Allopurinol
 | |
 | |
| Names | |
|---|---|
| Trade names | Zyloprim, Caplenal, Zyloric, others |
IUPAC name
| |
| Clinical data | |
| Drug class | Xanthine oxidase inhibitor[1] |
| Main uses | High uric acid levels including in gout[2] |
| Side effects | Itchiness, rash, vomiting, kidney problems[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category | |
| Routes of use | By mouth (tablet), IV |
| Defined daily dose | 0.4 gram (by mouth or injection)[4] |
| Typical dose | 100 to 900 mg/day[5] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682673 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 78±20% |
| Protein binding | Negligible |
| Metabolism | Liver (80% oxipurinol, 10% allopurinol ribosides) |
| Elimination half-life | 2 h (oxipurinol 18–30 h) |
| Chemical and physical data | |
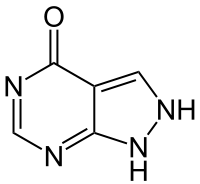
| Formula | C5H4N4O |
| Molar mass | 136.114 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Allopurinol, sold under the brand name Zyloprim among others, is a medication used to decrease high blood uric acid levels.[2] It is specifically used to prevent gout, prevent specific types of kidney stones, and for the high uric acid levels that can occur with chemotherapy.[6][1] It is taken by mouth or injected into a vein.[1]
Common side effects when used by mouth include itchiness and rash.[1] Common side effects when used by injection include vomiting and kidney problems.[1] While not recommended historically, starting allopurinol during an attack of gout appears to be safe.[7] In those already on the medication, it should be continued even during an acute gout attack.[7][6] While use during pregnancy does not appear to result in harm, this use has not been well studied.[3] Allopurinol is in the xanthine oxidase inhibitor family of medications.[1]
Allopurinol was approved for medical use in the United States in 1966.[1] It is on the World Health Organization's List of Essential Medicines.[8] Allopurinol is available as a generic medication and is not expensive.[9] The wholesale cost in the developing world is about US$0.81–3.42 per month.[10] In the United States a month of treatment costs less than $25.[11] In 2017, it was the 54th most prescribed medication in the United States with more than 14 million prescriptions.[12][13]
Medical uses
Gout
Allopurinol is used to reduce urate formation in conditions where urate deposition has already occurred or is predictable. The specific diseases and conditions where it is used include gouty arthritis, skin tophi, kidney stones, idiopathic gout; uric acid lithiasis; acute uric acid nephropathy; neoplastic disease and myeloproliferative disease with high cell turnover rates, in which high urate levels occur either spontaneously, or after cytotoxic therapy; certain enzyme disorders which lead to overproduction of urate, for example: hypoxanthine-guanine phosphoribosyltransferase, including Lesch–Nyhan syndrome; glucose 6-phosphatase including glycogen storage disease; phosphoribosyl pyrophosphate synthetase, phosphoribosyl pyrophosphate amidotransferase; adenine phosphoribosyltransferase.
It is also used to treat kidney stones caused by deficient activity of adenine phosphoribosyltransferase.
