Pentoxifylline
 | |
 | |
| Names | |
|---|---|
| Pronunciation | /ˌpɛntɒkˈsɪfɪliːn, -ɪn/ |
| Trade names | Pentoxil, Trental, others[1] |
| Other names | Oxpentifylline (former AAN)[2] |
IUPAC name
| |
| Clinical data | |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a685027 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 10–30%[3] |
| Metabolism | Liver and via erythrocytes |
| Elimination half-life | 0.4–0.8 hours (1–1.6 hours for active metabolite)[3] |
| Excretion | Urine (95%), faeces (<4%)[3] |
| Chemical and physical data | |
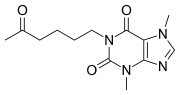
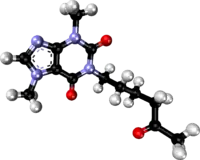
| Formula | C13H18N4O3 |
| Molar mass | 278.312 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Pentoxifylline, also known as oxpentifylline, is a medication used to treat peripheral artery disease that results in pain with walking and venous leg ulcers.[4] There is tentative evidence that it may improve peoples ability to walk.[5] Use is not recommended in the United Kingdom.[4] It is taken by mouth.[6]
Common side effects include nausea, dizziness, and heart burn.[6] Other side effects may include bleeding.[4] It is a xanthine derivative and is believed to work by increasing red blood cell flexibility.[6]
Pentoxifylline was approved for medical use in the United States in 1984.[6] It is available as a generic medication.[6] In the United Kingdom it costs the NHS about £19 a month as of 2021.[4] This amount in the United States is about 36 USD.[7]
Medical uses
Its primary use to try to reduce pain, cramping, numbness, or weakness in legs due to intermittent claudication, a form of muscle pain resulting from peripheral artery diseases.[5]
It may also be used off-label as an adjunct to compression bandaging for chronic venous leg ulcers.[8][9]
Pentoxifylline has been tested for use in sarcoidosis as an alternative or compliment to prednisone and other steroids, as the drug can inhibit excess levels of TNF-a, which is associated with granuloma formation.[10][11][12]
Dosage
It is taken at a dose of 400 mg two to three times per day.[4]
Side effects
Common side effects are belching, bloating, stomach discomfort or upset, nausea, vomiting, indigestion, dizziness, and flushing. Uncommon and rare side effects include angina, palpitations, hypersensitivity, itchiness, rash, hives, bleeding, hallucinations, arrhythmias, and aseptic meningitis.[2][3][13][14]
Contraindications include intolerance to pentoxifylline or other xanthine derivatives, recent retinal or cerebral haemorrhage, and risk factors for haemorrhage.[3]
Mechanism
Like other methylated xanthine derivatives, pentoxifylline is a competitive nonselective phosphodiesterase inhibitor[15] which raises intracellular cAMP, activates PKA, inhibits TNF[16][17] and leukotriene[18] synthesis, and reduces inflammation and innate immunity.[18] In addition, pentoxifylline improves red blood cell deformability (known as a haemorrheologic effect), reduces blood viscosity and decreases the potential for platelet aggregation and blood clot formation.[19] Pentoxifylline is also an antagonist at adenosine 2 receptors.[20]
Society and culture
Intermittent claudication is its only FDA, MHRA and TGA-labelled indication.[2][13][14]
Research
There is some evidence that pentoxifylline can lower the levels of some biomarkers in non-alcoholic steatohepatitis but evidence is insufficient to determine if the drug is safe and effective for this use.[21] Animal studies have been conducted exploring the use of pentoxifylline for erectile dysfunction[22] and hearing loss.[23] Human studies have been conducted for Peyronie's disease.[24]
Pentoxifylline, in combination with tocopherol and clodronate, has been found to heal refractory osteoradionecrosis of the jaw,[25] and to be prophylactic against osteoradionecrosis.[26]
In a Cochrane systematic review on the use of pentoxifylline for intermittent claudication in 2015, the following was concluded "The quality of included studies was generally low, and very large variability between studies was noted in reported findings including duration of trials, doses of pentoxifylline and distances participants could walk at the start of trials. Most included studies did not report on randomisation techniques or how treatment allocation was concealed, did not provide adequate information to permit judgement of selective reporting and did not report blinding of outcome assessors. Given all these factors, the role of pentoxifylline in intermittent claudication remains uncertain, although this medication was generally well tolerated by participants".[27]
See also
- Lisofylline, an active metabolite of pentoxifylline
- Propentofylline
- Cilostazol, a PDE-3 inhibitor with better evidence for intermittent claudication on the Cochrane review cited above.
