WHO Model List of Essential Medicines
The WHO Model List of Essential Medicines, also known as Essential Medicines List (EML),[1] published by the World Health Organization (WHO), contains the medications considered to be most effective and safe to meet the most important needs in a health system.[2] The list is frequently used by countries to help develop their own local lists of essential medicines.[2] As of 2016, more than 155 countries have created national lists of essential medicines based on the World Health Organization's model list.[1] This includes both developed and developing countries.[2][3]
The list is divided into core items and complementary items.[4] The core items are deemed to be the most cost-effective options for key health problems and are usable with little additional health care resources.[4] The complementary items either require additional infrastructure such as specially trained health care providers or diagnostic equipment or have a lower cost–benefit ratio.[4] About 25% of items are in the complementary list.[5] Some medications are listed as both core and complementary.[6] While most medications on the list are available as generic products, being under patent does not preclude inclusion.[7]
The first list was published in 1977 and included 208 medications.[8][2][9] The WHO updates the list every two years.[10] There are 306 medications in the 14th list in 2005,[11] 410 in the 19th list in 2015,[10] 433 in the 20th list in 2017,[12][13] 460 in the 21st list in 2019,[14][15][16] and 479 in the 22nd list in 2021.[17][18] Various national lists contain between 334 and 580 medications.[5][19] The 23rd list was updated in 2023 containing 1200 recommendations for 591 drugs and 103 therapeutic equivalents.[20]
A separate list for children up to 12 years of age, known as the WHO Model List of Essential Medicines for Children (EMLc), was created in 2007 and is in its 9th edition.[10][21][22][23] It was created to make sure that the needs of children were systematically considered such as availability of proper formulations.[24][25] Everything in the children's list is also included in the main list.[26] The list and notes are based on the 19th to 23rd edition of the main list.[4][12][14][17][27] An α indicates a medicine is on the complementary list.[4][14][17] Therapeutic alternatives with similar clinical performance are listed for some medicines and they may be considered for national essential medicines lists.[17][18] The 9th Essential Medicines List for Children was updated in July 2023.[23][28]
Anaesthetics, preoperative medicines and medical gases
General anaesthetics and oxygen
Inhalational medicines
Injectable medicines
Local anaesthetics
Complementary:
Preoperative medication and sedation for short-term procedures
Medical gases
Medicines for pain and palliative care
Non-opioids and non-steroidal anti-inflammatory medicines (NSAIMs)
- Acetylsalicylic acid (aspirin)
- Ibuprofen[note 3]
- Paracetamol[note 4] (acetaminophen)
Opioid analgesics
Complementary:
Medicines for other common symptoms in palliative care
Antiallergics and medicines used in anaphylaxis
Antidotes and other substances used in poisonings
Non-specific
Specific
- Acetylcysteine
- Atropine
- Calcium gluconate
- Methylthioninium chloride (methylene blue)
- Naloxone
- Penicillamine
- Prussian blue
- Sodium nitrite
- Sodium thiosulfate
Complementary:
Medicines for diseases of the nervous system
Antiseizure medicines
- Carbamazepine
- Diazepam
- Lamotrigine[note 12]
- Levetiracetam
- Lorazepam[note 13]
- Magnesium sulfate[note 14]
- Midazolam[note 15]
- Phenobarbital
- Phenytoin[note 16]
- Valproic acid (sodium valproate)[note 17]
Complementary:
- Ethosuximideα
- Levetiracetamα
- Valproic acid (sodium valproate)α[note 17]
Medicines for multiple sclerosis
Complementary:
Medicines for parkinsonism
Anti-infective medicines
Anthelminthics
Intestinal anthelminthics
Antifilarials
Antischistosomals and other antinematode medicines
Complementary:
Cysticidal medicines
Complementary:
Antibacterials
Access group antibiotics
- Amikacin
- Amoxicillin
- Amoxicillin/clavulanic acid (amoxicillin + clavulanic acid)
- Ampicillin
- Benzathine benzylpenicillin
- Benzylpenicillin
- Cefalexin
- Cefazolin[note 22]
- Chloramphenicol[note 23]
- Clindamycin
- Cloxacillin[note 24][note 25]
- Doxycycline[note 26]
- Gentamicin
- Metronidazole
- Nitrofurantoin
- Phenoxymethylpenicillin (penicillin V)
- Procaine benzylpenicillin[note 27]
- Spectinomycin
- Sulfamethoxazole/trimethoprim (sulfamethoxazole + trimethoprim)
- Trimethoprim
Watch group antibiotics
- Azithromycin
- Cefixime
- Cefotaxime[note 28]
- Ceftriaxone[note 29][note 30]
- Cefuroxime
- Ciprofloxacin