Tumor lysis syndrome
Allopurinol was also commonly used to treat tumor lysis syndrome in chemotherapeutic treatments, as these regimens can rapidly produce severe acute hyperuricemia;[14] however, it has gradually been replaced by urate oxidase therapy.[15] Intravenous formulations are used in this indication when people cannot take medicine by mouth.[16]
Inflammatory bowel disease
Allopurinol cotherapy is used to improve outcomes for people with inflammatory bowel disease and Crohn's disease who do not respond to thiopurine monotherapy.[17][18] Cotherapy has also been shown to greatly improve hepatoxicity side effects in treatment of IBD.[19] Cotherapy invariably requires dose reduction of the thiopurine, usually to one-third of the standard dose depending upon the patient's genetic status for thiopurine methyltransferase.[20]
Dosage
The typical dose by mouth is 100 to 900 mg per day.[5] With doses over 300 mg it maybe taken two or three times per day.[5]
The defined daily dose is 400 mg (by mouth or injection).[4]
Side effects

Because allopurinol is not a uricosuric, it can be used in people with poor kidney function. However, for people with impaired kidney function, allopurinal has two disadvantages. First, its dosing is complex.[21] Second, some people are hypersensitive to the drug, therefore its use requires careful monitoring.[22][23]
Allopurinol has rare but potentially fatal adverse effects involving the skin. The most serious adverse effect is a hypersensitivity syndrome consisting of fever, skin rash, eosinophilia, hepatitis, and worsened renal function.[22] Allopurinol is one of the drugs commonly known to cause Stevens–Johnson syndrome and toxic epidermal necrolysis, two life-threatening dermatological conditions.[22] More common is a less-serious rash that leads to discontinuing this drug.[22]
More rarely, allopurinol can also result in the depression of bone marrow elements, leading to cytopenias, as well as aplastic anemia. Moreover, allopurinol can also cause peripheral neuritis in some patients, although this is a rare side effect. Another side effect of allopurinol is interstitial nephritis.[24]
Allopurinol should not be given to people who are allergic to it.[14]
Interactions
Drug interactions are extensive, and are as follows:[14]
- Azathioprine and 6-mercaptopurine: Azathioprine is metabolised to 6-mercaptopurine which in turn is inactivated by the action of xanthine oxidase - the target of allopurinol. Giving allopurinol with either of these drugs at their normal dose will lead to overdose of either drug; only one-quarter of the usual dose of 6-mercaptopurine or azathioprine should be given;
- Didanosine: plasma didanosine Cmax and AUC values were approximately doubled with concomitant allopurinol treatment; it should not be co-administered with allopuroinol and if it must be, the dose of should be reduced and the person should be closely monitored.
Allopurinol may also increase the activity or half-life of the following drugs, in order of seriousness and certainty of the interaction:[14]
- Ciclosporin
- Coumarin anticoagulants, such as warfarin (reported rarely, but is serious when it occurs)
- Vidarabine
- Chlorpropamide
- Phenytoin
- Theophylline
- Cyclophosphamide, doxorubicin, bleomycin, procarbazine, mechlorethamine
Co-administration of the following drugs may make allopurinol less active or decrease its half-life:[14]
- Salicylates and medicines that increase the secretion of uric acid
- furosemide (see more on diuretics below)
Co-administration of the following drugs may cause hypersensitivity or skin rash:[14]
- Ampicillin and amoxicillin
- Diuretics, in particular thiazides, especially in renal impairment
- Angiotensin-converting-enzyme inhibitors (ACE inhibitors)
Pharmacology
A common misconception is that allopurinol is metabolized by its target, xanthine oxidase, but this action is principally carried out by aldehyde oxidase.[25] The active metabolite of allopurinol is oxipurinol, which is also an inhibitor of xanthine oxidase. Allopurinol is almost completely metabolized to oxipurinol within two hours of oral administration, whereas oxipurinol is slowly excreted by the kidneys over 18–30 hours. For this reason, oxipurinol is believed responsible for the majority of allopurinol's effect.[26]
Mechanism of action
