived from the original on 18 August 2022. Retrieved 9 December 2022.
- 1 2 Hurst, Jacklyn R.; Brouwer, Stephan; Walker, Mark J.; McCormick, John K. (30 December 2021). "Streptococcal superantigens and the return of scarlet fever". PLOS Pathogens. 17 (12): e1010097. doi:10.1371/journal.ppat.1010097. ISSN 1553-7374. PMID 34969060. Archived from the original on 30 May 2022. Retrieved 13 December 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 Ferretti, Joseph; Kohler, Werner (February 2016). "History of Streptococcal Research". Streptococcus Pyogenes: Basic Biology to Clinical Manifestations. PMID 26866232.
- ↑ Smallman-Raynor, Matthew (2012). Atlas of epidemic Britain : a twentieth century picture. Oxford: Oxford University Press. p. 48. ISBN 9780199572922. Archived from the original on 14 February 2017.
- ↑ Welte, Alex; Williams, Brian; Hitchcock, Gavin (2017). "5.18. Mathematical models of transmission and control of infectious agents". In Detels, Roger; Gulliford, Martin; Karim, Quarraisha Abdool; Tan, Chorh Chuan (eds.). Oxford Textbook of Global Public Health. Vol. 1 (6th ed.). Oxford University Press. pp. 648–650. ISBN 978-0-19-871930-4. Archived from the original on 19 December 2022. Retrieved 18 December 2022.
- 1 2 3 Wessels, Michael R. (2016). Ferretti, Joseph J.; Stevens, Dennis L.; Fischetti, Vincent A. (eds.). Streptococcus pyogenes : Basic Biology to Clinical Manifestations. Oklahoma City (OK): University of Oklahoma Health Sciences Center. PMID 26866221. Archived from the original on 3 March 2021. Retrieved 28 January 2018.
- 1 2 3 4 5 6 7 8 9 Langlois DM, Andreae M (October 2011). "Group A streptococcal infections". Pediatrics in Review. 32 (10): 423–9, quiz 430. doi:10.1542/pir.32-10-423. PMID 21965709. S2CID 207170856.
- 1 2 3 4 Usatine, Richard (2013). Color Atlas of Family Medicine, Second Edition. McGraw Hill Companies.
- 1 2 3 4 5 6 7 8 9 10 11 12 Kliegman, Robert; Stanton, Bonita; St Geme, Joseph; Schor, Nina (2016). Nelson Textbook of Pediatrics. Elsevier. pp. 1327–1337.
- ↑ Bennett, John; Dolin, Raphael; Blaser, Martin (2015). Mandell, Douglas and Bennett's Principles and Practice of Infectious Disease, Eighth Edition. Saunders. pp. 2285–2299.
- 1 2 Kaspar, Dennis; Fauci, Anthony; Hauser, Stephen; Longo, Dan; Jameson, J. Larry; Loscalzo, Joseph (2015). Harrison's Principles of Internal Medicine, 19th edition. McGraw Hill Education.
- ↑ Babbar, Anshu (2015). "1. Streptococcus pyogenes". Streptococcal Superantigens. Heidelberg: Springer. p. 2. ISBN 978-3-319-22454-1. Archived from the original on 19 December 2022. Retrieved 18 December 2022.
- 1 2 3 Tanz, Robert (2018). "Sore Throat". Nelson Pediatric Symptom-Based Diagnosis. Elsevier. pp. 1–14.
- ↑ Sainato, Rebecca J.; Weisse, Martin E. (January 2019). "Poststreptococcal Glomerulonephritis and Antibiotics: A Fresh Look at Old Data". Clinical Pediatrics. 58 (1): 10–12. doi:10.1177/0009922818793345. ISSN 0009-9228.
- ↑ McShan, W. Michael (February 1997). "Bacteriophage T12 of Streptococcus pyogenes integrates into the gene encoding a serine tRNA". Molecular Microbiology. 23 (4): 719–728. doi:10.1046/j.1365-2958.1997.2591616.x. PMID 9157243.
- ↑ Zabriskie, J. B. (1964). "The role of temperate bacteriophage in the production of erythrogenic toxin by Group A Streptococci". Journal of Experimental Medicine. 119 (5): 761–780. doi:10.1084/jem.119.5.761. PMC 2137738. PMID 14157029.

- ↑ Krause, R. M. (2002). "A Half-century of Streptococcal Research: Then & Now". Indian Journal of Medical Research. 115: 215–241. PMID 12440194.
- ↑ McShan, W. M.; Ferretti, J. J. (1997). "Genetic diversity in temperate bacteriophages of Streptococcus pyogenes: identification of a second attachment site for phages carrying the erythrogenic toxin A gene". Journal of Bacteriology. 179 (20): 6509–6511. doi:10.1128/jb.179.20.6509-6511.1997. PMC 179571. PMID 9335304.
- 1 2 Weeks, C. R.; Ferretti, J. J. (1986). "Nucleotide sequence of the type A streptococcal exotoxin (erythrogenic toxin) gene from Streptococcus pyogenes bacteriophage T12". Infection and Immunity. 52 (1): 144–150. doi:10.1128/IAI.52.1.144-150.1986. PMC 262210. PMID 3514452.