- Clarithromycin[note 31][note 32]
- Piperacillin/tazobactam (piperacillin + tazobactam)
- Vancomycin[note 33]
Complementary:
Reserve group antibiotics
Reserve antibiotics are last-resort antibiotics. The EML antibiotic book was published in 2022.[29][30][31]
Complementary:
Antileprosy medicines
Antituberculosis medicines
- Ethambutol
- Ethambutol/isoniazid/pyrazinamide/rifampicin (ethambutol + isoniazid + pyrazinamide + rifampicin)
- Ethambutol/isoniazid/rifampicin (ethambutol + isoniazid + rifampicin)
- Ethionamide
- Isoniazid
- Isoniazid/pyrazinamide/rifampicin (isoniazid + pyrazinamide + rifampicin)
- Isoniazid/rifampicin (isoniazid + rifampicin)
- Isoniazid/rifapentine (isoniazid + rifapentine)
- Moxifloxacin
- Pyrazinamide
- Rifabutin[note 36]
- Rifampicin
- Rifapentine
Complementary:
Antifungal medicines
- Amphotericin B
- Clotrimazole
- Fluconazole
- Flucytosine
- Griseofulvin
- Itraconazole[note 41]
- Nystatin
- Voriconazole[note 42]
Complementary:
Antiviral medicines
Antiherpes medicines
Antiretrovirals
Nucleoside/nucleotide reverse transcriptase inhibitors
Non-nucleoside reverse transcriptase inhibitors
Protease inhibitors
200mg.jpg.webp)
Integrase inhibitors
Fixed-dose combinations of antiretroviral medicines
- Abacavir/lamivudine (abacavir + lamivudine)
- Dolutegravir/lamivudine/tenofovir (dolutegravir + lamivudine + tenofovir)
- Efavirenz/emtricitabine/tenofovir[note 49]
- Efavirenz/lamivudine/tenofovir (efavirenz + lamivudine + tenofovir)
- Emtricitabine/tenofovir (emtricitabine + tenofovir)[note 49][note 50]
- Lamivudine/zidovudine (lamivudine + zidovudine)
Medicines for prevention of HIV-related opportunistic infections
Other antivirals
Complementary:
Antihepatitis medicines
Medicines for hepatitis B
Nucleoside/Nucleotide reverse transcriptase inhibitors
Medicines for hepatitis C
Pangenotypic direct-acting antiviral combinations
Non-pangenotypic direct-acting antiviral combinations
Other antivirals for hepatitis C
Antiprotozoal medicines
Antiamoebic and antigiardiasis medicines
Antileishmaniasis medicines
Antimalarial medicines
For curative treatment
- Amodiaquine[note 62]
- Artemether[note 63]
- Artemether/lumefantrine (artemether + lumefantrine)[note 64]
- Artesunate[note 65]
- Artesunate/amodiaquine (artesunate + amodiaquine)[note 66]
- Artesunate/mefloquine (artesunate + mefloquine)
- Artesunate/pyronaridine tetraphosphate (artesunate + pyronaridine tetraphosphate)[note 67]
- Chloroquine[note 68]
- Dihydroartemisinin/piperaquine phosphate (dihydroartemisinin + piperaquine phosphate)[note 69]
- Doxycycline[note 70]
- Mefloquine[note 62]
- Primaquine[note 71]
- Quinine[note 72]
- Sulfadoxine/pyrimethamine (sulfadoxine + pyrimethamine)[note 73]
For chemoprevention
Antipneumocystosis and antitoxoplasmosis medicines
Complementary:
Antitrypanosomal medicines
African trypanosomiasis
Medicines for the treatment of 1st stage African trypanosomiasis
Medicines for the treatment of 2nd stage African trypanosomiasis
Complementary:
American trypanosomiasis
Medicines for ectoparasitic infections
Medicines for Ebola virus disease
Medicines for COVID-19
No listings in this section.
Antimigraine medicines
For treatment of acute attack
- Acetylsalicylic acid (aspirin)
- Ibuprofen
- Paracetamol (acetaminophen)[note 83]
- Sumatriptan
For prophylaxis
Immunomodulators and antineoplastics
Immunomodulators for non-malignant disease
Complementary:
Antineoplastics and supportive medicines
Cytotoxic medicines
Complementary:
- Arsenic trioxideα
- Asparaginaseα[note 18]
- Bendamustineα
- Bleomycinα
- Calcium folinate (leucovorin calcium)α
- Capecitabineα
- Carboplatinα
- Chlorambucilα
- Cisplatinα
- Cyclophosphamideα
- Cytarabineα
- Dacarbazineα
- Dactinomycinα
- Daunorubicinα
- Docetaxelα
- Doxorubicinα
- Doxorubicin (as pegylated liposomal)α
- Etoposideα
- Fludarabineα
- Fluorouracilα
- Gemcitabineα
- Hydroxycarbamide (hydroxyurea)α
- Ifosfamideα
- Irinotecanα
- Melphalanα
- Mercaptopurineα
- Methotrexateα
- Oxaliplatinα
- Paclitaxelα
- Pegaspargaseα[note 18]
- Procarbazineα
- Realgar Indigo naturalis formulationα
- Tioguanineα
- Vinblastineα
- Vincristineα
- Vinorelbineα
Targeted therapies
Complementary:
Immunomodulators
Complementary:
Hormones and antihormones
Complementary:
Supportive medicines
Complementary:
Therapeutic foods
- Ready-to-use therapeutic food[note 92]
Medicines affecting the blood
Antianaemia medicines
- Ferrous salt
- Ferrous salt/folic acid (ferrous salt + folic acid)
- Folic acid[note 93]
- Hydroxocobalamin
Complementary:
Medicines affecting coagulation
- Dabigatran[note 95]
- Enoxaparin[note 96]
- Heparin sodium
- Phytomenadione
- Protamine sulfate
- Tranexamic acid
- Warfarin
Complementary:
Other medicines for haemoglobinopathies