Allopurinol is a purine analog; it is a structural isomer of hypoxanthine (a naturally occurring purine in the body) and is an inhibitor of the enzyme xanthine oxidase.[2] Xanthine oxidase is responsible for the successive oxidation of hypoxanthine and xanthine, resulting in the production of uric acid, the product of human purine metabolism.[2] In addition to blocking uric acid production, inhibition of xanthine oxidase causes an increase in hypoxanthine and xanthine. While xanthine cannot be converted to purine ribotides, hypoxanthine can be salvaged to the purine ribotides adenosine and guanosine monophosphates. Increased levels of these ribotides may cause feedback inhibition of amidophosphoribosyl transferase, the first and rate-limiting enzyme of purine biosynthesis. Allopurinol, therefore, decreases uric acid formation and may also inhibit purine synthesis.[27]
Pharmacogenetics
The HLA-B*5801 allele is a genetic marker for allopurinol-induced severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN).[28][29] The frequency of the HLA-B*5801 allele varies between ethnicities: Han Chinese and Thai populations have HLA-B*5801 allele frequencies of around 8%, as compared to European and Japanese populations, who have allele frequencies of around 1.0% and 0.5%, respectively.[30] The increase in risk for developing allopurinol-induced SJS or TEN in individuals with the HLA-B*5801 allele (as compared to those who do not have this allele) is very high, ranging from a 40-fold to a 580-fold increase in risk, depending on ethnicity.[28][29] As of 2011 the FDA-approved drug label for allopurinol did not contain any information regarding the HLA-B*5801 allele, though FDA scientists did publish a study in 2011 which reported a strong, reproducible and consistent association between the allele and allopurinol-induced SJS and TEN.[31] However, the American College of Rheumatology recommends screening for HLA-B*5801 in high-risk populations (e.g. Koreans with stage 3 or worse chronic kidney disease and those of Han Chinese and Thai descent), and prescribing patients who are positive for the allele an alternative drug.[32] The Clinical Pharmacogenetics Implementation Consortium Archived 20 July 2014 at the Wayback Machine guidelines state that allopurinol is contraindicated in known carriers of the HLA-B*5801 allele.[33][34]
History
Allopurinol was first synthesized and reported in 1956 by Roland K. Robins (1926-1992), in a search for antineoplastic agents.[2][35] Because allopurinol inhibits the breakdown (catabolism) of the thiopurine drug mercaptopurine, and it was later tested by Wayne Rundles, in collaboration with Gertrude Elion's lab at Wellcome Research Laboratories to see if it could improve treatment of acute lymphoblastic leukemia by enhancing the action of mercaptopurine.[2][36] However, no improvement in leukemia response was noted with mercaptopurine-allopurinol co-therapy, so that work turned to other compounds and the team then started testing allopurinol as a potential for gout.[37] Allopurinol was first marketed as a treatment for gout in 1966.[36]
Society and culture
Formulations
Allopurinol is sold as an injection for intravenous use[16] and as a tablet.[14]
Brands
Allopurinol has been marketed in the United States since August 19, 1966, when it was first approved by FDA under the trade name Zyloprim.[38] Allopurinol was marketed at the time by Burroughs Wellcome. Allopurinol is a generic drug sold under a variety of brand names, including Allohexal, Allosig, Milurit, Alloril, Progout, Ürikoliz, Zyloprim, Zyloric, Zyrik, and Aluron.[39]
See also
- Lesinurad/allopurinol, a fixed-dose combination drug
References
- 1 2 3 4 5 6 7 8 "Allopurinol". The American Society of Health-System Pharmacists. Archived from the original on 29 April 2016. Retrieved 8 December 2016.
- 1 2 3 4 5 6 Pacher P, Nivorozhkin A, Szabó C (March 2006). "Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol". Pharmacological Reviews. 58 (1): 87–114. doi:10.1124/pr.58.1.6. PMC 2233605. PMID 16507884.
- 1 2 3 "Allopurinol Use During Pregnancy". Drugs.com. Archived from the original on 20 August 2016. Retrieved 20 December 2016.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 19 September 2020. Retrieved 17 September 2020.
- 1 2 3 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 1183. ISBN 978-0-85711-369-6.
- 1 2 World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 39. hdl:10665/44053. ISBN 9789241547659.
