Abdominal obesity
| Abdominal obesity | |
|---|---|
| Other names | Central obesity, truncal obesity; see also § Colloquialisms |
 | |
| An abdominous obese male Weight: 182 kg/400 lbs Height: 185 cm/6 ft 1 in. Body mass index: 53 | |
| Specialty | Endocrinology |
| Complications | Heart disease, asthma, stroke, diabetes |
| Causes | Sedentary lifestyle, Overeating, Cushing's syndrome, Alcoholism, Polycystic ovarian syndrome, Prader-Willi syndrome |
Abdominal obesity, also known as central obesity and truncal obesity, is a condition when excessive abdominal fat around the stomach and abdomen has built up to the extent that it is likely to have a negative impact on health. Abdominal obesity has been strongly linked to cardiovascular disease,[1] Alzheimer's disease, and other metabolic and vascular diseases.[2]
Visceral and central abdominal fat and waist circumference show a strong association with type 2 diabetes.[3]
Visceral fat, also known as organ fat or intra-abdominal fat, is located inside the peritoneal cavity, packed in between internal organs and torso, as opposed to subcutaneous fat, which is found underneath the skin, and intramuscular fat, which is found interspersed in skeletal muscle. Visceral fat is composed of several adipose depots including mesenteric, epididymal white adipose tissue (EWAT), and perirenal fat. An excess of adipose visceral fat is known as central obesity, the "pot belly" or "beer belly" effect, in which the abdomen protrudes excessively. This body type is also known as "apple shaped", as opposed to "pear shaped" in which fat is deposited on the hips and buttocks.
Researchers first started to focus on abdominal obesity in the 1980s when they realized it had an important connection to cardiovascular disease, diabetes, and dyslipidemia. Abdominal obesity was more closely related with metabolic dysfunctions connected with cardiovascular disease than was general obesity. In the late 1980s and early 1990s insightful and powerful imaging techniques were discovered that would further help advance the understanding of the health risks associated with body fat accumulation. Techniques such as computed tomography and magnetic resonance imaging made it possible to categorize mass of adipose tissue located at the abdominal level into intra-abdominal fat and subcutaneous fat.[4]
Health risks
Heart disease
Abdominal obesity is associated with a statistically higher risk of heart disease, hypertension, insulin resistance, and type 2 diabetes (see below).[5] With an increase in the waist to hip ratio and overall waist circumference the risk of death increases as well.[6] Metabolic syndrome is associated with abdominal obesity, blood lipid disorders, inflammation, insulin resistance, full-blown diabetes, and increased risk of developing cardiovascular disease.[7][8][9][10] It is now generally believed that intra-abdominal fat is the depot that conveys the biggest health risk.[4][11]
Recent validation has concluded that total and regional body volume estimates correlate positively and significantly with biomarkers of cardiovascular risk and BVI calculations correlate significantly with all biomarkers of cardio-vascular risk.[12]
Diabetes
There are numerous theories as to the exact cause and mechanism in type 2 diabetes. Central obesity is known to predispose individuals for insulin resistance. Abdominal fat is especially active hormonally, secreting a group of hormones called adipokines that may possibly impair glucose tolerance. But adiponectin, an anti-inflammatory adipokine, which is found in lower concentration in obese and diabetic individuals has shown to be beneficial and protective in type 2 diabetes mellitus (T2DM).[13][14]
Insulin resistance is a major feature of diabetes mellitus type 2 , and central obesity is correlated with both insulin resistance and T2DM itself.[15][16] Increased adiposity (obesity) raises serum resistin levels,[17][18][19][20] which in turn directly correlate to insulin resistance.[21][22][23][24] Studies have also confirmed a direct correlation between resistin levels and T2DM.[17][25][26][27] And it is waistline adipose tissue (central obesity) which seems to be the foremost type of fat deposits contributing to rising levels of serum resistin.[28][29] Conversely, serum resistin levels have been found to decline with decreased adiposity following medical treatment.[30]
Asthma
Developing asthma due to abdominal obesity is also a main concern. As a result of breathing at low lung volume, the muscles are tighter and the airway is narrower. Obesity causes decreased tidal volumes due to reduced in chest expansion that is caused both by the weight on the chest itself and the effect of abdominal obesity on flattening the diaphragms.[31] It is commonly seen that people who are obese breathe quickly and often, while inhaling small volumes of air.[32] People with obesity are also more likely to be hospitalized for asthma. A study has stated that 75% of patients treated for asthma in the emergency room were either overweight or obese.[33]
Alzheimer's disease
Based on studies, it is evident that obesity has a strong association with vascular and metabolic disease which could potentially be linked to Alzheimer's disease. Recent studies have also shown an association between mid-life obesity and dementia, but the relationship between later life obesity and dementia is less clear.[2] A study by Debette et al. (2010) examining over 700 adults found evidence to suggest higher volumes of visceral fat, regardless of overall weight, were associated with smaller brain volumes and increased risk of dementia.[34][35][36] Alzheimer's disease and abdominal obesity has a strong correlation and with metabolic factors added in, the risk of developing Alzheimer's disease was even higher. Based on logistic regression analyses, it was found that obesity was associated with an almost 10-fold increase risk of Alzheimer's disease.[2]
Other health risks
Central obesity can be a feature of lipodystrophies, a group of diseases that is either inherited, or due to secondary causes (often protease inhibitors, a group of medications against AIDS). Central obesity is a symptom of Cushing's syndrome[37] and is also common in patients with polycystic ovary syndrome (PCOS). Central obesity is associated with glucose intolerance and dyslipidemia. Once dyslipidemia becomes a severe problem, an individual's abdominal cavity would generate elevated free fatty acid flux to the liver. The effect of abdominal adiposity occurs not just in those who are obese, but also affects people who are non-obese and it also contributes to insulin sensitivity.
Ghroubi et al. (2007) examined whether abdominal circumference is a more reliable indicator than BMI of the presence of knee osteoarthritis in obese patients.[38] They found that it actually appears to be a factor linked with the presence of knee pain as well as osteoarthritis in obese study subjects. Ghroubi et al. (2007) concluded that a high abdominal circumference is associated with great functional repercussion.[38]
Causes
Diet
The currently prevalent belief is that the immediate cause of obesity is net energy imbalance—the organism consumes more usable calories than it expends, wastes, or discards through elimination. Some studies indicate that visceral adiposity, together with lipid dysregulation and decreased insulin sensitivity,[39] is related to the excessive consumption of fructose.[40][41][42] Some evidence shows that in regards to juveniles, when free fructose is present as children's fat cells mature, it makes more of these cells mature into fat cells in the abdominal region. It also caused both visceral fat and subcutaneous fat to be less sensitive to insulin. These effects were not attenuated when compared to similar glucose consumption.[43]
Intake of trans fat from industrial oils has been associated with increased abdominal obesity in men[44] and increased weight and waist circumference in women.[45] These associations were not attenuated when fat intake and calorie intake was accounted for.[46][47] Greater meat (processed meat, red meat, & poultry) consumption has also been positively associated with greater weight gain, and specifically abdominal obesity, even when accounting for calories.[48][49] Conversely, studies suggest that oily fish consumption is negatively associated with total body fat and abdominal fat distribution even when body mass remains constant.[50][51] Similarly, increased soy protein consumption is correlated with lower amounts of abdominal fat in postmenopausal women even when calorie consumption is controlled.[52][53]
Numerous large studies have demonstrated that eating ultraprocessed food[54] has a positive dose-dependent relationship with both abdominal obesity and general obesity in both men and women. Consuming a diet rich in unprocessed food and minimally processed food is linked with lower obesity risk, lower waist circumference and less chronic disease. These findings are consistent among American,[55] Canadian,[56] Latin American,[57] British,[58] Australian,[59] French,[60] Spaniard,[61] South Korean[62] Chinese,[63] and Sub-Saharan African[64] populations.
