Deferiprone
 | |
| Names | |
|---|---|
| Trade names | Ferriprox |
IUPAC name
| |
| Clinical data | |
| Drug class | Iron chelator[1] |
| Main uses | Iron overload in thalassaemia major[1][2] |
| Side effects | Red-brown urine, nausea, abdominal pain, vomiting[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category | |
| Routes of use | By mouth |
| Typical dose | 25 mg/kg TID[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a612016 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Metabolism | Glucuronidation |
| Elimination half-life | 2 to 3 hours |
| Excretion | Kidney (75 to 90% in 24 hours) |
| Chemical and physical data | |
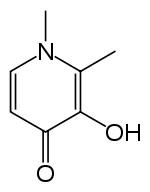
| Formula | C7H9NO2 |
| Molar mass | 139.154 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Deferiprone, sold under the brand name Ferriprox among others, is a medication used to treat iron overload due to blood transfusions in thalassaemia major.[1][2] It is taken by mouth.[5] Evidence supports improved blood markers but not symptoms or survival.[2]
Common side effects include red-brown urine, nausea, abdominal pain, and vomiting.[1] Other side effects may include low white blood cells, infection, and prolonged QT.[1][2] Use in pregnancy may harm the baby.[2] It is an iron chelator.[1]
Deferiprone became commercially available in 1994.[6] It was initially approved in Europe and Asia.[7] It is on the World Health Organization's List of Essential Medicines as an alternative to deferasirox.[8] It is available as a generic medication.[5] This was followed by approval in the United States in 2011.[2] In the United Kingdom 100 tablets of 500 mg costs the NHS about £130.[5] In the United States this amount costs about 7,500 USD.[9]
Medical uses
Deferiprone is indicated in the European Union for the treatment of iron overload in those with thalassaemia major when current chelation therapy is contraindicated or inadequate.[1]
Deferiprone in combination with another chelator is indicated in the European Union in those with thalassaemia major when monotherapy with any iron chelator is ineffective, or when prevention or treatment of life-threatening consequences of iron overload (mainly cardiac overload) justifies rapid or intensive correction.[1]
Dosage
It is generally used at a dose of 25 mg/kg body weight three times a day.[1] The maximum dose is 100 mg/kg per day.[5]
History
Deferiprone was approved for medical use in the European Union in August 1999.[1]
It was approved for medical use in the United States in October 2011.[10][11] Generic versions were approved in August 2019.[12]
The safety and effectiveness of deferiprone is based on an analysis of data from twelve clinical studies in 236 participants.[10] Participants in the study did not respond to prior iron chelation therapy.[10] Deferiprone was considered a successful treatment for participants who experienced at least a 20 percent decrease in serum ferritin, a protein that stores iron in the body for later use.[10] Half of the participants in the study experienced at least a 20 percent decrease in ferritin levels.[10]
Controversy
Deferiprone was at the center of a protracted struggle between Nancy Olivieri, a Canadian haematologist and researcher, and the Hospital for Sick Children and the pharmaceutical company Apotex, that started in 1996, and delayed approval of the drug in North America.[13] Olivieri's data suggested deferiprone leads to progressive hepatic fibrosis.[14][15][16]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Ferriprox EPAR". European Medicines Agency (EMA). Archived from the original on 14 August 2020. Retrieved 20 May 2020. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- 1 2 3 4 5 6 "Deferiprone Monograph for Professionals". Drugs.com. Archived from the original on 11 June 2021. Retrieved 21 December 2021.
- 1 2 "Deferiprone (Ferriprox) Use During Pregnancy". Drugs.com. 30 March 2020. Archived from the original on 26 October 2020. Retrieved 20 May 2020.
- ↑ "Ferriprox 100 mg/ml oral solution - Summary of Product Characteristics (SmPC)". (emc). 26 November 2019. Archived from the original on 7 August 2020. Retrieved 20 May 2020.
- 1 2 3 4 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 1075. ISBN 978-0857114105.
- ↑ Staff. "Cipla's History". Cipla. Archived from the original on 2015-10-27.
- ↑ Savulescu J (February 2004). "Thalassaemia major: the murky story of deferiprone". BMJ. 328 (7436): 358–9. doi:10.1136/bmj.328.7436.358. PMC 341373. PMID 14962851.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ↑ "Ferriprox Prices, Coupons and Patient Assistance Programs". Retrieved 22 December 2021.
- 1 2 3 4 5 "FDA Approves Ferripox (deferiprone) to Treat Patients with Excess Iron in the Body". U.S. Food and Drug Administration (FDA) (Press release). 14 October 2011. Archived from the original on 10 October 2016.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Drug Approval Package: Ferriprox (deferiprone) Tablet NDA #021825". U.S. Food and Drug Administration (FDA). 30 November 2011. Archived from the original on 29 November 2020. Retrieved 20 May 2020.
- ↑ "Deferiprone: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 19 October 2020. Retrieved 20 May 2020.
- ↑ Viens AM, Savulescu J (February 2004). "Introduction to The Olivieri symposium". Journal of Medical Ethics. 30 (1): 1–7. doi:10.1136/jme.2003.006577. PMC 1757126. PMID 14872065.
- ↑ Brittenham GM, Nathan DG, Olivieri NF, Porter JB, Pippard M, Vichinsky EP, Weatherall DJ (June 2003). "Deferiprone and hepatic fibrosis". Blood. 101 (12): 5089–90, author reply 5090–1. doi:10.1182/blood-2002-10-3173. PMID 12788794.
- ↑ Wanless IR, Sweeney G, Dhillon AP, Guido M, Piga A, Galanello R, et al. (September 2002). "Lack of progressive hepatic fibrosis during long-term therapy with deferiprone in subjects with transfusion-dependent beta-thalassemia". Blood. 100 (5): 1566–9. doi:10.1182/blood-2002-01-0306. PMID 12176871.
- ↑ Cribb R (2019-02-27). "UHN patients given unlicensed drug that led to diabetes, liver dysfunction and one death, study finds". The Star. Toronto. Archived from the original on 2019-02-27. Retrieved 2019-02-27.
External links
| External sites: |
|
|---|---|
| Identifiers: |