- ↑ Yu, C. E.; Ferretti, J. J. (1991). "Molecular characterization of new group A streptococcal bacteriophages containing the gene for streptococcal erythrogenic toxin A (speA)". Molecular and General Genetics. 231 (1): 161–168. doi:10.1007/BF00293833. PMID 1753942. S2CID 36197596.
- ↑ American Academy of Pediatrics (2013). Baker, Carol (ed.). Red Book Atlas of Pediatric Infectious Diseases. American Academy of Pediatrics. pp. 473–476. ISBN 9781581107951.
- ↑ Ferri, Fred (2009). Ferri's Color Atlas and Text of Clinical Medicine. Saunders. pp. 47–48.
- ↑ Kato, Hirohisa (2010). Cardiology, Third Edition. Elsevier. pp. 1613–1626.
- ↑ Habif, Thomas (2016). Clinical Dermatology. Elsevier. pp. 534–576.
- ↑ Adams, James (2013). Emergency Medicine Clinical Essentials. Saunders. pp. 149–158.
- ↑ "Initiative for Vaccine Research (IVR)—Group A Streptococcus". World Health Organization. Archived from the original on 13 May 2012. Retrieved 15 June 2012.
- ↑ Chih-Feng, Kuo; Tsao, Nina; I-Chen, Hsieh; Yee-Shin, Lin; Jiunn-Jong, Wu; Yu-Ting, Hung (March 2017). "Immunization with a streptococcal multiple-epitope recombinant protein protects mice against invasive group A streptococcal infection". PLOS ONE. 12 (3): e0174464. Bibcode:2017PLoSO..1274464K. doi:10.1371/journal.pone.0174464. PMC 5371370. PMID 28355251.
- ↑ Ferri, Fred (2018). Ferri's Clinical Advisor 2018. Elsevier. p. 1143.
- ↑ "Second HK child dies of mutated scarlet fever". Associated Press (online). 22 June 2011. Archived from the original on 24 June 2011. Retrieved 23 June 2011.
- ↑ "Managing scarlet fever". BMJ. 362: k3005. 2018. doi:10.1136/bmj.k3005. ISSN 0959-8138. PMID 30166279. S2CID 52136139.
- ↑ Guerrant, Richard; Walker, David; Weller, Peter (2011). Tropical Infectious Diseases: Principles, Pathogens and Practice. Elsevier. pp. 203–211. ISBN 9780702039355.
- ↑ Basetti, S.; Hodgson, J.; Rawson, T.M.; Majeed, A. (August 2017). "Scarlet Fever: A guide for general practitioners". London Journal of Primary Care. 9 (5): 77–79. doi:10.1080/17571472.2017.1365677. PMC 5649319. PMID 29081840.
- ↑ "Scarlet fever in England reaches highest level in 50 years". Pharmaceutical Journal. 30 November 2017. Archived from the original on 26 January 2020. Retrieved 2 January 2018.
- ↑ "Archive copy" (PDF). Archived (PDF) from the original on 24 February 2021. Retrieved 28 April 2019.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ Huber, B. (2006). "100 years of allergy: Clemens von Pirquet—his idea of allergy and its immanent concept of disease" (PDF). Wiener klinische Wochenschrift. 118 (19–20): 573–579. doi:10.1007/s00508-006-0701-3. PMID 17136331. S2CID 46144926. Archived (PDF) from the original on 1 May 2019. Retrieved 27 June 2019.
- ↑ Cantacuzène, J.; Bonciu, O. (1926). "Modifications subies par des streptocoques d'origine non scarlatineuse au contact de produits scarlatineux filtrès". Comptes rendus de l'Académie des Sciences (in français). 182: 1185–1187.
- ↑ Rudolf Franck - Moderne Therapie in Innerer Medizin und Allgemeinpraxis - Ein Handbuch der Medikamentösen, Physikalischen und Diätetischen Behandlungsweisen der Letzten Jahre. Springer Verlag. 13 August 2013. ISBN 9783662221860. Archived from the original on 9 January 2017. Retrieved 9 January 2017.
- ↑ Ellis, Ronald W.; Brodeur, Bernard R. (2012). New Bacterial Vaccines. Springer Science & Business Media. p. 158. ISBN 9781461500537. Archived from the original on 9 January 2017.
- ↑ Lamagni, Theresa; Guy, Rebecca; Chand, Meera (2018). "Resurgence of scarlet fever in England, 2014–16: a population-based surveillance study". The Lancet Infectious Diseases. The Lancet: Infectious Disease. 18 (2): 180–187. doi:10.1016/S1473-3099(17)30693-X. PMID 29191628.
- ↑ Branswell, Helen (27 November 2017). "Scarlet fever, a disease of yore, is making a comeback in parts of the world". STAT. Archived from the original on 28 November 2017. Retrieved 28 November 2017.
- ↑ Dick, G. F.; Dick, G. H. (1924). "A skin test for susceptibility to scarlet fever". Journal of the American Medical Association. 82 (4): 265–266. doi:10.1001/jama.1924.02650300011003.
- ↑ Claude, B; McCartney, J.E.; McGarrity, J. (January 1925). "The Dick test for susceptibility to scarlet fever". The Lancet. 205 (5292): 230–231. doi:10.1016/S0140-6736(00)56009-7.
External links
| Classification |
|---|
