Rabies vaccine
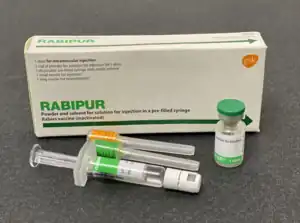 Rabies (RABIPUR) vaccine | |
| Vaccine description | |
|---|---|
| Target disease | Rabies |
| Type | Inactivated |
| Names | |
| Trade names | RabAvert, Rabipur, Rabivax, others |
| Other names | Rabies virus inactivated antigen |
| Clinical data | |
| Main uses | Prevention of rabies[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category | |
| Routes of use | Intramuscular injection |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607023 |
| Legal | |
| License data | |
| Legal status |
|
Rabies vaccine is a vaccine used to prevent rabies.[1] It is used in high risk groups before exposure to rabies virus, and can be used if an unvaccinated person comes into contact with the rabies virus.[1][3] Doses are usually given by injection into muscle.[1] The immunity that develops is long lasting after a full course.[1] Spread of rabies to humans can also be prevented by vaccinating dogs.[1]
It is recommended for people at high risk of coming into contact with rabies, when it is given as a course of 2 or 3 doses at 0, 7, and 21 or 28 days.[3][4] A blood test every 6 to 24 months can check immunity.[3] After exposure to the virus such as from a dog or bat bite, the vaccine is given as a course of 4 doses at 0, 3, 7 and 14 days, along with rabies immunoglobulin.[1][3] People with a weakened immune system may require an additional dose at 28 days.[3]
There are a number of vaccines available that are both safe and effective.[1] They may be safely used in all age groups.[1] About 40 percent of people develop a brief period of redness and pain at the injection site.[1] About 10 percent of people may have fever, headaches, or nausea.[1] After exposure to rabies there is no contraindication to its use.[1] Most vaccines do not contain thimerosal.[1] Given in pregnancy, it is not known to harm the baby.[5]
The first rabies vaccine was introduced in 1885, and was followed by an improved version in 1908.[6] Millions of people globally have been vaccinated and it is estimated that this saves more than 250,000 people a year.[1] It is on the World Health Organization's List of Essential Medicines.[7] The wholesale cost in the developing world is between US$44 and US$78 for a course of treatment as of 2014.[8] In the United States a course of rabies vaccine is more than US$750.[9] In the United Kingdom it costs around £120 for a course of treatment as of 2021.[5] In Canada it costs about $CAD230 per dose as of 2023.[10]
Medical uses
Before exposure
The World Health Organization (WHO) recommends vaccinating in those who are at high risk of the disease including children who live in areas where it is common.[1] Other groups may include veterinarians, researchers, or people planning to travel to regions where rabies is common.[11] Two to three doses of the vaccine are given over a one-month period on days zero, seven, and either twenty-one or twenty-eight.[11][1][4]
After exposure
For individuals who have been potentially exposed to the virus, four doses over two weeks are recommended, as well as an injection of rabies immunoglobulin with the first dose.[12] This is known as post exposure vaccinations.[13] For people who have previously been vaccinated, only a single dose of the rabies vaccine is required.[13] Vaccination after exposure is neither a treatment nor a cure for rabies; it can only prevent the development of rabies in a person if given before the virus reaches the brain.[13] Because the rabies virus has a relatively long incubation period, post exposure vaccinations are typically highly effective.[1]
Additional doses