Complementary:
- Deferoxamineα
- Hydroxycarbamide (hydroxyurea)α
Blood products of human origin and plasma substitutes
Blood and blood components

- Cryoprecipitate, pathogen-reduced[note 98]
- Fresh frozen plasma
- Platelets
- Red blood cells
- Whole blood
Plasma-derived medicines
Human immunoglobulins
- Rho(D) immune globulin (anti-D immunoglobulin)
- Anti-rabies immunoglobulin
- Anti-tetanus immunoglobulin
Complementary:
Blood coagulation factors
Complementary:
Plasma substitutes
Cardiovascular medicines
Antianginal medicines
Antiarrhythmic medicines
- Bisoprolol[note 101]
- Digoxin
- Epinephrine (adrenaline)
- Lidocaine
- Verapamil
Complementary:
Antihypertensive medicines
- Amlodipine[note 102]
- Bisoprolol[note 103]
- Enalapril[note 104]
- Hydralazine[note 105]
- Hydrochlorothiazide[note 106]
- Lisinopril/amlodipine (lisinopril + amlodipine)[note 107]
- Lisinopril/hydrochlorothiazide (lisinopril + hydrochlorothiazide)[note 108]
- Losartan[note 109]
- Methyldopa[note 110]
- Telmisartan/amlodipine (telmisartan + amlodipine)[note 111]
- Telmisartan/hydrochlorothiazide (telmisartan + hydrochlorothiazide)[note 112]
Complementary:
Medicines used in heart failure
- Bisoprolol[note 101]
- Digoxin
- Enalapril[note 113]
- Furosemide[note 114]
- Hydrochlorothiazide[note 106]
- Losartan[note 109]
- Spironolactone
Complementary:
Antithrombotic medicines
Anti-platelet medicines
- Acetylsalicylic acid (aspirin)
- Clopidogrel
Thrombolytic medicines
Complementary:
Lipid-lowering agents
Fixed-dose combinations for prevention of atherosclerotic cardiovascular disease
- Acetylsalicylic acid/atorvastatin/ramipril (acetylsalicylic acid + atorvastatin + ramipril)[note 116][note 117]
- Acetylsalicylic acid/simvastatin/ramipril/atenolol/hydrochlorothiazide (acetylsalicylic acid + simvastatin + ramipril + atenolol + hydrochlorothiazide)[note 118][note 117][note 119][note 120]
- Atorvastatin/perindopril/amlodipine (atorvastatin + perindopril + amlodipine)[note 116][note 121][note 122]
Dermatological medicines (topical)
Antifungal medicines
Anti-infective medicines
Anti-inflammatory and antipruritic medicines
Medicines affecting skin differentiation and proliferation
- Benzoyl peroxide
- Calcipotriol[note 126]
- Coal tar
- Fluorouracil
- Podophyllum resin[note 127]
- Salicylic acid
- Urea
Complementary:
Scabicides and pediculicides
Diagnostic agents
Ophthalmic medicines
Radiocontrast media
Complementary:
Antiseptics and disinfectants
Antiseptics
Disinfectants
Diuretics
Complementary:
Gastrointestinal medicines
Complementary:
Antiulcer medicines
Antiemetic medicines
Complementary:
Anti-inflammatory medicines
Complementary:
Laxatives
Medicines used in diarrhoea
- Oral rehydration salts + zinc sulfate (Co-packaged)
Oral rehydration
Medicines for diarrhoea
Medicines for endocrine disorders
Adrenal hormones and synthetic substitutes
Androgens
Complementary:
Estrogens
No listings in this section.
Progestogens
Medicines for diabetes
Insulins
Oral hypoglycaemic agents
Complementary:
Medicines for hypoglycaemia
Complementary:
Thyroid hormones and antithyroid medicines
Complementary:
Medicines for disorders of the pituitary hormone system
Complementary:
Immunologicals
Diagnostic agents
- Tuberculin, purified protein derivative (PPD)
Sera, immunoglobulins and monoclonal antibodies
- Anti-rabies virus monoclonal antibodies[note 18]
- Antivenom immunoglobulin[note 148]
- Diphtheria antitoxin
- Equine rabies immunoglobulin
Vaccines
Recommendations for all
- BCG vaccine
- Diphtheria vaccine
- Haemophilus influenzae type b vaccine
- Hepatitis B vaccine
- Human papilloma virus (HPV) vaccine
- Measles vaccine
- Pertussis vaccine
- Pneumococcal vaccine
- Poliomyelitis vaccine
- Rotavirus vaccine
- Rubella vaccine
- Tetanus vaccine
Recommendations for certain regions
- Japanese encephalitis vaccine[note 149]
- Tick-borne encephalitis vaccine[note 149]
- Yellow fever vaccine[note 149]
Recommendations for some high-risk populations
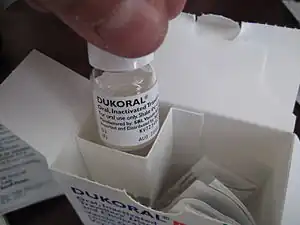
- Cholera vaccine[note 150]
- Dengue vaccine[note 150]
- Hepatitis A vaccine[note 150]
- Meningococcal meningitis vaccine[note 150]
- Rabies vaccine[note 150]
- Typhoid vaccine[note 150]
Recommendations for immunization programmes with certain characteristics
Muscle relaxants (peripherally-acting) and cholinesterase inhibitors
Complementary:
Ophthalmological preparations
Anti-infective agents
Anti-inflammatory agents
Local anesthetics
Miotics and antiglaucoma medicines
Mydriatics
Complementary:
- Epinephrine (adrenaline)α
Anti-vascular endothelial growth factor (VEGF) preparations
Complementary:
Medicines for reproductive health and perinatal care
Contraceptives
Oral hormonal contraceptives