Obesity plays an important role in the impairment of lipid and carbohydrate metabolism shown in high-carbohydrate diets.[65] It has also been shown that quality protein intake during a 24-hour period and the number of times the essential amino acid threshold of approximately 10 g[66] has been achieved is inversely related to the percentage of central abdominal fat. Quality protein uptake is defined as the ratio of essential amino acids to daily dietary protein.[67]
Visceral fat cells will release their metabolic by-products in the portal circulation, where the blood leads straight to the liver. Thus, the excess of triglycerides and fatty acids created by the visceral fat cells will go into the liver and accumulate there. In the liver, most of it will be stored as fat. This concept is known as 'lipotoxicity'.[68]
Alcohol consumption
A study has shown that alcohol consumption is directly associated with waist circumference and with a higher risk of abdominal obesity in men, but not in women. After controlling for energy under-reporting, which have slightly attenuated these associations, it was observed that increasing alcohol consumption significantly increased the risk of exceeding recommended energy intakes in male participants – but not in the small number of female participants (2.13%) with elevated alcohol consumption, even after establishing a lower number of drinks per day to characterize women as consuming a high quantity of alcohol. Further research is needed to determine whether a significant relationship between alcohol consumption and abdominal obesity exists among women who consume higher amounts of alcohol.[69]
A systemic review and meta-analysis failed to find data pointing towards a dose-dependent relationship between beer intake and general obesity or abdominal obesity at low or moderate intake levels (under ~500 mL/day). However, high beer intake (above ~4 L/wk) appeared to be associated with a higher degree of abdominal obesity specifically, particularly among men.[70]
Other factors
Other environmental factors, such as maternal smoking, estrogenic compounds in the diet, and endocrine-disrupting chemicals may be important also.[71]
Hypercortisolism, such as in Cushing's syndrome, also leads to central obesity. Many prescription drugs, such as dexamethasone and other steroids, can also have side effects resulting in central obesity,[37] especially in the presence of elevated insulin levels.
The prevalence of abdominal obesity is increasing in Western populations, possibly due to a combination of low physical activity and high-calorie diets, and also in developing countries, where it is associated with the urbanization of populations.[72][73]
Waist measurement (e.g., for BFP standard) is more prone to errors than measuring height and weight (e.g., for BMI standard). It is recommended to use both standards. BMI will illustrate the best estimate of one's total body fatness, while waist measurement gives an estimate of visceral fat and risk of obesity-related disease.[74]
Diagnosis
There are various ways of measuring abdominal obesity including:
- Absolute waist circumference (>102 cm (40 in) in men and >88 cm (35 in) in women)[75]
- Waist–hip ratio (the circumference of the waist divided by that of the hips of >0.9 for men and >0.85 for women)[1]
- Waist-stature ratio (waist circumference divided by their height, >0.5 for adults under 40 and >0.6 for adults over 50)
- Sagittal Abdominal Diameter[76]

In those with a body mass index (BMI) under 35, intra-abdominal body fat is related to negative health outcomes independent of total body fat.[77] Intra-abdominal or visceral fat has a particularly strong correlation with cardiovascular disease.[1]
BMI and waist measurements are well recognized ways to characterize obesity. However, waist measurements are not as accurate as BMI measurements. For this reason, it is recommended to use both methods of measurements.[78]
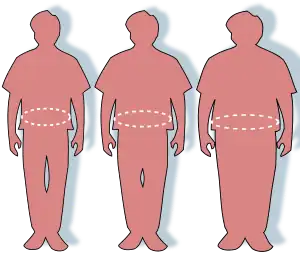
While central obesity can be obvious just by looking at the naked body (see the picture), the severity of central obesity is determined by taking waist and hip measurements. The absolute waist circumference 102 centimetres (40 in) in men and 88 centimetres (35 in) in women and the waist-hip ratio (>0.9 for men and >0.85 for women)[1] are both used as measures of central obesity. A differential diagnosis includes distinguishing central obesity from ascites and intestinal bloating. In the cohort of 15,000 people participating in the National Health and Nutrition Examination Survey (NHANES III), waist circumference explained obesity-related health risk better than BMI when metabolic syndrome was taken as an outcome measure and this difference was statistically significant. In other words, excessive waist circumference appears to be more of a risk factor for metabolic syndrome than BMI.[79] Another measure of central obesity which has shown superiority to BMI in predicting cardiovascular disease risk is the Index of Central Obesity (waist-to-height ratio, WHtR), where a ratio of >=0.5 (i.e. a waist circumference at least half of the individual's height) is predictive of increased risk.[80] Another diagnosis of obesity is the analysis of intra-abdominal fat having the most risk to one's personal health. The increased amount of fat in this region relates to the higher levels of plasma lipid and lipoproteins as per studies mentioned by Eric Poehlman (1998) review.[4] An increasing acceptance of the importance of central obesity within the medical profession as an indicator of health risk has led to new developments in obesity diagnosis such as the Body Volume Index, which measures central obesity by measuring a person's body shape and their weight distribution. The effect of abdominal adiposity occurs not just in those who are obese, but also affects people who are non-obese and it also contributes to insulin sensitivity.
Index of central obesity
Index of Central Obesity (ICO) is the ratio of waist circumference and height first proposed by a Parikh et al. in 2007[81] as a better substitute to the widely used waist circumference in defining metabolic syndrome.[82] The National Cholesterol Education Program Adult Treatment Panel III suggested cutoff of 102 cm (40 in) and 88 cm (35 in) for males and females as a marker of central obesity.[75] The same was used in defining metabolic syndrome.[83] Misra et al. suggested that these cutoffs are not applicable among Indians and the cutoffs be lowered to 90 cm (35 in) and 80 cm (31 in) for males and females.[84] Various race specific cutoffs were suggested by different groups.[85] The International Diabetes Federation defined central obesity based on these various race and gender specific cutoffs.[86] The other limitation of waist circumference is that it the measurement procedure has not been standardized and in children there are no, or few, comparison standards or reference data.[87]
Parikh et al. looked at the average heights of various races and suggested that by using ICO various race- and gender-specific cutoffs of waist circumference can be discarded.[82] An ICO cutoff of 0.53 was suggested as a criterion to define central obesity. Parikh et al. further tested a modified definition of metabolic syndrome in which waist circumference was replaced with ICO in the National Health and Nutrition Examination Survey (NHANES) database and found the modified definition to be more specific and sensitive.[82]
This parameter has been used in the study of metabolic syndrome[88][89] and cardiovascular disease.[90]
Central obesity in individuals with normal BMI is referred to as normal weight obesity.