Immunity following a course of doses is typically long lasting.[1] Additional doses are not typically needed except in those at very high risk.[1] Those at high risk may have tests done to measure rabies antibody in the blood, and then get rabies boosters as needed.[11] Following administration of a booster dose, one study found 97% of immuno-competent individuals demonstrate protective levels of neutralizing antibodies at 10 years.[14]
Safety
Rabies vaccines are safe in all age groups.[1][15] About 35 to 45 percent of people develop a brief period of redness and pain at the injection site.[1] About 5 to 15 percent of people may have fever, headaches, or nausea.[1] Because rabies is invariably fatal, there is no contraindication to its use after exposure.[1]
Most vaccines do not contain thimerosal.[1] Vaccines made from nerve tissue are used in a few countries, mainly in Asia and Latin America, but are less effective and have greater side effects.[1] Their use is thus not recommended by the World Health Organization.[1]
Types
The human diploid cell rabies vaccine (H.D.C.V.) was started in 1967. Human diploid cell rabies vaccines are inactivated vaccines made using the attenuated Pitman-Moore L503 strain of the virus.[16]
In addition to these developments, newer and less expensive purified chicken embryo cell vaccines (CCEEV) and purified Vero cell rabies vaccines are now available and are recommended for use by the WHO.[1] The purified Vero cell rabies vaccine uses the attenuated Wistar strain of the rabies virus, and uses the Vero cell line as its host. CCEEVs can be used in both pre and post exposure vaccinations. CCEEVs use inactivated rabies virus grown from either embryonated eggs or in cell cultures and are safe for use in humans and animals.[1][17]
History
Virtually all infections with rabies resulted in death until two French scientists, Louis Pasteur and Émile Roux, developed the first rabies vaccination in 1885. Nine-year-old Joseph Meister (1876–1940), who had been mauled by a rabid dog, was the first human to receive this vaccine.[18] The treatment started with subcutaneous injection on 6 July 1885, at 8:00 PM, which was followed with 12 additional doses administered over the following 10 days. The first injection was derived from the spinal cord of an inoculated rabbit which had died of rabies 15 days earlier. All the doses were obtained by attenuation but later ones were progressively more virulent.[19]
Pasteur-Roux vaccine attenuated the harvested virus samples by allowing them to dry for 5 to 10 days. Similar nerve tissue-derived vaccines are still used now in some countries, and while they are much cheaper than modern cell culture vaccines, they are not as effective.[20] Neural tissue vaccines also carry a certain risk of neurological complications.[21]
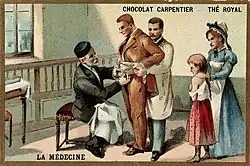 Pasteur inoculating a man with the rabies virus
Pasteur inoculating a man with the rabies virus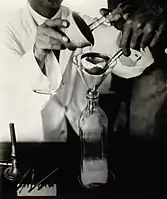 Preparation of the rabies vaccin at the Pasteur Institute, Kasauli, India (1910)
Preparation of the rabies vaccin at the Pasteur Institute, Kasauli, India (1910) Child receiving rabies innoculation (1929)
Child receiving rabies innoculation (1929) Laboratory technician inoculates eggs in the process of producing rabies vaccine - Iran (1967)
Laboratory technician inoculates eggs in the process of producing rabies vaccine - Iran (1967)
Cost
A limitation to acquiring preexposure rabies immunization for travellers from developed countries, has been the cost of the vaccine, which requires 3 clinic visits prior to travel. In 2015, in the United States, a course of three IM doses could exceed $1,000 in cost.[22]
Even after the modern cell-culture rabies vaccine was first introduced, in the early 1980s, the cost of $45 per dose was considered to be too expensive.
