Ethinylestradiol/etonogestrel
.png.webp) Vaginal ring application (step 1) | |
| Combination of | |
|---|---|
| Ethinylestradiol | Estrogen |
| Etonogestrel | Progestogen |
| Names | |
| Trade names | NuvaRing, others |
| Clinical data | |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Vaginal (ring) |
| External links | |
| AHFS/Drugs.com | FDA Professional Drug Information |
| MedlinePlus | a604032 |
| Legal | |
| Legal status |
|
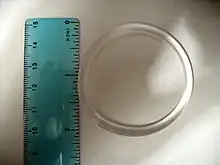
Ethinylestradiol/etonogestrel, sold under the brand names NuvaRing among others, is a hormonal vaginal ring used for birth control and to improve menstrual symptoms.[1] It contains ethinylestradiol, an estrogen, and etonogestrel, a progestin.[2] It is used by insertion into the vagina.[1] Pregnancy occurs in about 0.3% of women with perfect use and 9% of women with typical use.[3]
Common side effects include irregular vaginal bleeding, nausea, sore breasts, vaginitis, mood changes, and headache.[4] Rare but serious side effects may include blood clots, toxic shock syndrome, anaphylaxis, gallstones, and liver problems.[4] Use is not recommended in those who both smoke and are over the age of 35.[4] While use in pregnancy is not recommended, such use has not been found to be harmful to the baby.[4] Use during breastfeeding is typically not recommended as it may decrease the milk supply.[4] It mainly works by decreasing gonadotropins thereby stopping ovulation.[4]
The combination was approved for medical use in the United States in 2001.[2] It is on the World Health Organization's List of Essential Medicines.[5] It is available as a generic medication in the United Kingdom.[1] A month supply costs the UK's NHS £30 as of 2020.[1] In the United States the wholesale cost of this amount is about US$470.[6] In 2017, it was the 177th most commonly prescribed medication in the United States, with more than three million prescriptions.[7][8] Lawsuits were filed in the US against Merck alleging it concealed health risks associated with the product.[9] These were settled for $100 million in 2014.[10]
Medical use
The ring is placed into the vagina for a three-week period, then removal of the ring for one week, during which the user will experience a menstrual period. The break week is comparable to the placebo week for combined oral birth control pills ("the Pill"), and the birth control effect is maintained during this period. Extended use regimens (seven-week, quarterly, or annual) involving back-to-back use of (2, 4, or 17) rings have been studied in clinical trials, but are not currently approved.[11][12][13]
Insertion of the ring is comparable to insertion of other vaginal rings. The muscles of the vagina keep NuvaRing securely in place, even during exercise or sex. Women can check the birth control ring periodically with their finger. In rare instances, NuvaRing may fall out during sexual intercourse, while straining before or during a bowel movement, or while removing a tampon.[14][15]
In the case of accidental expulsion, the manufacturer recommends rinsing the ring with lukewarm water before reinserting. If not done correctly, the risk of pregnancy is increased. Birth control efficacy is reduced if the ring is removed, accidentally expelled, or left outside of the vagina for more than three hours. If left outside of the vagina for more than three hours, the device is to be rinsed and reinserted immediately. If this occurs, the manufacturer recommends that a backup method of birth control be used until the ring has been used continuously for a subsequent seven days.[14][15]
Benefits
The benefits of the ring include:
- once-a-month self-administered use offering convenience, ease of use and privacy (most users and most partners do not feel the ring, and of those who do, most do not object to it)[16][17][18]
- lower estrogen exposure than with combined oral contraceptive pills or the contraceptive patch Ortho Evra.[16][19][20]
- a low incidence of estrogenic side effects such as nausea and breast tenderness[17][21]
- a low incidence of irregular bleeding despite its lower estrogen dose[17][21]
Contraindications
The contraceptive vaginal ring is contraindicated for a risk of blood clots. This is because it contains the hormone etonogestrel, the active metabolite of the prodrug desogestrel. It is a third-generation contraceptive.[9]
A study in the BMJ, with over 1.6 million women, found that users of vaginal rings with ethinylestradiol and etonogestrel have a 6.5 times increased risk of venous thrombosis compared to non-users.[22][23] Epidemiological studies have shown that oral contraceptives that contain desogestrel can increase the risk of blood clots (venous thrombosis) by 1.5 to 2.4 times the risk of second-generation oral contraceptives.[24] Second-generation oral contraceptives do not contain desogestrel. Hormones are released continuously from NuvaRing, thus peak and total estrogen and progestin doses are lower than with combined oral contraceptives, but what effect this has on the risk of blood clots has not been established.[15]
NuvaRing also has the cardiovascular contraindications associated with combined oral contraceptives, such as stroke and heart attack. These risks have been shown to be much greater if combined with other risk factors such as smoking, recent surgery, a history of cardiovascular disease, or women over 40 years old.[15]
NuvaRing should not be used while breastfeeding. The hormones may pass to the baby through the milk, and it may decrease milk production.[25]
Side effects