Sex differences
50% of men and 70% of women in the United States between the ages of 50 and 79 years now exceed the waist circumference threshold for central obesity. [91]
When comparing the body fat of men and women it is seen that men have close to twice the visceral fat as that of pre-menopausal women. [92][93]
Central obesity is positively associated with coronary heart disease risk in women and men. It has been hypothesized that the sex differences in fat distribution may explain the sex difference in coronary heart disease risk.[94]
There are sex-dependent differences in regional fat distribution. In women, estrogen is believed to cause fat to be stored in the buttocks, thighs, and hips.[95] When women reach menopause and the estrogen produced by ovaries declines, fat migrates from their buttocks, hips, and thighs to their belly.[96][97]
Males are more susceptible to upper-body fat accumulation, most likely in the belly, due to sex hormone differences.[98] Abdominal obesity in males is correlated with comparatively low testosterone levels.[99] Testosterone administration significantly increased thigh muscle area, reduced subcutaneous fat deposition at all levels measured, but slightly increased the visceral fat area.[100]
Even with the differences, at any given level of central obesity measured as waist circumference or waist to hip ratio, coronary artery disease rates are identical in men and women.[101]
Management
A permanent routine of exercise, eating healthily, and, during periods of being overweight, consuming the same number or fewer calories than used will prevent and help fight obesity.[102] A single pound of fat yields approximately 3500 calories of energy (32 000 kJ energy per kilogram of fat), and weight loss is achieved by reducing energy intake,[103] or increasing energy expenditure, thus achieving a negative balance. Adjunctive therapies which may be prescribed by a physician are orlistat or sibutramine, although the latter has been associated with increased cardiovascular events and strokes and has been withdrawn from the market in the US,[104] the UK,[105] the EU,[106] Australia,[107] Canada,[108] Hong Kong,[109] and Thailand.[110]
A 2006 study published in the International Journal of Sport Nutrition and Exercise Metabolism,[111] suggests that combining cardiovascular (aerobic) exercise with resistance training is more effective than cardiovascular training alone in getting rid of abdominal fat. An additional benefit to exercising is that it reduces stress and insulin levels, which reduce the presence of cortisol, a hormone that leads to more belly fat deposits and leptin resistance.[112]
Self-motivation by understanding the risks associated with abdominal obesity is widely regarded as being far more important than worries about cosmetics. In addition, understanding the health issues linked with abdominal obesity can help in the self-motivation process of losing the abdominal fat. As mentioned above, abdominal fat is linked with cardiovascular disease, diabetes, and cancer. Specifically it's the deepest layer of belly fat (the fat that cannot seen or grabbed) that poses health risks, as these "visceral" fat cells produce hormones that can affect health (e.g. increased insulin resistance and/or breast cancer risk). The risk increases considering the fact that they are located in the proximity or in between organs in the abdominal cavity. For example, fat next to the liver drains into it, causing a fatty liver, which is a risk factor for insulin resistance, setting the stage for type 2 diabetes. However, visceral fat is more responsive to the circulation of catecholamines.
In the presence of type 2 diabetes, the physician might instead prescribe metformin and thiazolidinediones (rosiglitazone or pioglitazone) as antidiabetic drugs rather than sulfonylurea derivatives. Thiazolidinediones may cause slight weight gain but decrease "pathologic" abdominal fat (visceral fat), and therefore may be prescribed for diabetics with central obesity.[113] Thiazolidinedione has been associated with heart failure and increased cardiovascular risk; so it has been withdrawn from the market in Europe by EMA in 2010.[114]
Low-fat diets may not be an effective long-term intervention for obesity: as Bacon and Aphramor wrote, "The majority of individuals regain virtually all of the weight that was lost during treatment."[115] The Women's Health Initiative ("the largest and longest randomized, controlled dietary intervention clinical trial"[115]) found that long-term dietary intervention increased the waist circumference of both the intervention group and the control group, though the increase was smaller for the intervention group. The conclusion was that mean weight decreased significantly in the intervention group from baseline to year 1 by 2.2 kg (P<.001) and was 2.2 kg less than the control group change from baseline at year 1. This difference from baseline between control and intervention groups diminished over time, but a significant difference in weight was maintained through year 9, the end of the study.[116]
Society and culture
Myths
There is a common misconception that spot exercise (that is, exercising a specific muscle or location of the body) most effectively burns fat at the desired location, but this is not the case. Spot exercise is beneficial for building specific muscles, but it has little effect, if any, on fat in that area of the body, or on the body's distribution of body fat. The same logic applies to sit-ups and belly fat. Sit-ups, crunches and other abdominal exercises are useful in building the abdominal muscles, but they have little effect, if any, on the adipose tissue located there.[117]
Colloquialisms
A large central adiposity deposit has been assigned many common use names, including; "spare tire", "paunch", and "potbelly".[118] Several colloquial terms used to refer to central obesity, and to people who have it, refer to beer drinking. However, there is little scientific evidence that beer drinkers are more prone to central obesity, despite its being known colloquially as "beer belly", "beer gut", or "beer pot". One of the few studies conducted on the subject did not find that beer drinkers are more prone to central obesity than nondrinkers or drinkers of wine or spirits.[119][120] Chronic alcoholism can lead to cirrhosis, symptoms of which include gynecomastia (enlarged breasts) and ascites (abdominal fluid). These symptoms can suggest the appearance of central obesity.
Deposits of excess fat at the sides of one's waistline or obliques are commonly referred to as "love handles".
Economics
Researchers in Copenhagen examined the relationship between waist circumferences and costs among 31,840 subjects aged 50–64 years of age with different waist circumferences. Their study showed that an increase in just an additional centimetre above normal waistline caused a 1.25% and 2.08% rise in health care costs in women and men respectively. To put this in perspective, a woman with a waistline of 95 cm (approx 37.4 in) and without underlying health problems or co-morbidities can incur economic costs that are 22%, or US$397, higher per year than a woman with a normal waist circumference.[121]
See also
- Bariatrics, the branch of medicine that deals with the causes, prevention, and treatment of obesity
- Lipoatrophy, the term describing the localized loss of fat tissue
- Normal weight obesity, normal BMI with excessive fat, usually centrally localized
- Panniculus, hanging belly fat
- Steatosis, also called fatty change, fatty degeneration or adipose degeneration
- Muffin top
References
- 1 2 3 4 Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. (2004). "Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study". Lancet. 364 (9438): 937–52. doi:10.1016/S0140-6736(04)17018-9. hdl:10983/21615. PMID 15364185. S2CID 30811593.
- 1 2 3 Razay G, Vreugdenhil A, Wilcock G (2006). "Obesity, abdominal obesity and Alzheimer disease". Dementia and Geriatric Cognitive Disorders. 22 (2): 173–6. doi:10.1159/000094586. PMID 16847377. S2CID 24351283.