However, "intradermal (ID) rabies immunization began almost as soon as the intramuscular (IM) human diploid cell vaccine (HDCV) was manufactured. By reconstituting the 1.0 mL of vaccine in the vial, practitioners could draw up approximately eight 0.1-mL doses. One problem was that the entire vial had to be used within a few hours of reconstituting, meaning that a provider had to either be in a busy clinic or line up groups of people, such as families, for rabies immunization at the same time."[22]
Veterinary use


Pre-exposure immunization has been used on domesticated and wild populations. In many jurisdictions, domestic dogs, cats, ferrets, and rabbits are required to be vaccinated.[23]
Dogs
Aside from vaccinating humans, another approach was also developed by vaccinating dogs to prevent the spread of the virus. In 1979 the Van Houweling Research Laboratory of the Silliman University Medical Center in Dumaguete in the Philippines[24] developed and produced a dog vaccine that gave a three-year immunity from rabies. The development of the vaccine resulted in the elimination of rabies in many parts of the Visayas and Mindanao Islands. The successful program in the Philippines was later used as a model by other countries, such as Ecuador and the Yucatan State of Mexico, in their fight against rabies conducted in collaboration with the World Health Organization.[25]
In Tunisia a rabies control program was initiated to give dog owners free vaccination to promote mass vaccination which was sponsored by their government. The vaccine is known as Rabisin (Mérial), which is a cell based rabies vaccine only used countrywide. Vaccinations are often administered when owners take in their dogs for check-ups and visits at the vet.[26]
Wild animals
Wildlife species, primarily bats, raccoons, skunks, and foxes, act as reservoir species for different variants of the rabies virus.[15][27] This results in the general occurrence of rabies as well as outbreaks in animal populations.[27] Approximately 90% of all reported rabies cases in the US are from wildlife.[27]
Oral rabies vaccine
There is an oral vaccination in pellet form which can be left out for wild animals to produce a herd immunity effect.[28] Oral rabies vaccination (ORV) programs have been used in many countries in an effort to control the spread of rabies and limit the risk of human contact with the rabies virus.[27] ORV programs were initiated in Europe in the 1980s, Canada in 1985, and in the United States in 1990.[29] ORV is a preventive measure to eradicate rabies in wild animal vectors of disease, mainly foxes, raccoons, raccoon dogs, coyotes and jackals, but also can be used for dogs in developing countries.[30] ORV programs typically use edible baits to deliver the vaccine to targeted animals. ORV baits consist of a small packet containing the oral vaccine which is then either coated in a fishmeal paste or encased in a fishmeal-polymer block.[27] When an animal bites into the bait, the packets burst and the vaccine is administered.[29] Current research suggests that if adequate amounts of the vaccine is ingested, immunity to the virus should last for upwards of one year.[31] By immunizing wild or stray animals, ORV programs work to create a buffer zone between the rabies virus and potential contact with humans, pets, or livestock.[29] The effectiveness of ORV campaigns in specific areas is determined through trap-and-release methods.[32] Titer tests are performed on the blood drawn from the sample animals in order to measure rabies antibody levels in the blood.[32] Baits are usually distributed by aircraft to more efficiently cover large, rural regions. In order to place baits more precisely and to minimize human and pet contact with baits, however, they are distributed by hand in suburban or urban regions.[29] The potential for human contact with baits is a present concern for OPV programs, but the oral vaccine does not contain the whole rabies virus and has been proven safe in over 60 animal species including cats and dogs.[31] The idea of wildlife vaccination was conceived during the 1960s, and modified-live rabies viruses were used for the experimental oral vaccination of carnivores by the 1970s. The development of safe and effective rabies virus vaccines applied in attractive baits resulted in the first field trials in Switzerland in 1978 to immunize red foxes.[33] ORV programs have seen success in preventing the westward spread of raccoon variant rabies in the United States and even eradicating rabies in red foxes in Switzerland.[34][35]
Imrab is an example of a veterinary rabies vaccine containing the Pasteur strain of killed rabies virus. Several different types of Imrab exist, including Imrab, Imrab 3, and Imrab Large Animal. Imrab 3 has been approved for ferrets and, in some areas, pet skunks.[36][37] The reason why these oral vaccines that enter the body through the GI tract are able to convey resistance to rabies is due to the usage of a live human adenovirus type 5 vector. Adenovirus, a common viral pathogen that infects the GI tract and causes diarrhea is genetically altered to express rabies surface proteins, thereby allowing the adenovirus to infect GI tract cells. This enables the viral vector to infect cells in the GI and stimulate a cellular and humoral response that would provide immunity in the case of being bitten by an infected animal and being infected via blood.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 World Health Organization (2018). "Rabies vaccines: WHO position paper – April 2018". Weekly Epidemiological Record. 93 (16): 201–19. hdl:10665/272372.
- Lay summary in: (PDF) https://www.who.int/immunization/policy/position_papers/pp_rabies_summary_2018.pdf?ua=1.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help)
- Lay summary in: (PDF) https://www.who.int/immunization/policy/position_papers/pp_rabies_summary_2018.pdf?ua=1.
- 1 2 "Rabies vaccine, human diploid cell (Imovax Rabies) Use During Pregnancy". Drugs.com. 22 November 2019. Archived from the original on 29 December 2019. Retrieved 29 December 2019.