- 1 2 Robinson PC, Stamp LK (May 2016). "The management of gout: Much has changed". Australian Family Physician. 45 (5): 299–302. PMID 27166465.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ Hitchings, Andrew; Lonsdale, Dagan; Burrage, Daniel; Baker, Emma (2019). The Top 100 Drugs: Clinical Pharmacology and Practical Prescribing (2nd ed.). Elsevier. pp. 42–43. ISBN 978-0-7020-7442-4. Archived from the original on 22 May 2021. Retrieved 9 November 2021.
- ↑ "Allopurinol". International Drug Price Indicator Guide. Archived from the original on 22 January 2018. Retrieved 8 December 2016.
- ↑ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 465. ISBN 9781284057560.
- ↑ "The Top 300 of 2020". ClinCalc. Archived from the original on 18 March 2020. Retrieved 11 April 2020.
- ↑ "Allopurinol - Drug Usage Statistics". ClinCalc. Archived from the original on 13 April 2020. Retrieved 11 April 2020.
- 1 2 3 4 5 6 7 "300 mg Allopurinol tables". UK Electronic Medicines Compendium. 7 April 2016. Archived from the original on 11 September 2016.
- ↑ Jeha S (October 2001). "Tumor lysis syndrome". Seminars in Hematology. 38 (4 Suppl 10): 4–8. doi:10.1016/S0037-1963(01)90037-X. PMID 11694945.
- 1 2 "Label for injectable Allopurinol". DailyMed. June 2014. Archived from the original on 13 September 2016.
- ↑ Bradford K, Shih DQ (October 2011). "Optimizing 6-mercaptopurine and azathioprine therapy in the management of inflammatory bowel disease". World Journal of Gastroenterology. 17 (37): 4166–73. doi:10.3748/wjg.v17.i37.4166. PMC 3208360. PMID 22072847.
- ↑ Sparrow MP, Hande SA, Friedman S, Cao D, Hanauer SB (February 2007). "Effect of allopurinol on clinical outcomes in inflammatory bowel disease nonresponders to azathioprine or 6-mercaptopurine". Clinical Gastroenterology and Hepatology. 5 (2): 209–14. doi:10.1016/j.cgh.2006.11.020. PMID 17296529.
- ↑ Ansari A, Patel N, Sanderson J, O'Donohue J, Duley JA, Florin TH (March 2010). "Low-dose azathioprine or mercaptopurine in combination with allopurinol can bypass many adverse drug reactions in patients with inflammatory bowel disease". Alimentary Pharmacology & Therapeutics. 31 (6): 640–7. doi:10.1111/j.1365-2036.2009.04221.x. PMID 20015102.
- ↑ Ansari AR, Duley JA (March 2012). "Azathioprine co-therapy with allopurinol for inflammatory bowel disease: trials and tribulations" (PDF). Rev Assoc Med Bras. 58 (Suppl.1): S28–33. Archived (PDF) from the original on 27 August 2021. Retrieved 11 September 2019.
- ↑ Dalbeth N, Stamp L (2007). "Allopurinol dosing in renal impairment: walking the tightrope between adequate urate lowering and adverse events". Seminars in Dialysis. 20 (5): 391–5. doi:10.1111/j.1525-139X.2007.00270.x. PMID 17897242.
- 1 2 3 4 Chung WH, Wang CW, Dao RL (July 2016). "Severe cutaneous adverse drug reactions". The Journal of Dermatology. 43 (7): 758–66. doi:10.1111/1346-8138.13430. PMID 27154258.
- ↑ Tsai TF, Yeh TY (2010). "Allopurinol in dermatology". American Journal of Clinical Dermatology. 11 (4): 225–32. doi:10.2165/11533190-000000000-00000. PMID 20509717.
- ↑ De Broe, Marc E.; Bennett, William M.; Porter, George A. (2003). Clinical Nephrotoxins: Renal Injury from Drugs and Chemicals. Springer Science+Business Media. ISBN 9781402012778. Archived from the original on 27 August 2021. Retrieved 3 June 2020.
Acute interstitial nephritis has also been reported associated with by the administration of allopurinol.