- ↑ Anjana M, Sandeep S, Deepa R, Vimaleswaran KS, Farooq S, Mohan V (December 2004). "Visceral and central abdominal fat and anthropometry in relation to diabetes in Asian Indians". Diabetes Care. 27 (12): 2948–53. doi:10.2337/diacare.27.12.2948. PMID 15562212.
- 1 2 3 Poehlman ET (1998). "Abdominal Obesity: The Metabolic Multi-risk Factor". Coronary Heart Disease. Exp. 9 (8): 469–471. doi:10.1097/00019501-199809080-00001. S2CID 57778374.
- ↑ Westphal SA (2008). "Obesity, abdominal obesity, and insulin resistance". Clinical Cornerstone. 9 (1): 23–29, discussion 30–1. doi:10.1016/S1098-3597(08)60025-3. PMID 19046737.
- ↑ Cameron AJ, Zimmet PZ (April 2008). "Expanding evidence for the multiple dangers of epidemic abdominal obesity". Circulation. 117 (13): 1624–6. doi:10.1161/CIRCULATIONAHA.108.775080. PMID 18378623.
- ↑ Després JP, Lemieux I (December 2006). "Abdominal obesity and metabolic syndrome". Nature. 444 (7121): 881–7. Bibcode:2006Natur.444..881D. doi:10.1038/nature05488. PMID 17167477. S2CID 11944065.
- ↑ Expert Panel On Detection, Evaluation (May 2001). "Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III)". JAMA. 285 (19): 2486–97. doi:10.1001/jama.285.19.2486. PMID 11368702.
- ↑ Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant D, for the Conference Participants. Definition of metabolic syndrome: report of the National, Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433-438.
- ↑ "American Heart Association's description of Syndrome X". Americanheart.org. Retrieved 2013-01-05.
- ↑ Mørkedal B, Romundstad PR, Vatten LJ (June 2011). "Informativeness of indices of blood pressure, obesity and serum lipids in relation to ischaemic heart disease mortality: the HUNT-II study". European Journal of Epidemiology. 26 (6): 457–61. doi:10.1007/s10654-011-9572-7. PMC 3115050. PMID 21461943.
- ↑ Romero-Corral, A. Somers, V. Lopez-Jimenez, F. Korenfeld, Y. Palin, S. Boelaert, K. Boarin, S. Sierra-Johnson, J. Rahim, A. (2008) 3-D Body Scanner, Body Volume Index: A Novel, Reproducible and Automated Anthropometric Tool Associated with Cardiometabolic Biomarkers Obesity A Research Journal 16 (1) 266-P
- ↑ Ghoshal K, Bhattacharyya M (February 2015). "Adiponectin: Probe of the molecular paradigm associating diabetes and obesity". World Journal of Diabetes. 6 (1): 151–66. doi:10.4239/wjd.v6.i1.151. PMC 4317307. PMID 25685286.
- ↑ Darabi H, Raeisi A, Kalantarhormozi MR, Ostovar A, Assadi M, Asadipooya K, et al. (August 2015). "Adiponectin as a Protective Factor Against the Progression Toward Type 2 Diabetes Mellitus in Postmenopausal Women". Medicine. 94 (33): e1347. doi:10.1097/md.0000000000001347. PMC 4616451. PMID 26287420.
- ↑ Duman BS, Turkoglu C, Gunay D, Cagatay P, Demiroglu C, Buyukdevrim AS (2003). "The interrelationship between insulin secretion and action in type 2 diabetes mellitus with different degrees of obesity: evidence supporting central obesity". Diabetes Butr Metab. 16 (4): 243–250.
- ↑ Gabriely I, Ma XH, Yang XM, Atzmon G, Rajala MW, Berg AH, et al. (October 2002). "Removal of visceral fat prevents insulin resistance and glucose intolerance of aging: an adipokine-mediated process?". Diabetes. 51 (10): 2951–8. doi:10.2337/diabetes.51.10.2951. PMID 12351432.
- 1 2 Asensio C, Cettour-Rose P, Theander-Carrillo C, Rohner-Jeanrenaud F, Muzzin P (May 2004). "Changes in glycemia by leptin administration or high- fat feeding in rodent models of obesity/type 2 diabetes suggest a link between resistin expression and control of glucose homeostasis". Endocrinology. 145 (5): 2206–13. doi:10.1210/en.2003-1679. PMID 14962997.
- ↑ Degawa-Yamauchi M, Bovenkerk JE, Juliar BE, Watson W, Kerr K, Jones R, et al. (November 2003). "Serum resistin (FIZZ3) protein is increased in obese humans". The Journal of Clinical Endocrinology and Metabolism. 88 (11): 5452–5. doi:10.1210/jc.2002-021808. PMID 14602788.
- ↑ Lee JH, Bullen JW, Stoyneva VL, Mantzoros CS (March 2005). "Circulating resistin in lean, obese, and insulin-resistant mouse models: lack of association with insulinemia and glycemia". American Journal of Physiology. Endocrinology and Metabolism. 288 (3): E625-32. doi:10.1152/ajpendo.00184.2004. PMID 15522996.
- ↑ Vendrell J, Broch M, Vilarrasa N, Molina A, Gómez JM, Gutiérrez C, et al. (June 2004). "Resistin, adiponectin, ghrelin, leptin, and proinflammatory cytokines: relationships in obesity". Obesity Research. 12 (6): 962–71. doi:10.1038/oby.2004.118. PMID 15229336.
- ↑ Hirosumi J, Tuncman G, Chang L, Görgün CZ, Uysal KT, Maeda K, et al. (November 2002). "A central role for JNK in obesity and insulin resistance". Nature. 420 (6913): 333–6. Bibcode:2002Natur.420..333H. doi:10.1038/nature01137. PMID 12447443. S2CID 1659156.
- ↑ Rajala MW, Qi Y, Patel HR, Takahashi N, Banerjee R, Pajvani UB, et al. (July 2004). "Regulation of resistin expression and circulating levels in obesity, diabetes, and fasting". Diabetes. 53 (7): 1671–9. doi:10.2337/diabetes.53.7.1671. PMID 15220189.
- ↑ Silha JV, Krsek M, Skrha JV, Sucharda P, Nyomba BL, Murphy LJ (October 2003). "Plasma resistin, adiponectin and leptin levels in lean and obese subjects: correlations with insulin resistance". European Journal of Endocrinology. 149 (4): 331–5. doi:10.1530/eje.0.1490331. PMID 14514348.
- ↑ Smith SR, Bai F, Charbonneau C, Janderová L, Argyropoulos G (July 2003). "A promoter genotype and oxidative stress potentially link resistin to human insulin resistance". Diabetes. 52 (7): 1611–8. doi:10.2337/diabetes.52.7.1611. PMID 12829623.
- ↑ Fujinami A, Obayashi H, Ohta K, Ichimura T, Nishimura M, Matsui H, et al. (January 2004). "Enzyme-linked immunosorbent assay for circulating human resistin: resistin concentrations in normal subjects and patients with type 2 diabetes". Clinica Chimica Acta; International Journal of Clinical Chemistry. 339 (1–2): 57–63. doi:10.1016/j.cccn.2003.09.009. PMID 14687894.