Injectable hormonal contraceptives
Intrauterine devices
Barrier methods
Implantable contraceptives
Intravaginal contraceptives
Ovulation inducers
Complementary:
Uterotonics
Antioxytocics (tocolytics)
Other medicines administered to the mother
Medicines administered to the neonate
Complementary:
Peritoneal dialysis solution
Complementary:
- Intraperitoneal dialysis solution (of appropriate composition)α
Medicines for mental and behavioural disorders
Medicines used in psychotic disorders
- Fluphenazine[note 168]
- Haloperidol[note 169]
- Olanzapine
- Paliperidone[note 170]
- Risperidone[note 171]
Complementary:
Medicines used in mood disorders
Medicines used in depressive disorders
Medicines used in bipolar disorders
- Carbamazepine
- Lithium carbonate
- Quetiapine[note 173]
- Valproic acid (sodium valproate)[note 17]
Medicines for anxiety disorders
Medicines used for obsessive compulsive disorders
Medicines for disorders due to psychoactive substance use
Medicines for alcohol use disorders
Medicines for nicotine use disorders
Complementary:
Medicines acting on the respiratory tract
Antiasthmatic medicines and medicines for chronic obstructive pulmonary disease
Solutions correcting water, electrolyte and acid-base disturbances
Oral
Parenteral
- Glucose
- Glucose with sodium chloride
- Potassium chloride
- Sodium chloride
- Sodium hydrogen carbonate
- Sodium lactate, compound solution (Ringer's lactate solution)
Miscellaneous
Vitamins and minerals
- Ascorbic acid
- Calcium
- Colecalciferol[note 181]
- Ergocalciferol[note 182]
- Iodine
- Multiple micronutrient powder
- Nicotinamide
- Pyridoxine
- Retinol
- Riboflavin
- Thiamine
Complementary:
Ear, nose and throat medicines
Medicines for diseases of joints
Medicines used to treat gout
Disease-modifying anti-rheumatic drugs (DMARDs)
Complementary:
Medicines for juvenile joint diseases
Complementary:
Dental medicines and preparations
- Fluoride
- Glass ionomer cement
- Resin-based composite (low-viscosity)[note 186]
- Resin-based composite (high-viscosity)[note 187]
- Silver diamine fluoride
Notes
An α indicates the medicine is on the complementary list for which specialized diagnostic or monitoring or training is needed. An item may also be listed as complementary on the basis of higher costs or a less attractive cost-benefit ratio.[4][14]
- ↑ (For use in spinal anaesthesia during delivery, to prevent hypotension).
- ↑ No more than 30% oxygen should be used to initiate resuscitation of neonates less than or equal to 32 weeks of gestation.
- ↑ Not in children less than three months.
- ↑ Not recommended for anti‐inflammatory use due to lack of proven benefit to that effect.
- ↑ For the management of cancer pain
- ↑ Hydromorphone and oxycodone are alternatives
- ↑ For the management of cancer pain.
- 1 2 Dolasetron, granisetron, palonosetron, and tropisetron are alternatives
- ↑ Cetirizine and fexofenadine are alternatives
- ↑ There may be a role for sedating antihistamines for limited indications (EMLc).
- ↑ Prednisone is an alternative
- ↑ For use as adjunctive therapy for treatment-resistant partial or generalized seizures.
- ↑ Diazepam and midazolam are alternatives
- ↑ For use in eclampsia and severe pre‐eclampsia and not for other convulsant disorders.
- ↑ For buccal administration when solution for oromucosal administration is not available.
- ↑ The presence of both 25 mg/5 mL and 30 mg/5 mL strengths on the same market would cause confusion in prescribing and dispensing and should be avoided.
- 1 2 3 Avoid use in pregnancy and in women and girls of child-bearing potential, unless alternative treatments are ineffective or not tolerated because of the high risk of birth defects and developmental disorders in children exposed to valproate in the womb.
- 1 2 3 4 5 6 7 8 9 10 11 Including quality-assured biosimilars
- ↑ Trihexyphenidyl is an alternative
- ↑ benserazide is an alternative for carbidopa
- ↑ Oxamniquine is listed for use when praziquantel treatment fails.
- ↑ > 1 month.
- ↑ Only for the presumptive treatment of epidemic meningitis in children older than two years and in adults.
- ↑ Alternatives are 4th level ATC chemical subgroup (J01CF Beta-lactamase resistant penicillins)
- ↑ cloxacillin, dicloxacillin and flucloxacillin are preferred for oral administration due to better bioavailability.
- ↑ Use in children <8 years only for life-threatening infections when no alternative exists.
- ↑ Procaine benzylpenicillin is not recommended as first-line treatment for neonatal sepsis except in settings with high neonatal mortality, when given by trained health workers in cases where hospital care is not achievable.
- ↑ Third-generation cephalosporin of choice for use in hospitalized neonates.