- 1 2 3 4 5 Lampiris, Harry W.; maddix, Daniel S. (2020). "Appendix: Vaccines, immune globulins, and other complex biologic products". In Katzung, Bertram G.; Trevor, Anthony J. (eds.). Basic and Clinical Pharmacology (15th ed.). New York: McGraw-Hill. p. 1229. ISBN 978-1-260-45231-0. Archived from the original on 2021-10-10. Retrieved 2021-12-28.
- 1 2 "Rabies Vaccine Information Statement | CDC". www.cdc.gov. 27 April 2023. Archived from the original on 6 November 2019. Retrieved 10 November 2023.
- 1 2 "14. Vaccines". British National Formulary (BNF) (82 ed.). London: BMJ Group and the Pharmaceutical Press. September 2021 – March 2022. pp. 1369–1392. ISBN 978-0-85711-413-6.
{{cite book}}: CS1 maint: date format (link) - ↑ Nunnally, Brian (2014). Vaccine Analysis: Strategies, Principles, and Control. Springer. p. 63. ISBN 9783662450246. Archived from the original on 2016-03-05.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Vaccine, Rabies". International Drug Price Indicator Guide. Archived from the original on 22 January 2018. Retrieved 6 December 2015.
- ↑ Shlim, David (June 24, 2019). "Perspectives: Intradermal Rabies Preexposure Immunization". Centers for Disease Control and Prevention (CDC). Archived from the original on 2 October 2015. Retrieved 26 December 2019.
- ↑ "Travel Clinic Fees". Nova Travel Clinic. Archived from the original on 2 June 2023. Retrieved 10 November 2023.
- 1 2 3 "Preexposure Vaccinations". Centers for Disease Control and Prevention (CDC). April 22, 2011. Archived from the original on 23 August 2019. Retrieved 19 November 2019.
- ↑ "Rabies Vaccine Information Statement". Centers for Disease Control and Prevention (CDC). 2009-10-06. Archived from the original on 2019-11-06. Retrieved 27 September 2019.
- 1 2 3 "Rabies Postexposure Prophylaxis (PEP)". Centers for Disease Control and Prevention (CDC). June 11, 2019. Archived from the original on 21 December 2019. Retrieved 19 November 2019.
- ↑ "An Advisory Committee Statement (ACS). Committee to Advise on Tropical Medicine and Travel (CATMAT). Statement on travellers and rabies vaccine" (PDF). Canada Communicable Disease Report (CCDR). 28 (ACS 4): 1–12. March 2002. ISSN 1481-8531. PMID 11889905. Archived (PDF) from the original on 2020-08-31. Retrieved 2020-01-07.
- 1 2 "National Rabies Management Program Overview". Animal and Plant Health Inspection Service (APHIS). Archived from the original on 3 August 2020. Retrieved 12 November 2019.
- ↑ "Rabies - Human Vaccines". World Health Organization (WHO). Archived from the original on 3 November 2012. Retrieved 1 October 2012.
- ↑ "Rabies". World Health Organization (WHO). Archived from the original on 15 February 2015. Retrieved 21 November 2019.
- ↑ Geison GL (1978). "Pasteur's work on rabies: Reexamining the ethical issues diagnosis for developing countries". Hastings Center Report. The Hastings Center. 8 (April): 26–. doi:10.2307/3560403. JSTOR 3560403. PMID 348641.
- ↑ Arnaud Tarantola (2017). "Four Thousand Years of Concepts Relating to Rabies in Animals and Humans, Its Prevention and Its Cure". Trop Med Infect Dis. 2 (2): 5. doi:10.3390/tropicalmed2020005. PMC 6082082. PMID 30270864.
- ↑ Plotkin, Stanley A. (1980). "Rabies Vaccine Prepared in Human Cell Cultures: Progress and Perspectives". Reviews of Infectious Diseases. 2 (3): 433–448. doi:10.1093/clinids/2.3.433. PMID 6158081.
- ↑ Srivastava, AK; Sardana, V; Prasad, K; Behari, M (March 2004). "Diagnostic dilemma in flaccid paralysis following anti-rabies vaccine". Neurol India. 52 (1): 132–3. PMID 15069272. Archived from the original on 2009-08-02.