References
- ↑ Drugs.com drugs.com international listings for Pentoxifylline Archived 2020-09-25 at the Wayback Machine. Page accessed Feb 1, 206
- 1 2 3 "PRODUCT INFORMATION TRENTAL® 400" (PDF). TGA eBusiness Services. sanofi-aventis australia pty limited. 25 March 2010. Archived from the original on 9 August 2017. Retrieved 3 February 2014.
- 1 2 3 4 5 "Trental, Pentoxil (pentoxifylline) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 4 February 2014. Retrieved 3 February 2014.
- 1 2 3 4 5 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 250. ISBN 978-0857114105.
- 1 2 Broderick, Cathryn; Forster, Rachel; Abdel-Hadi, Mohammed; Salhiyyah, Kareem (October 16, 2020). "Pentoxifylline for intermittent claudication". The Cochrane Database of Systematic Reviews. 10: CD005262. doi:10.1002/14651858.CD005262.pub4. ISSN 1469-493X. PMC 8094235. PMID 33063850.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - 1 2 3 4 5 "Pentoxifylline Monograph for Professionals". Drugs.com. Archived from the original on 18 June 2019. Retrieved 27 October 2021.
- ↑ "Pentoxifylline Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 20 January 2021. Retrieved 27 October 2021.
- ↑ SIGN (2010) Management of chronic venous leg ulcers. Clinical guideline No. 120. Scottish Intercollegiate Guidelines Network. www.sign.ac.uk ISBN 978-1-905813-66-7
- ↑ Jull, Andrew B; Arroll, Bruce; Parag, Varsha; Waters, Jill (2012). "Pentoxifylline for treating venous leg ulcers". Cochrane Database of Systematic Reviews. 12: CD001733. doi:10.1002/14651858.CD001733.pub3. ISSN 1465-1858. PMC 7061323. PMID 23235582.
- ↑ Zabel P, Entzian P, Dalhoff K, Schlaak M. Pentoxifylline in treatment of sarcoidosis. Am J Respir Crit Care Med. 1997 May;155(5):1665-9. doi: 10.1164/ajrccm.155.5.9154873. PMID: 9154873
- ↑ Park MK, Fontana Jr, Babaali H, Gilbert-McClain LI, Stylianou M, Joo J, Moss J, Manganiello VC. Steroid-sparing effects of pentoxifylline in pulmonary sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2009 Jul;26(2):121-31. PMID: 20560292; PMCID: PMC2946799.
- ↑ Tong Z, Dai H, Chen B, Abdoh Z, Guzman J, Costabel U. Inhibition of cytokine release from alveolar macrophages in pulmonary sarcoidosis by pentoxifylline: comparison with dexamethasone. Chest. 2003 Oct;124(4):1526-32. doi: 10.1378/chest.124.4.1526. PMID: 14555589.
- 1 2 "PENTOXIFYLLINE tablet, extended release [Apotex Corp.]". DailyMed. Apotex Corp. February 2013. Archived from the original on 19 February 2014. Retrieved 3 February 2014.
- 1 2 "Trental 400 - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Sanofi. 10 October 2013. Archived from the original on 19 February 2014. Retrieved 3 February 2014.
- ↑ Essayan DM (2001). "Cyclic nucleotide phosphodiesterases". The Journal of Allergy and Clinical Immunology. 108 (5): 671–80. doi:10.1067/mai.2001.119555. PMID 11692087.