- ↑ Do not administer with calcium and avoid in infants with hyperbilirubinemia.
- ↑ > 41 weeks corrected gestational age.
- ↑ Erythromycin is an alternative as second choice treatment for pharyngitis in children (EMLc only)
- ↑ For use in combination regimens for eradication of H. pylori in adults.
- ↑ Vancomycin powder for injection may also be used for oral administration
- ↑ Imipenem/cilastatin is an alternative for complicated intraabdominal infections and high-risk febrile neutropenia only, except for acute bacterial meningitis in neonates, where meropenem is preferred
- ↑ Tedizolid phosphate is an alternative
- ↑ For use only in patients with HIV receiving protease inhibitors.
- ↑ For use only in combination with meropenem or imipenem/cilastatin.
- ↑ Terizidone is an alternative
- ↑ Prothionamide is an alternative
- ↑ Imipenem/cilastatin is an alternative
- ↑ For treatment of chronic pulmonary aspergillosis, histoplasmosis, sporotrichosis, paracoccidioidomycosis, mycoses caused by Talaromyces marneffei and chromoblastomycosis; and prophylaxis of histoplasmosis and infections caused by Talaromyces marneffei in AIDS patients.
- ↑ For treatment of chronic pulmonary aspergillosis and acute invasive aspergillosis.
- ↑ Anidulafungin and caspofungin are alternatives
- ↑ Valaciclovir is an alternative
- ↑ also indicated for pre-exposure prophylaxis.
- ↑ > 6 weeks
- ↑ > 3 years
- ↑ For use in pregnant women and in second-line regimens in accordance with WHO treatment guidelines.
- 1 2 lamivudine is an alternative for emtricitabine
- ↑ combination also indicated for pre-exposure prophylaxis
- ↑ For the treatment of viral haemorrhagic fevers
- ↑ For the treatment of cytomegalovirus retinitis (CMVr).
- ↑ For severe illness due to confirmed or suspected influenza virus infection in critically ill hospitalized patients
- ↑ For the treatment of cytomegalovirus retinitis (CMVr).
- ↑ Pangenotypic when used in combination with sofosbuvir
- ↑ Pangenotypic when used in combination with sofosbuvir
- ↑ Pangenotypic when used in combination with daclatasvir or ravidasvir
- ↑ For the treatment of hepatitis C, in combination with direct acting anti-viral medicines
- ↑ > 25 kg.
- ↑ Tinidazole is an alternative
- ↑ Liposomal amphotericin B has a better safety profile than the sodium deoxycholate formulation and should be prioritized for selection and use depending on local availability and cost.
- 1 2 To be used in combination with artesunate 50 mg.
- ↑ For use in the management of severe malaria.
- ↑ Not recommended in the first trimester of pregnancy or in children below 5 kg.
- ↑ To be used in combination with either amodiaquine, mefloquine, or sulfadoxine + pyrimethamine.
- ↑ Other combinations that deliver the target doses required such as 153 mg or 200 mg (as hydrochloride) with 50 mg artesunate are alternatives
- ↑ > 5 kg
- ↑ For use only for the treatment of Plasmodium vivax infection.
- ↑ > 5 kg
- ↑ For use only in combination with quinine.
- ↑ Only for use to achieve radical cure of Plasmodium vivax and Plasmodium ovale infections, given for 14 days.
- ↑ For use only in the management of severe malaria, and should be used in combination with doxycycline.
- ↑ Only in combination with artesunate 50 mg.
- ↑ For use only in Central American regions, for Plasmodium vivax infections.
- ↑ > 8 years.
- ↑ > 5 kg or > 3 months.
- ↑ For use only in combination with chloroquine.
- ↑ For the treatment of 1st and 2nd stage human African trypanosomiasis due to Trypanosoma brucei gambiense infection.
- ↑ To be used for the treatment of Trypanosoma brucei gambiense infection.
- ↑ To be used for the treatment of the initial phase of Trypanosoma brucei rhodesiense infection.
- ↑ To be used for the treatment of Trypanosoma brucei gambiense infection
- ↑ Only to be used in combination with eflornithine, for the treatment of Trypanosoma brucei gambiense infection.
- ↑ The presence of both 120 mg/5 mL and 125 mg/5mL strengths on the same market would cause confusion in prescribing and dispensing and should be avoided.
- 1 2 Certolizumab pegol, etanercept, golimumab and infliximab are alternatives, including quality-assured biosimilars
- ↑ Afatinib and gefitinib are alternatives
- ↑ Pembrolizumab is an alternative, including quality-assured biosimilars
- ↑ Enzalutamide is an alternative
- ↑ Alternatives are 4th level ATC chemical subgroup (L02BG Aromatase inhibitors)
- ↑ Flutamide and nilutamide are alternatives
- ↑ Goserelin and triptorelin are alternatives
- ↑ Prednisone is an alternative
- ↑ Biscuit or paste of nutritional composition as determined by the UN joint statement on the community-based management of severe acute malnutrition and Codex alimentarius guidelines.
- ↑ periconceptual use for prevention of first occurrence of neural tube defects
- ↑ Epoetin alfa, beta and theta; darbepoetin alfa; methoxy polyethylene glycol-epoetin beta; and their quality-assured biosimilars are alternatives
- ↑ Apixaban, edoxaban, and rivaroxaban are alternatives
- ↑ Alternatives are dalteparin and nadroparin, including their quality-assured biosimilars.