- ↑ McTernan PG, Fisher FM, Valsamakis G, Chetty R, Harte A, McTernan CL, et al. (December 2003). "Resistin and type 2 diabetes: regulation of resistin expression by insulin and rosiglitazone and the effects of recombinant resistin on lipid and glucose metabolism in human differentiated adipocytes". The Journal of Clinical Endocrinology and Metabolism. 88 (12): 6098–106. doi:10.1210/jc.2003-030898. PMID 14671216.
- ↑ Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, et al. (January 2001). "The hormone resistin links obesity to diabetes". Nature. 409 (6818): 307–12. Bibcode:2001Natur.409..307S. doi:10.1038/35053000. PMID 11201732. S2CID 4358808.
- ↑ LiPuma JJ, Spilker T, Coenye T, Gonzalez CF (June 2002). "An epidemic Burkholderia cepacia complex strain identified in soil". Lancet. 359 (9322): 2002–3. doi:10.1016/S0140-6736(02)08836-0. PMID 12076559. S2CID 8649208.
- ↑ McTernan PG, McTernan CL, Chetty R, Jenner K, Fisher FM, Lauer MN, et al. (May 2002). "Increased resistin gene and protein expression in human abdominal adipose tissue". The Journal of Clinical Endocrinology and Metabolism. 87 (5): 2407. doi:10.1210/jc.87.5.2407. PMID 11994397.
- ↑ Valsamakis G, McTernan PG, Chetty R, Al Daghri N, Field A, Hanif W, et al. (April 2004). "Modest weight loss and reduction in waist circumference after medical treatment are associated with favorable changes in serum adipocytokines". Metabolism. 53 (4): 430–4. doi:10.1016/j.metabol.2003.11.022. PMID 15045687.
- ↑ Mohanan S, Tapp H, McWilliams A, Dulin M (November 2014). "Obesity and asthma: pathophysiology and implications for diagnosis and management in primary care". Experimental Biology and Medicine. 239 (11): 1531–40. doi:10.1177/1535370214525302. PMC 4230977. PMID 24719380.
- ↑ Shore SA, Johnston RA (April 2006). "Obesity and asthma". Pharmacology & Therapeutics. 110 (1): 83–102. doi:10.1016/j.pharmthera.2005.10.002. PMID 16297979.
- ↑ Thomson CC, Clark S, Camargo CA (September 2003). "Body mass index and asthma severity among adults presenting to the emergency department". Chest. 124 (3): 795–802. doi:10.1378/chest.124.3.795. PMID 12970000. S2CID 13138899.
- ↑ Debette S, Beiser A, Hoffmann U, Decarli C, O'Donnell CJ, Massaro JM, et al. (August 2010). "Visceral fat is associated with lower brain volume in healthy middle-aged adults". Annals of Neurology. 68 (2): 136–44. doi:10.1002/ana.22062. PMC 2933649. PMID 20695006.
- ↑ "'Beer belly' link to Alzheimer's". BBC News. 2010-05-20.
- ↑ Mitchell S (2008-03-26). "Bulging belly now could mean dementia later". NBC News. Retrieved 2013-01-05.
- 1 2 Bujalska IJ, Kumar S, Stewart PM (April 1997). "Does central obesity reflect "Cushing's disease of the omentum"?". Lancet. 349 (9060): 1210–3. doi:10.1016/S0140-6736(96)11222-8. PMID 9130942. S2CID 24643796.
- 1 2 Ghroubi S, Elleuch H, Guermazi M, Kaffel N, Feki H, Abid M, et al. (November 2007). "[Abdominal obesity and knee ostheoarthritis]". Annales de Réadaptation et de Médecine Physique. 50 (8): 661–6. doi:10.1016/j.annrmp.2007.03.005. PMID 17445932.
- ↑ Stanhope KL, Havel PJ (March 2010). "Fructose consumption: recent results and their potential implications". Annals of the New York Academy of Sciences. 1190 (1): 15–24. Bibcode:2010NYASA1190...15S. doi:10.1111/j.1749-6632.2009.05266.x. PMC 3075927. PMID 20388133.
- ↑ Elliott SS, Keim NL, Stern JS, Teff K, Havel PJ (November 2002). "Fructose, weight gain, and the insulin resistance syndrome". The American Journal of Clinical Nutrition. 76 (5): 911–22. doi:10.1093/ajcn/76.5.911. PMID 12399260.
- ↑ Perez-Pozo SE, Schold J, Nakagawa T, Sánchez-Lozada LG, Johnson RJ, Lillo JL (March 2010). "Excessive fructose intake induces the features of metabolic syndrome in healthy adult men: role of uric acid in the hypertensive response". International Journal of Obesity. 34 (3): 454–61. doi:10.1038/ijo.2009.259. PMID 20029377. S2CID 4344197.
- ↑ Choi ME (March 2009). "The not-so-sweet side of fructose". Journal of the American Society of Nephrology. 3. 20 (3): 457–9. doi:10.1681/asn.2009010104. PMID 19244571.
- ↑ "Fructose sugar makes maturing human fat cells fatter, less insulin-sensitive, study finds". ScienceDaily. Retrieved 2021-03-08.
- ↑ Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, Rimm E (October 2003). "Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men". The American Journal of Clinical Nutrition. 78 (4): 719–27. doi:10.1093/ajcn/78.4.719. PMID 14522729.
- ↑ Bendsen NT, Chabanova E, Thomsen HS, Larsen TM, Newman JW, Stender S, et al. (January 2011). "Effect of trans fatty acid intake on abdominal and liver fat deposition and blood lipids: a randomized trial in overweight postmenopausal women". Nutrition & Diabetes. 1 (1): e4. doi:10.1038/nutd.2010.4. PMC 3302130. PMID 23154296.
- ↑ Micha R, Mozaffarian D (1 September 2008). "Trans fatty acids: effects on cardiometabolic health and implications for policy". Prostaglandins, Leukotrienes, and Essential Fatty Acids. 79 (3–5): 147–52. doi:10.1016/j.plefa.2008.09.008. PMC 2639783. PMID 18996687.
- ↑ Kavanagh K, Jones KL, Sawyer J, Kelley K, Carr JJ, Wagner JD, Rudel LL (July 2007). "Trans fat diet induces abdominal obesity and changes in insulin sensitivity in monkeys". Obesity. 15 (7): 1675–84. doi:10.1038/oby.2007.200. PMID 17636085. S2CID 4835948.
- ↑ Vergnaud AC, Norat T, Romaguera D, Mouw T, May AM, Travier N, et al. (August 2010). "Meat consumption and prospective weight change in participants of the EPIC-PANACEA study". The American Journal of Clinical Nutrition. 92 (2): 398–407. doi:10.3945/ajcn.2009.28713. PMID 20592131.
- ↑ Vergnaud AC, Norat T, Romaguera D, Peeters PH (2010-11-01). "Reply to A Astrup et al". The American Journal of Clinical Nutrition. 92 (5): 1275–1276. doi:10.3945/ajcn.110.000786. ISSN 0002-9165.