- ↑ Reiter S, Simmonds HA, Zöllner N, Braun SL, Knedel M (March 1990). "Demonstration of a combined deficiency of xanthine oxidase and aldehyde oxidase in xanthinuric patients not forming oxipurinol". Clinica Chimica Acta; International Journal of Clinical Chemistry. 187 (3): 221–34. doi:10.1016/0009-8981(90)90107-4. PMID 2323062.
- ↑ Day RO, Graham GG, Hicks M, McLachlan AJ, Stocker SL, Williams KM (2007). "Clinical pharmacokinetics and pharmacodynamics of allopurinol and oxypurinol". Clinical Pharmacokinetics. 46 (8): 623–44. doi:10.2165/00003088-200746080-00001. PMID 17655371.
- ↑ Cameron JS, Moro F, Simmonds HA (February 1993). "Gout, uric acid and purine metabolism in paediatric nephrology". Pediatric Nephrology. 7 (1): 105–18. doi:10.1007/BF00861588. PMID 8439471.
- 1 2 "Uric Acid-Lowering Drugs Pathway, Pharmacodynamics". PharmGKB. Archived from the original on 8 August 2014.
- 1 2 "PharmGKB". Archived from the original on 8 August 2014. Retrieved 1 August 2014.
- ↑ "Allele Frequency Net Database". Archived from the original on 28 August 2009.
- ↑ Zineh I, Mummaneni P, Lyndly J, Amur S, La Grenade LA, Chang SH, et al. (December 2011). "Allopurinol pharmacogenetics: assessment of potential clinical usefulness". Pharmacogenomics. 12 (12): 1741–9. doi:10.2217/pgs.11.131. PMID 22118056. Archived (PDF) from the original on 27 August 2021. Retrieved 3 June 2020.
- ↑ Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, et al. (October 2012). "2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia". Arthritis Care & Research. 64 (10): 1431–46. doi:10.1002/acr.21772. PMC 3683400. PMID 23024028.
- ↑ "Annotation of CPIC Guideline for allopurinol and HLA-B". PharmGKB. Archived from the original on 8 August 2014. Retrieved 1 August 2014.
- ↑ Hershfield MS, Callaghan JT, Tassaneeyakul W, Mushiroda T, Thorn CF, Klein TE, Lee MT (February 2013). "Clinical Pharmacogenetics Implementation Consortium guidelines for human leukocyte antigen-B genotype and allopurinol dosing". Clinical Pharmacology and Therapeutics. 93 (2): 153–8. doi:10.1038/clpt.2012.209. PMC 3564416. PMID 23232549.
- ↑ Robins RK (1956). "Potential Purine Antagonists. I. Synthesis of Some 4,6-Substituted Pyrazolo \3,4-d] pyrimidines1". J. Am. Chem. Soc. 78 (4): 784–790. doi:10.1021/ja01585a023.
- 1 2 Sneader, Walter (2005). Drug Discovery: A History. John Wiley & Sons. p. 254. ISBN 9780471899792. Archived from the original on 10 June 2016. Retrieved 4 September 2015.
- ↑ Elion GB (April 1989). "The purine path to chemotherapy". Science. 244 (4900): 41–7. Bibcode:1989Sci...244...41E. doi:10.1126/science.2649979. PMID 2649979.
- ↑ "FDA Approved Drug Products". Drugs@FDA. Archived from the original on 14 August 2012. Retrieved 8 November 2013.
- ↑ "Search Results for Allopurinol". DailyMed. Archived from the original on 25 March 2012. Retrieved 27 July 2011.
External links
| External sites: |
|
|---|---|
| Identifiers: |
- Allopurinol pathway on PharmGKB Archived 8 August 2014 at the Wayback Machine
- Dean L (March 2016). "Allopurinol Therapy and HLA-B*58:01 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520356. Archived from the original on 26 October 2020. Retrieved 15 April 2020.