- ↑ Deferiprone is an alternative
- ↑ cryoprecipitate (not pathogen-reduced) is an alternative
- ↑ Coagulation factor IX complex is an alternative
- ↑ Polygeline, injectable solution, 3.5% is considered an alternative
- 1 2 3 Carvedilol and metoprolol are alternatives
- ↑ Alternatives are 4th level ATC chemical subgroup (C08CA Dihydropyridine derivatives)
- ↑ Includes atenolol, carvedilol, and metoprolol as alternatives. Atenolol should not be used as a first-line agent in uncomplicated hypertension in patients > 60 years.
- ↑ Alternatives are 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain)
- ↑ Hydralazine is listed for use only in the acute management of severe pregnancy-induced hypertension. Its use in the treatment of essential hypertension is not recommended in view of the evidence of greater efficacy and safety of other medicines.
- 1 2 3 Chlorothiazide, chlorthalidone, and indapamide are alternatives
- ↑ Alternatives are 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain) (for lisinopril) and 4th level ATC chemical subgroup (C08CA Dihydropyridine derivatives) (for amlodipine)
- ↑ Alternatives are 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain) (for lisinopril) and chlorthalidone, chlorothiazide, indapamide (for hydrochlorothiazide)
- 1 2 Alternatives are 4th level ATC chemical subgroup (C09CA Angiotensin II receptor blockers (ARBs), plain)
- ↑ Methyldopa is listed for use only in the management of pregnancy-induced hypertension. Its use in the treatment of essential hypertension is not recommended in view of the evidence of greater efficacy and safety of other medicines.
- ↑ Alternatives are 4th level ATC chemical subgroup (C09CA Angiotensin II receptor blockers (ARBs), plain) (for telmisartan) and 4th level ATC chemical subgroup (C08CA Dihydropyridine derivatives) (for amlodipine)
- ↑ Alternatives are 4th level ATC chemical subgroup (C09CA Angiotensin II receptor blockers (ARBs), plain) (for telmisartan) and chlorthalidone, chlorothiazide, indapamide (for hydrochlorothiazide)
- ↑ Alternatives are 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain)
- ↑ Bumetanide and torasemide are alternatives
- ↑ For use in high‐risk patients. Atorvastatin, fluvastatin, lovastatin, and pravastatin are alternatives
- 1 2 fluvastatin, lovastatin, pravastatin, and simvastatin are alternatives for atorvastatin
- 1 2 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain) are alternatives for ramipril
- ↑ atorvastatin, fluvastatin, lovastatin, and pravastatin are alternatives for simvastatin
- ↑ bisoprolol, carvedilol, and metoprolol are alternatives for atenolol
- ↑ chlorthalidone, chlorothiazide, and indapamide are alternatives for hydrochlorothiazide
- ↑ 4th level ATC chemical subgroup (C09AA ACE inhibitors, plain) are alternatives for perindopril
- ↑ 4th level ATC chemical subgroup (C08CA Dihydropyridine derivatives) are alternatives for amlodipine
- ↑ Alternatives are 4th level ATC chemical subgroup (D01AC Imidazole and triazole derivatives) excluding combinations
- ↑ Alternatives are 4th level ATC chemical subgroup (D07AC Corticosteroids, potent (group III))
- ↑ Alternatives are 4th level ATC chemical subgroup (D07AA Corticosteroids, weak (group I))
- ↑ Calcitriol and tacalcitol are alternatives
- ↑ Podophyllotoxin is an alternative
- ↑ precipitated sulfur topical ointment is an alternative
- ↑ Atropine and cyclopentolate are alternatives
- ↑ Propanol is an alternative
- ↑ Iodine is an alternative
- ↑ Alternatives are 4th level ATC chemical subgroup (D08AE Phenol and derivatives)
- ↑ Bumetanide and torasemide are alternatives
- ↑ Chlorothiazide and chlorthalidone are alternatives
- ↑ Alternatives are 4th level ATC chemical subgroup (A02BC Proton pump inhibitors) excluding combinations
- ↑ Alternatives are 4th level ATC chemical subgroup (A02BA H2-receptor antagonists) excluding combinations
- ↑ Mesalazine is an alternative
- ↑ Bisacodyl is an alternative
- ↑ In acute diarrhoea zinc sulfate should be used as an adjunct to oral rehydration salts.
- ↑ Norethisterone is an alternative
- ↑ Insulin degludec, insulin detemir, and insulin glargine, including quality-assured biosimilars are alternatives
- ↑ Canagliflozin and dapagliflozin are alternatives
- ↑ Glibenclamide not suitable above 60 years. Alternatives are 4th level ATC chemical subgroup (A10BB Sulfonylureas)
- 1 2 Carbimazole is an alternative depending on local availability
- ↑ For use when alternative first-line treatment is not appropriate or available; and in patients during the first trimester of pregnancy.
- ↑ For use when alternative first-line treatment is not appropriate or available
- ↑ bromocriptine is an alternative
- ↑ Exact type to be defined locally
- 1 2 3 Recommended for certain regions
- 1 2 3 4 5 6 Recommended for some high-risk populations
- 1 2 3 Recommended only for immunization programmes with certain characteristics
- ↑ atracurium is an alternative
- ↑ For infections due to Chlamydia trachomatis or Neisseria gonorrhoeae.