- ↑ Hosseini-Esfahani F, Mirmiran P, Koochakpoor G, Daneshpour MS, Guity K, Azizi F (May 2017). "Some dietary factors can modulate the effect of the zinc transporters 8 polymorphism on the risk of metabolic syndrome". Scientific Reports. 7 (1): 1649. Bibcode:2017NatSR...7.1649H. doi:10.1038/s41598-017-01762-9. PMC 5431973. PMID 28490771.
- ↑ Noreen EE, Sass MJ, Crowe ML, Pabon VA, Brandauer J, Averill LK (October 2010). "Effects of supplemental fish oil on resting metabolic rate, body composition, and salivary cortisol in healthy adults". Journal of the International Society of Sports Nutrition. 7: 31. doi:10.1186/1550-2783-7-31. PMC 2958879. PMID 20932294.
- ↑ Sites CK, Cooper BC, Toth MJ, Gastaldelli A, Arabshahi A, Barnes S (December 2007). "Effect of a daily supplement of soy protein on body composition and insulin secretion in postmenopausal women". Fertility and Sterility. 88 (6): 1609–17. doi:10.1016/j.fertnstert.2007.01.061. PMC 2200634. PMID 17412329.
- ↑ Bakhtiari A, Yassin Z, Hanachi P, Rahmat A, Ahmad Z, Sajadi P, Shojaei S (2012-04-30). "Effects of Soy on Body Composition: A 12-Week Randomized Controlled Trial among Iranian Elderly Women with Metabolic Syndrome". Iranian Journal of Public Health. 41 (4): 9–18. PMC 3481610. PMID 23113160.
- ↑ Monteiro, Carlos Augusto; Cannon, Geoffrey; Moubarac, Jean-Claude; Levy, Renata Bertazzi; Louzada, Maria Laura C.; Jaime, Patrícia Constante (January 2018). "The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing". Public Health Nutrition. 21 (1): 5–17. doi:10.1017/S1368980017000234. ISSN 1368-9800. PMID 28322183.
- ↑ "Processed foods highly correlated with obesity epidemic in the US". ScienceDaily. Retrieved 2021-03-08.
- ↑ Nardocci, Milena; Leclerc, Bernard-Simon; Louzada, Maria-Laura; Monteiro, Carlos Augusto; Batal, Malek; Moubarac, Jean-Claude (20 September 2018). "Consumption of ultra-processed foods and obesity in Canada". Canadian Journal of Public Health. 110 (1): 4–14. doi:10.17269/s41997-018-0130-x. ISSN 0008-4263. PMC 6964616. PMID 30238324.
- ↑ Organization, Pan American Health (17 June 2019). Ultra-processed food and drink products in Latin America: Sales, sources, nutrient profiles, and policy implications. ISBN 978-92-75-12032-3. Retrieved 15 March 2021.
- ↑ Rauber F, Steele EM, Louzada ML, Millett C, Monteiro CA, Levy RB (2020-05-01). "Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008-2016)". PLOS ONE. 15 (5): e0232676. Bibcode:2020PLoSO..1532676R. doi:10.1371/journal.pone.0232676. PMC 7194406. PMID 32357191.
- ↑ Machado PP, Steele EM, Levy RB, da Costa Louzada ML, Rangan A, Woods J, et al. (December 2020). "Ultra-processed food consumption and obesity in the Australian adult population". Nutrition & Diabetes. 10 (1): 39. doi:10.1038/s41387-020-00141-0. PMC 7719194. PMID 33279939.
- ↑ Beslay M, Srour B, Méjean C, Allès B, Fiolet T, Debras C, et al. (August 2020). "Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort". PLOS Medicine. 17 (8): e1003256. doi:10.1371/journal.pmed.1003256. PMC 7451582. PMID 32853224.
- ↑ Sandoval-Insausti H, Jiménez-Onsurbe M, Donat-Vargas C, Rey-García J, Banegas JR, Rodríguez-Artalejo F, Guallar-Castillón P (August 2020). "Ultra-Processed Food Consumption Is Associated with Abdominal Obesity: A Prospective Cohort Study in Older Adults". Nutrients. 12 (8): 2368. doi:10.3390/nu12082368. PMC 7468731. PMID 32784758.
- ↑ Sung, Hyuni; Park, Ji Min; Oh, Se Uk; Ha, Kyungho; Joung, Hyojee (February 2021). "Consumption of Ultra-Processed Foods Increases the Likelihood of Having Obesity in Korean Women". Nutrients. 13 (2): 698. doi:10.3390/nu13020698. PMC 7926298. PMID 33671557.
- ↑ Li, Ming; Shi, Zumin (August 2021). "Ultra-Processed Food Consumption Associated with Overweight/Obesity among Chinese Adults—Results from China Health and Nutrition Survey 1997–2011". Nutrients. 13 (8): 2796. doi:10.3390/nu13082796. PMC 8399660. PMID 34444957.
- ↑ Reardon, Thomas; Tschirley, David; Liverpool-Tasie, Lenis Saweda O.; Awokuse, Titus; Fanzo, Jessica; Minten, Bart; Vos, Rob; Dolislager, Michael; Sauer, Christine; Dhar, Rahul; Vargas, Carolina (2021-03-01). "The processed food revolution in African food systems and the double burden of malnutrition". Global Food Security. 28: 100466. doi:10.1016/j.gfs.2020.100466. ISSN 2211-9124. PMC 8049356. PMID 33868911.
- ↑ Ibrahim IA, Abd El-Aziz MF, Ahmed AF, Mohamed MA (2011). "Is the effect of high fat diet on lipid and carbohydrate metabolism related to inflammation?". Mediterranean Journal of Nutrition and Metabolism. 4 (3): 203–209. doi:10.1007/s12349-011-0056-9. S2CID 83758966.
- ↑ Cuthbertson D, Smith K, Babraj J, Leese G, Waddell T, Atherton P, et al. (March 2005). "Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle". FASEB Journal. 19 (3): 422–4. doi:10.1096/fj.04-2640fje. PMID 15596483. S2CID 22609751.
- ↑ Loenneke JP, Wilson JM, Manninen AH, Wray ME, Barnes JT, Pujol TJ (January 2012). "Quality protein intake is inversely related with abdominal fat". Nutrition & Metabolism. 9 (1): 5. doi:10.1186/1743-7075-9-5. PMC 3284412. PMID 22284338.
- ↑ President and fellows of Harvard College. (2006). Abnormal obesity and your health. Retrieved from http://www.health.harvard.edu/fhg/updates/abdominal-obesity-and-your-health.shtml Archived 2013-03-15 at the Wayback Machine
- ↑ Schröder H, Morales-Molina JA, Bermejo S, Barral D, Mándoli ES, Grau M, et al. (October 2007). "Relationship of abdominal obesity with alcohol consumption at population scale" (PDF). European Journal of Nutrition. 46 (7): 369–76. doi:10.1007/s00394-007-0674-7. PMID 17885722. S2CID 7185367.
- ↑ Bendsen NT, Christensen R, Bartels EM, Kok FJ, Sierksma A, Raben A, Astrup A (February 2013). "Is beer consumption related to measures of abdominal and general obesity? A systematic review and meta-analysis". Nutrition Reviews. 71 (2): 67–87. doi:10.1111/j.1753-4887.2012.00548.x. PMID 23356635.