In two large studies, over a one-year period, 15.1% of users discontinued NuvaRing because of adverse events. Device-related adverse events (foreign object sensation, sexual problems, or expulsion) were the most frequently reported adverse events that resulted in discontinuation (by 2.5% of users). Device-related adverse events were reported at least once during the one-year study period by 4.4% of NuvaRing users.[17]
The most common adverse events reported by 5 to 14% of the 2501 women who used NuvaRing in five clinical trials were: vaginitis (14.1%), headache (9.8%), upper respiratory tract infection (8.0%), leukorrhea (5.8%), sinusitis (5.7%), nausea (5.2%), and weight gain (4.9%).[15][26][27] NuvaRing is weight neutral.[28][29] Additional side effect information (including, but not limited to, severe blood clots) is provided in the NuvaRing full prescribing information.[15][27] Breakthrough bleeding occurs in 2.0 to 6.4% of NuvaRing users.[30]
Blood clots
The vaginal ring with ethinylestradiol and etonogestrel increases the risk of venous blood clots 6.5 times compared to non-users of hormonal birth control.[22] This is similar to the risk of blood clots with combination birth control pills, which range between 3 times to 14 times the risk.[31] As such, birth control vaginal rings do not necessarily appear to pose a lower risk of thrombosis than do birth control pills.[22][31] Additionally pregnancy and the period immediately following pregnancy is associated with a high risk of blood clots.[4]
Mechanism of action
Like all combined hormonal contraceptives, NuvaRing works primarily by preventing ovulation. A secondary mechanism of action is inhibition of sperm penetration by changes in the cervical mucus. Hormonal contraceptives also have effects on the endometrium that theoretically could affect implantation, however no scientific evidence indicates that prevention of implantation actually results from their use.[32] NuvaRing should not be used if a woman is pregnant.
NuvaRing delivers 120 µg of etonogestrel (a progestin) and 15 µg of ethinylestradiol (an estrogen) each day of use.
Society and culture
Cost
A month supply costs the NHS in the UK £29.70 as of 2020.[1] In the United States the wholesale cost of this amount is about US$468.78.[6] In 2017, it was the 177th most commonly prescribed medication in the United States, with more than three million prescriptions.[7][8]
.svg.png.webp) Ethinylestradiol/etonogestrel costs (US)
Ethinylestradiol/etonogestrel costs (US).svg.png.webp) Ethinylestradiol/etonogestrel prescriptions (US)
Ethinylestradiol/etonogestrel prescriptions (US)
Restrictions on use
On July 31, 2014, CTV News reported that Merck Canada Inc. stated that women who are over 35 and smoke should not use the Nuvaring. In addition to this group of women, women who have any of the following conditions also should not use the Nuvaring: abnormal blood-fat levels, clotting disorders, diabetes, heart disease, high blood pressure, migraine headaches with vision problems or "constant stomach pain caused by pancreatic dysfunction along with high levels of fats in the blood".[33]
Lawsuits
In March 2008, the first lawsuit was filed against the manufacturers, distributors, and marketers of NuvaRing. The plaintiff alleged that these companies concealed the health risks associated with using the device, which is claimed to have caused the death of the plaintiff's wife.[34] Subsequent plaintiffs alleged multiple problems with the advertising of NuvaRing and that they downplayed its risks of injury and death.[35] The company denied these allegations.[35]
The first bellwether trial, selected from a pool of federal lawsuits, was scheduled to begin on April 7, 2014.[36] On February 6, 2014, however, Merck & Co announced that it was ready to settle the NuvaRing lawsuits for $100 million. At that time, there were more than 1,850[37] lawsuits and the settlement was initially estimated pay about $58,000 per complaint.[38] Approval of the settlement required 95% of the plaintiffs to agree to settle by the end of the day, March 10, 2014,[37] otherwise Merck could retract their offer.[39] On June 5, 2014 US District Judge Rodney W. Sippel approved the $100 million settlement. About 3,800 claimants would share the settlement.[40]
History
The first progestogen-releasing vaginal contraceptive was developed by the World Health Organization in the 1970s. High rates of menstrual problems led to the development of a vaginal ring which combined both progestogen and estrogen in 1978. NV Organon of the Netherlands developed a ring containing etonogestrel in the early 1990s, which led to the combined NuvaRing.[41] NuvaRing was first approved in The Netherlands in February 2001, then by all 14 other countries then in the European Union in June, and in the United States by the U.S. Food and Drug Administration (FDA) in October of the same year.[41][42] NuvaRing was first marketed in the United States in July 2002,[41] followed by a number European countries since then.[41]
In March 2007, Organon announced the market launch of NuvaRing in Australia, bringing the total number of countries where NuvaRing is available to 32. A study by Danish researcher Dr. Øjvind Lidegaard in 2012 with 1.6 million women found a 6.5 times increase in the likelihood of venous thromboembolism when compared to users of non-hormonal based birth control. In Canada, Lidegaard's study led to a change in labeling warning of increased risk of blood clots, but not in the United States.[23]
See also
References
- 1 2 3 4 5 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 843-844. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - 1 2 "Ethinyl Estradiol and Etonogestrel (Professional Patient Advice)". Drugs.com. Archived from the original on 20 April 2021. Retrieved 19 April 2019.