- ↑ Amikacin, kanamycin, netilmicin, and tobramycin are alternatives
- ↑ Alternatives are 4th level ATC chemical subgroup (S01AE Fluoroquinolones)
- ↑ Chlortetracycline and oxytetracycline are alternatives
- ↑ Alternatives are 4th level ATC chemical subgroup (S01HA Local anaesthetics) excluding cocaine and combinations
- ↑ Carbachol is an alternative
- ↑ Alternatives are 4th level ATC chemical subgroup (S01ED Beta blocking agents) excluding combinations
- ↑ Cyclopentolate hydrochloride or homatropine hydrobromide are alternatives only for the EMLc
- ↑ For use in women actively breastfeeding at least 4 times per day
- ↑ anastrozole is an alternative
- ↑ Methylergometrine is an alternative
- ↑ Where permitted under national law and where culturally acceptable.
- ↑ Only for use for induction of labour where appropriate facilities are available.
- ↑ Indometacin is an alternative
- ↑ Prostaglandin E2 is an alternative
- ↑ haloperidol decanonate and zuclopenthixol decanonate are alternatives
- ↑ Chlorpromazine is an alternative for the tablet
- ↑ Risperidone injection is an alternative
- ↑ aripiprazole, olanzapine, paliperidone, and quetiapine are alternatives
- 1 2 3 Citalopram, escitalopram, fluvoxamine, paroxetine, and sertraline are alternatives
- ↑ aripiprazole, olanzapine, and paliperidone are alternatives
- ↑ lorazepam is an alternative
- ↑ For short-term emergency management of acute and severe anxiety symptoms only
- ↑ buprenorphine is an alternative. The medicines should only be used within an established support programme.
- ↑ Beclometasone, ciclesonide, flunisolide, fluticasone, and mometasone are alternatives
- ↑ Beclometasone/formoterol, budesonide/salmeterol, fluticasone/formoterol, fluticasone furoate/vilanterol, and mometasone/formoterol are alternatives
- ↑ Terbutaline is an alternative
- ↑ Aclidinium, glycopyrronium, and umeclidinium are alternatives
- ↑ Ergocalciferol is an alternative
- ↑ Colecalciferol is an alternative
- ↑ Ofloxacin is an alternative
- ↑ For use for rheumatic fever, juvenile arthritis, Kawasaki disease
- ↑ triamcinolone acetonide is an alternative
- ↑ of any type for use as dental sealant
- ↑ of any type for use as dental filling material
References
- 1 2 "The WHO Essential Medicines List (EML): 30th anniversary". World Health Organization. Archived from the original on 27 May 2014. Retrieved 26 June 2016.
- 1 2 3 4 "Essential medicines". World Health Organization. Archived from the original on 2 October 2008. Retrieved 19 January 2017.
- ↑ Persaud N, Jiang M, Shaikh R, Bali A, Oronsaye E, Woods H, et al. (June 2019). "Comparison of essential medicines lists in 137 countries". Bull. World Health Organ. 97 (6): 394–404C. doi:10.2471/BLT.18.222448. hdl:10665/325509. ISSN 0042-9686. PMC 6560372. PMID 31210677.
- 1 2 3 4 5 6 "19th WHO Model List of Essential Medicines" (PDF). World Health Organization. April 2015. p. Annex 1. Archived (PDF) from the original on 13 May 2015. Retrieved 17 January 2017.
- 1 2 Bansal D, Purohit VK (January 2013). "Accessibility and use of essential medicines in health care: Current progress and challenges in India". Journal of Pharmacology & Pharmacotherapeutics. 4 (1): 13–18. doi:10.4103/0976-500X.107642. PMC 3643337. PMID 23662019.
- ↑ World Health Organization (2003). The selection and use of essential medicines (Report). World Health Organization (WHO). hdl:10665/42826. ISBN 92-4-120920-8. WHO technical report series 920.
- ↑ Beall R (2016). "Patents and the WHO Model List of Essential Medicines (18th Edition): Clarifying the Debate on IP and Access" (PDF). World Intellectual Property Organization (WIPO). Archived (PDF) from the original on 17 August 2017. Retrieved 3 May 2017.
- ↑ World Health Organization (1977). The selection of essential drugs: report of a WHO expert committee [meeting held in Geneva from 17 to 21 October 1977]. Geneva: World Health Organization. hdl:10665/41272. ISBN 92-4-120615-2. Technical report series; no. 615.
- ↑ Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, de Joncheere CP, Ewen MA, et al. (January 2017). "Essential medicines for universal health coverage". Lancet. 389 (10067): 403–476. doi:10.1016/S0140-6736(16)31599-9. PMC 7159295. PMID 27832874.
- 1 2 3 "WHO Model Lists of Essential Medicines". World Health Organization. Archived from the original on 2005-10-14. Retrieved 2022-11-05.
The current versions are the 21st WHO Essential Medicines List (EML) and the 7th WHO Essential Medicines List for Children (EMLc) updated in June 2019.
- ↑ Prakash B, Nadig P, Nayak A (2016). "Rational Prescription for a Dermatologist". Indian Journal of Dermatology. 61 (1): 32–38. doi:10.4103/0019-5154.174017. PMC 4763692. PMID 26955092.