- ↑ Heindel J (2011). "The Obesogen Hypothesis of Obesity: Overview and Human Evidence". Obesity Before Birth. Endocrine Updates. 4. Vol. 30. Springer. pp. 355–365. doi:10.1007/978-1-4419-7034-3_17. ISBN 978-1-4419-7033-6.
- ↑ Carey D.G.P. (1998). Abdominal Obesity. Current Opinion in Lipidology. (pp. 35-40). Vol. 9, No 1. Retrieved on April 9, 2012.
- ↑ Després J (2006). "Abdominal obesity: the most prevalent cause of the metabolic syndrome and related cardiometabolic risk". European Heart Journal. 8 (Supplements): B4–B12. doi:10.1093/eurheartj/sul002.
- ↑ Abdominal obesity and your health. (2006). Retrieved from http://www.health.harvard.edu/fhg/updates/abdominal-obesity-and-your-health.shtml Archived 2013-03-15 at the Wayback Machine
- 1 2 National Cholesterol Education Program (2002). Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III Final Report). National Institutes of Health. p. II–17. Archived from the original on 2005-05-24. Retrieved 2011-05-14.
- ↑ Iribarren C, Darbinian JA, Lo JC, Fireman BH, Go AS (December 2006). "Value of the sagittal abdominal diameter in coronary heart disease risk assessment: cohort study in a large, multiethnic population". American Journal of Epidemiology. 164 (12): 1150–9. doi:10.1093/aje/kwj341. PMID 17041127.
- ↑ U.S. Preventive Services Task Force Evidence Syntheses (2000). HSTAT: Guide to Clinical Preventive Services, 3rd Edition: Recommendations and Systematic Evidence Reviews, Guide to Community Preventive Services. Archived from the original on 2009-07-04. Retrieved 2017-08-29.
- ↑ "Abdominal obesity and your health". Health.harvard.edu. Archived from the original on 2013-03-15. Retrieved 2013-01-05.
- ↑ Smith SC, Haslam D (January 2007). "Abdominal obesity, waist circumference and cardio-metabolic risk: awareness among primary care physicians, the general population and patients at risk--the Shape of the Nations survey". Current Medical Research and Opinion. 23 (1): 29–47. doi:10.1185/030079906X159489. PMID 17261236. S2CID 11796524.
- ↑ Knowles KM, Paiva LL, Sanchez SE, Revilla L, Lopez T, Yasuda MB, et al. (January 2011). "Waist Circumference, Body Mass Index, and Other Measures of Adiposity in Predicting Cardiovascular Disease Risk Factors among Peruvian Adults". International Journal of Hypertension. 2011: 931402. doi:10.4061/2011/931402. PMC 3034939. PMID 21331161.
- ↑ Méthot J, Houle J, Poirier P (May 2010). "Obesity: how to define central adiposity?". Expert Review of Cardiovascular Therapy. 8 (5): 639–44. doi:10.1586/erc.10.38. PMID 20450297. S2CID 31913449.
- 1 2 3 Parikh RM, Joshi SR, Pandia K (December 2009). "Index of central obesity is better than waist circumference in defining metabolic syndrome". Metabolic Syndrome and Related Disorders. 7 (6): 525–7. doi:10.1089/met.2008.0102. PMID 19558273.
- ↑ National Cholesterol Education Program (2002). Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III Final Report). National Institutes of Health. p. II–27. Archived from the original on 2005-05-24. Retrieved 2011-05-14.
- ↑ Misra A, Wasir JS, Vikram NK, Pandey RM, Kumar P (June 2010). "Cutoffs of abdominal adipose tissue compartments as measured by magnetic resonance imaging for detection of cardiovascular risk factors in apparently healthy adult Asian Indians in North India". Metabolic Syndrome and Related Disorders. 8 (3): 243–7. doi:10.1089/met.2009.0046. PMID 20156066.
- ↑ Boston, 677 Huntington Avenue; Ma 02115 +1495‑1000 (2012-10-21). "Abdominal Obesity Measurement Guidelines for Different Ethnic Groups". Obesity Prevention Source. Retrieved 2021-03-31.
- ↑ Alberti KG, Zimmet P, Shaw J (2005). "The metabolic syndrome--a new worldwide definition". Lancet. 366 (9491): 1059–62. doi:10.1016/S0140-6736(05)67402-8. PMID 16182882. S2CID 30586927.
- ↑ Boston, 677 Huntington Avenue; Ma 02115 +1495‑1000 (2012-10-21). "Measuring Obesity". Obesity Prevention Source. Retrieved 2021-03-31.
- ↑ Joshi PP (March 2008). "Is waist to height ratio a better and more practical measure of obesity to assess cardiovascular or diabetes risk in indians?". The Journal of the Association of Physicians of India. 56: 202–3, author reply 203–4. PMID 18700281. Archived from the original on 2017-10-11. Retrieved 2011-06-04.
- ↑ Veigas NM, Dharmalingam, Marcus SR (2011). "Oxidative Stress in Obesity and Metabolic Syndrome in Asian Indians". Journal of Medical Biochemistry. 30 (2): 115–20. doi:10.2478/v10011-011-0006-6.
- ↑ Gupta R, Rastogi P, Sarna M, Gupta VP, Sharma SK, Kothari K (September 2007). "Body-mass index, waist-size, waist-hip ratio and cardiovascular risk factors in urban subejcts". The Journal of the Association of Physicians of India. 55: 621–7. PMID 18051732. Archived from the original on 2017-10-12. Retrieved 2011-06-04.
- ↑ [Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring) 2007;15 (1) 216- 224]
- ↑ Lemieux S, Prud'homme D, Bouchard C, Tremblay A, Després JP (October 1993). "Sex differences in the relation of visceral adipose tissue accumulation to total body fatness". The American Journal of Clinical Nutrition. 58 (4): 463–7. doi:10.1093/ajcn/58.4.463. PMID 8379501.
- ↑ Carey DG, Campbell LV, Chisholm DJ (1996). "Is visceral fat (intra-abdominal and hepatic) a major determinant of gender differences in insulin resistance and dyslipidaemia?". Diabetes. 45: 110A.
- ↑ Wingard DL (May 1990). "Sex differences and coronary heart disease. A case of comparing apples and pears?". Circulation. 81 (5): 1710–2. doi:10.1161/01.cir.81.5.1710. PMID 2331775.
- ↑ Andersen BL, Legrand J (1991). "Body Image for Women: Conceptualization, Assessment, and a Test of its Importance to Sexual Dysfunction and Medical Illness". Journal of Sex Research. 28 (3): 457–477. doi:10.1080/00224499109551619. PMC 3065017. PMID 21451731.
- ↑ Archived October 24, 2007, at the Wayback Machine
- ↑ "Abdominal fat and what to do about it. Visceral fat more of a health concern than subcutaneous fat". Harvard Health Publications. Health.harvard.edu. Archived from the original on 2011-09-28. Retrieved 2013-01-05.