- ↑ Trussell, James (2011). "Contraceptive efficacy". In Hatcher, Robert A.; Trussell, James; et al. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States. Archived 2013-11-12 at the Wayback Machine
- 1 2 3 4 5 6 7 "NuvaRing - FDA prescribing information, side effects and uses". Drugs.com. Archived from the original on 4 May 2021. Retrieved 19 April 2019.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- 1 2 "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Archived from the original on 2019-03-06. Retrieved 3 March 2019.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- 1 2 "Ethinyl Estradiol; Etonogestrel - Drug Usage Statistics". ClinCalc. Archived from the original on 18 January 2021. Retrieved 11 April 2020.
- 1 2 Mencimer, Stephanie (2009). "Is NuvaRing Dangerous?". Mother Jones. Archived from the original on 22 January 2021. Retrieved 30 June 2013.
- ↑ "Merck to Dole Out $100 Million in NuvaRing Settlement". Time. 7 February 2014. Archived from the original on 18 January 2021. Retrieved 19 April 2019.
- ↑ Organon (September 15, 2005). "NuvaRing is effective and well tolerated in extended use - Most women would like to decrease their number of periods a year". Archived from the original on October 18, 2006. Retrieved 2007-04-12.
- ↑ Miller L, Verhoeven CH, Hout J (2005). "Extended regimens of the contraceptive vaginal ring: a randomized trial". Obstet Gynecol. 106 (3): 473–82. doi:10.1097/01.AOG.0000175144.08035.74. PMID 16135576.
- ↑ Barreiros FA, Guazzelli CA, de Araujo FF, Barbosa R (2007). "Bleeding patterns of women using extended regimens of the contraceptive vaginal ring". Contraception. 75 (3): 204–8. doi:10.1016/j.contraception.2006.10.009. PMID 17303490.
- 1 2 Organon. "NuvaRing: Common Questions: Will NuvaRing fall out?". Archived from the original on 2012-07-06. Retrieved 2009-07-06.
- 1 2 3 4 5 6 Organon (August 2005). "NuvaRing - US Prescribing Information" (PDF). Archived from the original (PDF) on 2007-03-23. Retrieved 2007-04-12.
- 1 2 Hatcher, Robert A.; Nelson, Anita (2004). "Combined Hormonal Contraceptive Methods". In Hatcher, Robert A.; et al. (eds.). Contraceptive Technology (18th rev. ed.). New York: Ardent Media. pp. 391–460. ISBN 978-0-9664902-5-1.
- 1 2 3 4 Dieben TO, Roumen FJ, Apter D (2002). "Efficacy, cycle control, and user acceptability of a novel combined contraceptive vaginal ring". Obstet Gynecol. 100 (3): 585–93. doi:10.1016/S0029-7844(02)02124-5. PMID 12220783.
- ↑ Organon. "NuvaRing: Questions patients may have: Will my partner or I feel NuvaRing?". Archived from the original on 2007-02-25. Retrieved 2007-07-16.
- ↑ Organon. "NuvaRing: Knowing the benefits: Low dose of hormones". Archived from the original on 2006-11-18. Retrieved 2007-04-12.
- ↑ van den Heuvel MW, van Bragt AJ, Alnabawy AK, Kaptein MC (2005). "Comparison of ethinylestradiol pharmacokinetics in three hormonal contraceptive formulations: the vaginal ring, the transdermal patch and an oral contraceptive". Contraception. 72 (3): 168–74. doi:10.1016/j.contraception.2005.03.005. PMID 16102549.
- 1 2 Speroff, Leon; Darney, Philip D. (2005). "Vaginal and Transdermal Estrogen-Progestin Contraception". A Clinical Guide for Contraception (4th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 153–164. ISBN 978-0-7817-6488-9.