- 1 2 Shlim, David (June 24, 2019). "Perspectives: Intradermal Rabies Preexposure Immunization". Centers for Disease Control and Prevention (CDC). Archived from the original on 2 October 2015. Retrieved 26 December 2019.
- ↑ "State Rabies Vaccination Laws for Domestic Dogs, Cats, and Ferrets in the United States". lawatlas.org. Archived from the original on 2020-01-22. Retrieved 2020-01-22.
- ↑ "Dr. George W. Beran's Biography" World Rabies Day 2010 at the Wayback Machine (archived April 15, 2010)(Positional parameters ignored). World Rabies Day. Retrieved 2010-04-23.
- ↑ "One World, One Health Rabies" Wayback Machine at the Wayback Machine (archived 2011-07-24).OneHealthInitiative.com. Retrieved 2010-04-23.
- ↑ Touihri; Zaouia, I.; Elhili, K.; Dellagi, K.; Bahloul, C. (23 Dec 2009). "Evaluation of Mass Vaccination Campaign Coverage Against Rabies in Dogs in Tunisia". Zoonoses and Public Health. Institut Pasteur de Tunis and Blackwell Verlag GmbH. 58 (2): 110–8. doi:10.1111/j.1863-2378.2009.01306.x. PMID 20042063.
- 1 2 3 4 5 "Oral Rabies Vaccination". Animal and Plant Health Inspection Service (APHIS). Archived from the original on 8 July 2020. Retrieved 12 November 2019.
- ↑ "What are the signs and symptoms of rabies?". Centers for Disease Control and Prevention (CDC). Archived from the original on 2015-11-09. Retrieved 2015-11-09.
- 1 2 3 4 "Oral Rabies Vaccine Information". Animal and Plant Health Inspection Service (APHIS). 12 November 2019. Archived from the original on 14 November 2019.
- ↑ "Oral rabies vaccination". Archived from the original on January 7, 2014. Retrieved February 21, 2014.
- 1 2 "Frequently Asked Questions". Animal and Plant Health Inspection Service (APHIS). 12 November 2019. Archived from the original on 17 August 2020.
- 1 2 "Oral Rabies Vaccination Program in the East" (PDF). Animal and Plant Health Inspection Service (APHIS). January 2011. Archived from the original (PDF) on 2017-02-11. Retrieved 2019-11-19.
- ↑ Rupprecht CE, Hanlon CA, Slate D (2004). "Oral vaccination of wildlife against rabies: opportunities and challenges in prevention and control". Dev Biol (Basel). 119: 173–84. PMID 15742629.
- ↑ "Oral Rabies Vaccine Project – Environmental Epidemiology". www.vdh.virginia.gov. Archived from the original on 2017-08-18. Retrieved 2017-07-23.
- ↑ "Switzerland's Kind of Gross, Incredibly Effective Anti-Rabies Weapon | Now I Know". nowiknow.com. Archived from the original on 2016-02-12. Retrieved 2017-07-23.
- ↑ Merial US.Merial.com : Equine : Products : IMRAB® 3 at the Wayback Machine (archived April 9, 2005)
- ↑ Aspen Skunk Rabies Research, Inc. This site has been suspended at the Wayback Machine (archived May 25, 2011)
External links
| Identifiers: |
|---|
- Availability by country Archived 2023-08-04 at the Wayback Machine
- "Rabies Vaccine Information Statement". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 2019-11-06. Retrieved 2019-12-28.
- "Imovax". U.S. Food and Drug Administration (FDA). STN: 103931. Archived from the original on 2020-09-18. Retrieved 2020-01-19.
- "RabAvert - Rabies Vaccine". U.S. Food and Drug Administration (FDA). STN: BL 103334. Archived from the original on 2019-12-17. Retrieved 2020-01-19.
- "Rabipur Ampoule - Summary of Product Characteristics (SmPC)". electronic medicines compendium (emc). Archived from the original on 2019-02-03. Retrieved 2020-01-07.
- Rabies Vaccines at the US National Library of Medicine Medical Subject Headings (MeSH)