- ↑ Elbers JM, Asscheman H, Seidell JC, Gooren LJ (February 1999). "Effects of sex steroid hormones on regional fat depots as assessed by magnetic resonance imaging in transsexuals". The American Journal of Physiology. 276 (2): E317-25. doi:10.1152/ajpendo.1999.276.2.E317. PMID 9950792.
- ↑ Seidell JC, Björntorp P, Sjöström L, Kvist H, Sannerstedt R (September 1990). "Visceral fat accumulation in men is positively associated with insulin, glucose, and C-peptide levels, but negatively with testosterone levels". Metabolism. 39 (9): 897–901. doi:10.1016/0026-0495(90)90297-p. PMID 2202881.
- ↑ Tchernof A, Després JP, Bélanger A, Dupont A, Prud'homme D, Moorjani S, et al. (April 1995). "Reduced testosterone and adrenal C19 steroid levels in obese men". Metabolism. 44 (4): 513–9. doi:10.1016/0026-0495(95)90060-8. PMID 7723675.
- ↑ Barrett-Connor E (January 1997). "Sex differences in coronary heart disease. Why are women so superior? The 1995 Ancel Keys Lecture". Circulation. 95 (1): 252–64. doi:10.1161/01.cir.95.1.252. PMID 8994444.
- ↑ "Even a Little Exercise Fights Obesity". Webmd.com. 2009-11-06. Retrieved 2013-01-05.
- ↑ "Weight Management". Washington.edu. 2012-11-26. Archived from the original on February 9, 2013. Retrieved 2013-01-05.
- ↑ Rockoff JD, Dooren JC (October 8, 2010). "Abbott Pulls Diet Drug Meridia Off US Shelves". The Wall Street Journal. Archived from the original on 11 October 2010. Retrieved 8 October 2010.
- ↑ "Top obesity drug sibutramine being suspended". BBC News. 2010-01-22. Archived from the original on 25 January 2010. Retrieved 2010-01-22.
- ↑ (in German) Sibutramin-Vertrieb in der Europäischen Union ausgesetzt Archived 2012-07-19 at archive.today. Abbott Laboratories in Germany. Press release 2010-01-21. Retrieved 2010-01-27
- ↑ "Sibutramine (brand name Reductil) Information - Australia". Abbott Laboratories. 2010. Archived from the original on 14 October 2010. Retrieved 2010-10-08.
- ↑ "Health Canada Endorsed Important Safety Information on MERIDIA (Sibutramine Hydrochloride Monohydrate): Subject: Voluntary withdrawal of Meridia (sibutramine) capsules from the Canadian market". Hc-sc.gc.ca. 2010-10-14. Retrieved 2013-01-05.
- ↑ "De-registration of pharmaceutical products containing sibutramine" (Press release). info.gov in Hong Kong. November 2, 2010. Retrieved 2010-11-08.
- ↑ "Thai FDA reveals voluntary withdrawal of sibutramine from the Thai market" (PDF) (Press release). Food and Drug Administration of Thailand. October 20, 2010. Archived from the original (PDF) on May 11, 2011. Retrieved 2010-12-22.
- ↑ Arciero PJ, Gentile CL, Martin-Pressman R, Ormsbee MJ, Everett M, Zwicky L, Steele CA (August 2006). "Increased dietary protein and combined high intensity aerobic and resistance exercise improves body fat distribution and cardiovascular risk factors". International Journal of Sport Nutrition and Exercise Metabolism. 16 (4): 373–92. CiteSeerX 10.1.1.517.3533. doi:10.1123/ijsnem.16.4.373. PMID 17136940.
- ↑ Kelley GA, Kelley KS, Roberts S, Haskell W (2012). "Combined effects of aerobic exercise and diet on lipids and lipoproteins in overweight and obese adults: a meta-analysis". Journal of Obesity. 2012: 985902. doi:10.1155/2012/985902. PMC 3317197. PMID 22523670.
- ↑ Fonseca V (December 2003). "Effect of thiazolidinediones on body weight in patients with diabetes mellitus". The American Journal of Medicine. 115 Suppl 8A (8): 42S–48S. doi:10.1016/j.amjmed.2003.09.005. PMID 14678865.
- ↑ 23/09/2010 European Medicines Agency recommends suspension of Avandia, Avandamet and Avaglim http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2010/09/news_detail_001119.jsp&mid=WC0b01ac058004d5c1
- 1 2 Bacon L, Aphramor L (January 2011). "Weight science: evaluating the evidence for a paradigm shift". Nutrition Journal. 10 (9): 9. doi:10.1186/1475-2891-10-9. PMC 3041737. PMID 21261939.
- ↑ Howard BV, Manson JE, Stefanick ML, Beresford SA, Frank G, Jones B, et al. (January 2006). "Low-fat dietary pattern and weight change over 7 years: the Women's Health Initiative Dietary Modification Trial". JAMA. 295 (1): 39–49. doi:10.1001/jama.295.1.39. PMID 16391215.
- ↑ Jensen M (2007-01-19). "Belly fat in men: What you need to know". Mayoclinic.com. Archived from the original on 23 March 2008. Retrieved 2008-04-07.
Sit-ups will make your abdominal muscles stronger, sure. And, you may look thinner by building your abdominal muscles because you can hold in your belly fat better. But strengthening your stomach muscles alone will not specifically reduce belly fat.
- ↑
- "spare tire". Merriam-Webster. Retrieved August 2, 2021.
- "paunch". Merriam-Webster. Retrieved August 2, 2021.
- "potbelly". Merriam-Webster. Retrieved August 2, 2021.
- ↑ Bobak M, Skodova Z, Marmot M (October 2003). "Beer and obesity: a cross-sectional study". European Journal of Clinical Nutrition. 57 (10): 1250–3. doi:10.1038/sj.ejcn.1601678. PMID 14506485.
- ↑ Staff writer (2003-10-12). "Why the beer belly may be a myth". BBC News.
- ↑ Economic costs of abdominal obesity; Højgaard, Betina and Olsen, Kim Rose and Søgaard, Jes and Sørensen, Thorkild I A and Gyrd-Hansen, Dorte; Obesity facts, ISSN 1662-4025, 2008, Volume 1, Issue 3, pp. 146–154.
Further reading
| Wikimedia Commons has media related to Abdominal obesity. |
- Griesemer RL (July 25, 2008). "Index of Central Obesity as a Parameter to Evaluate Metabolic Syndrome for White, Black, and Hispanic Adults in the United States" (Master's thesis). Public Health Theses. Georgia State University.
- Lee K, Song YM, Sung J (April 2008). "Which obesity indicators are better predictors of metabolic risk?: healthy twin study". Obesity. 16 (4): 834–40. doi:10.1038/oby.2007.109. PMID 18239595. S2CID 1633972.
- Shao J, Yu L, Shen X, Li D, Wang K (November 2010). "Waist-to-height ratio, an optimal predictor for obesity and metabolic syndrome in Chinese adults". The Journal of Nutrition, Health & Aging. 14 (9): 782–5. doi:10.1007/s12603-010-0106-x. PMID 21085910. S2CID 11187741.