- 1 2 World Health Organization (2017). WHO model list of essential medicines, 20th list (March 2017, amended August 2017). Geneva. hdl:10665/273826.
- ↑ "Essential Medicines List and WHO Model Formulary". World Health Organization. Archived from the original on 3 August 2008. Retrieved 5 May 2018.
- 1 2 3 4 World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ World Health Organization (2019). Executive summary: the selection and use of essential medicines 2019: report of the 22nd WHO Expert Committee on the selection and use of essential medicines. Geneva. hdl:10665/325773. WHO/MVP/EMP/IAU/2019.05. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Strengthening access to essential medicines". World Health Organization. Archived from the original on 22 April 2020. Retrieved 3 May 2020.
- 1 2 3 4 World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- 1 2 World Health Organization (2021). Executive summary: the selection and use of essential medicines 2021: report of the 23rd WHO Expert Committee on the selection and use of essential medicines: virtual meeting, 21 June–2 July 2021. Geneva: World Health Organization. hdl:10665/345554. WHO/MHP/HPS/EML/2021.01.
- ↑ World Health Organization (2021). The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2021 (including the 22nd WHO model list of essential medicines and the 8th WHO model list of essential medicines for children). Geneva: World Health Organization. hdl:10665/351172. ISBN 978-92-4-004114-1. WHO technical report series;1035. License: CC BY-NC-SA 3.0 IGO.
- ↑ "WHO Model Lists of Essential Medicines". www.who.int. Archived from the original on 2020-11-07. Retrieved 2023-08-08.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines for children: 7th list 2019. Geneva. hdl:10665/325772. WHO/MVP/EMP/IAU/2019.07. License: CC BY-NC-SA 3.0 IGO.
- ↑ World Health Organization (2021). World Health Organization model list of essential medicines for children: 8th list (2021). Geneva: World Health Organization. hdl:10665/345534. WHO/MHP/HPS/EML/2021.03.
- 1 2 World Health Organization (2023). The selection and use of essential medicines 2023: web annex B: World Health Organization model list of essential medicines for children: 9th list (2023). Geneva: World Health Organization. hdl:10665/371091. WHO/MHP/HPS/EML/2023.03.
- ↑ Rose K, Anker JN (2010). Guide to Paediatric Drug Development and Clinical Research. Karger Medical and Scientific Publishers. p. 42. ISBN 978-3-8055-9362-5. Archived from the original on 2023-01-11. Retrieved 2020-09-20.
- ↑ Seyberth HW, Rane A, Schwab M (2011). Pediatric Clinical Pharmacology. Springer Science & Business Media. p. 358. ISBN 978-3-642-20195-0. Archived from the original on 2023-01-11. Retrieved 2020-09-20.
- ↑ Hoppu K (June 2017). "Essential Medicines for Children". Clinical Pharmacology and Therapeutics. 101 (6): 718–720. doi:10.1002/cpt.661. PMID 28182281. S2CID 23873145.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: executive summary of the report of the 24th WHO Expert Committee on Selection and Use of Essential Medicines, 24 28 April 2023. Geneva: World Health Organization. hdl:10665/371291. WHO/MHP/HPS/EML/2023.01.
- ↑ "The WHO Essential Medicines List Antibiotic Book". World Health Organization (WHO). 24 November 2021. Archived from the original on 2022-11-11. Retrieved 2022-10-06.
- ↑ The WHO AWaRe (Access, Watch, Reserve) antibiotic book. Geneva: World Health Organization (WHO). 2022. ISBN 978-92-4-006238-2. Archived from the original on 13 August 2023. Retrieved 29 January 2023.
- ↑ The WHO AWaRe (Access, Watch, Reserve) antibiotic book - Infographics. Geneva: World Health Organization (WHO). 2022. WHO/MHP/HPS/EML/2022.02. Archived from the original on 29 January 2023. Retrieved 29 January 2023.
Further reading
- Serafini M, Cargnin S, Massarotti A, Pirali T, Genazzani AA (September 2020). "Essential Medicinal Chemistry of Essential Medicines". Journal of Medicinal Chemistry. 63 (18): 10170–10187. doi:10.1021/acs.jmedchem.0c00415. PMC 8007110. PMID 32352778.
- Stuart MC, Kouimtzi M, Hill SR, eds. (2009). WHO Model Formulary 2008. World Health Organization. hdl:10665/44053. ISBN 978-92-4-154765-9.
- The selection and use of essential medicines. Twentieth report of the WHO Expert Committee 2015 (including 19th WHO Model List of Essential Medicines and 5th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization. 2015. hdl:10665/189763. ISBN 978-92-4-069494-1. ISSN 0512-3054. WHO technical report series; no. 994.
- The selection and use of essential medicines: report of the WHO Expert Committee, 2017 (including the 20th WHO Model List of Essential Medicines and the 6th Model List of Essential Medicines for Children). Geneva: World Health Organization. 2017. hdl:10665/259481. ISBN 978-92-4-121015-7. ISSN 0512-3054. WHO technical report series; no. 1006.
- The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization. 2019. hdl:10665/330668. ISBN 978-92-4-121030-0. ISSN 0512-3054. WHO technical report series;1021.
- "Additions and deletions of medicines on the WHO model lists of essential medicines: 1977–2017". World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.01. Archived from the original on 2023-08-13. Retrieved 2023-08-20.