- ↑ Deree J, Martins JO, Melbostad H, Loomis WH, Coimbra R (2008). "Insights into the regulation of TNF-alpha production in human mononuclear cells: the effects of non-specific phosphodiesterase inhibition". Clinics. 63 (3): 321–8. doi:10.1590/S1807-59322008000300006. PMC 2664230. PMID 18568240.
- ↑ Marques LJ, Zheng L, Poulakis N, Guzman J, Costabel U (1999). "Pentoxifylline inhibits TNF-alpha production from human alveolar macrophages". American Journal of Respiratory and Critical Care Medicine. 159 (2): 508–11. doi:10.1164/ajrccm.159.2.9804085. PMID 9927365.
- 1 2 Peters-Golden M, Canetti C, Mancuso P, Coffey MJ (2005). "Leukotrienes: underappreciated mediators of innate immune responses". Journal of Immunology. 174 (2): 589–94. doi:10.4049/jimmunol.174.2.589. PMID 15634873.
- ↑ Ward A, Clissold SP (1987). "Pentoxifylline. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy". Drugs. 34 (1): 50–97. doi:10.2165/00003495-198734010-00003. PMID 3308412.
- ↑ Rodríguez-Morán M, Guerrero-Romero F (2008). "Efficacy of pentoxifylline in the management of microalbuminuria in patients with diabetes". Current Diabetes Reviews. 4 (1): 55–62. doi:10.2174/157339908783502343. PMID 18220696.
- ↑ Li W, Zheng L, Sheng C, Cheng X, Qing L, Qu S (2011). "Systematic review on the treatment of pentoxifylline in patients with non-alcoholic fatty liver disease". Lipids in Health and Disease. 10: 49. doi:10.1186/1476-511X-10-49. PMC 3088890. PMID 21477300.
- ↑ Anele, U. A.; Morrison, B. F.; Burnett, A. L. (2015). "Molecular pathophysiology of priapism: Emerging targets". Current Drug Targets. 16 (5): 474–83. doi:10.2174/1389450115666141111111842. PMC 4430197. PMID 25392014.
- ↑ Latoni, J.; Shivapuja, B.; Seidman, M. D.; Quirk, W. S. (May 1996). "Pentoxifylline maintains cochlear microcirculation and attenuates temporary threshold shifts following acoustic overstimulation". Acta Oto-Laryngologica. 116 (3): 388–94. doi:10.3109/00016489609137862. PMID 8790737.
- ↑ El-Sakka, A. I. (2011). "Reversion of penile fibrosis: Current information and a new horizon". Arab Journal of Urology. 9 (1): 49–55. doi:10.1016/j.aju.2011.03.013. PMC 4149188. PMID 26579268.
- ↑ Delanian, S., Chatel, C., Porcher, R., Depondt, J. and Lefaix, J.L., 2011. Complete restoration of refractory mandibular osteoradionecrosis by prolonged treatment with a pentoxifylline-tocopherol-clodronate combination (PENTOCLO): a phase II trial. International Journal of Radiation Oncology, Biology, Physics, 80(3), pp.832-839.
- ↑ Patel, V., Gadiwalla, Y., Sassoon, I., Sproat, C., Kwok, J. and McGurk, M., 2016. Prophylactic use of pentoxifylline and tocopherol in patients who require dental extractions after radiotherapy for cancer of the head and neck. British Journal of Oral and Maxillofacial Surgery, 54(5), pp.547-550.
- ↑ Salhiyyah, Kareem; Forster, Rachel; Senanayake, Eshan; Abdel-Hadi, Mohammed; Booth, Andrew; Michaels, Jonathan A (2015-09-29). "Pentoxifylline for intermittent claudication". Cochrane Database of Systematic Reviews. 9 (9): CD005262. doi:10.1002/14651858.cd005262.pub3. ISSN 1465-1858. PMC 6513423. PMID 26417854.
External links
| Identifiers: |
|---|
- Pentoxifylline MedlinePlus Drug Information Archived 2016-07-05 at the Wayback Machine