- 1 2 3 Lidegaard, Øjvin; Øjvind Lidegaard; Lars Hougaard Nielsen; Charlotte Wessel Skovlund; Ellen Løkkegaard (May 2012). "Venous thrombosis in users of non-oral hormonal contraception: follow-up study, Denmark 2001-10". BMJ. 344: e2990. doi:10.1136/bmj.e2990. PMC 3349780. PMID 22577198. Archived from the original on 29 October 2013. Retrieved 30 June 2013.
- 1 2 Sabrina, Siddiqui (2013-12-18). "Side Effects May Include Death: The Story Of The Biggest Advance In Birth Control Since The Pill". The Huffington Post. Archived from the original on 2013-12-18. Retrieved 19 December 2013.
- ↑ Marie B. Walker & Henry I. Bussey, Pharm.D., FCCP, FAHA (2007). "Should 3rd Generation Birth Control Pills be Banned? - Petition to Ban 3rd Generation OCs due to Increased Clotting Risk". Archived from the original on 2008-09-13. Retrieved 2008-09-30.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ↑ "emedtv.com". Archived from the original on 2016-03-04. Retrieved 2016-12-28.
- ↑ FDA (2001). "NuvaRing NDA 21-187 Medical Review Part 2" (PDF). pp. 51, 53. Archived from the original (PDF) on 2007-09-26. Retrieved 2007-09-14.
- 1 2 Organon. "NuvaRing: Questions patients may have: What are the side effects associated with NuvaRing?". Archived from the original on 2008-10-25. Retrieved 2007-09-14.
- ↑ Organon. "NuvaRing: Questions patients may have: Does NuvaRing cause weight gain?". Archived from the original on 2008-10-25. Retrieved 2007-09-14.
- ↑ Bjarnadóttir RI, Tuppurainen M, Killick SR (2002). "Comparison of cycle control with a combined contraceptive vaginal ring and oral levonorgestrel/ethinyl estradiol". Am J Obstet Gynecol. 186 (3): 389–195. doi:10.1067/mob.2002.121103. PMID 11904596.
- ↑ Review of the combined contraceptive vaginal ring, NuvaRing. Archived 2016-01-14 at the Wayback Machine by Frans Jme Roumen. Therapeutics and Clinical Risk Management 05/2008; 4(2):441-51.
- 1 2 Vlieg, A van Hylckama; F M Helmerhorst; J P Vandenbroucke; C J M Doggen; F R Rosendaal (August 2009). "The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study". BMJ. 339: b2921. doi:10.1136/bmj.b2921. PMC 2726929. PMID 19679614. Archived from the original on 24 December 2013. Retrieved 23 Dec 2013.
- ↑ Rivera R, Yacobson I, Grimes D (1999). "The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices". Am J Obstet Gynecol. 181 (5 Pt 1): 1263–9. doi:10.1016/S0002-9378(99)70120-1. PMID 10561657.
- ↑ The Canadian Press (31 July 2014). "NuvaRing maker advises some women to avoid using product". CTV News. Archived from the original on 10 August 2014. Retrieved 8 August 2014.
- ↑ Cotton, Mark (2008-03-20). "Schering-Plough, Akzo Nobel sued over NuvaRing contraceptive device". Thomson Financial News. Forbes.com. Archived from the original on 2008-03-30. Retrieved 2008-05-06.
- 1 2 Edwards, Jim (19 April 2014). "At Merck, an Undercover Video and 40 Deaths Plague Nuvaring Birth Control Brand". CBS News. Archived from the original on 5 June 2014. Retrieved 5 June 2014.
- ↑ "Case: 4:08-md-01967-RWS (Nuvaring Products Liability Litigation)" (PDF). Archived (PDF) from the original on 2014-03-09. Retrieved 22 November 2013.
- 1 2 "NuvaRing's $100 Million Settlement Deadling is Monday", The Detroit Free Press, March 9, 2014, page 9A
- ↑ "Merck to settle NuvaRing lawsuits for $100 mln -media report". Reuters. 6 February 2014. Archived from the original on 22 February 2014. Retrieved 7 February 2014.
- ↑ Feeley, Jef and David Voreacos (2014-02-07). "Merck to Pay $100 Million NuvaRing Pact If Women Join". Thomson Financial News. Forbes.com. Archived from the original on 2014-02-07. Retrieved 2014-02-06.
- ↑ Salter, Jim (5 June 2014). "$100 Million NuvaRing Settlement Finalized". ABC News. Archived from the original on 5 June 2014. Retrieved 5 June 2014.
- 1 2 3 4 Mandelbaum, Rachel S.; Shoupe, Donna (2020). "The Contraceptive Vaginal Ring". The Handbook of Contraception: Evidence Based Practice Recommendations and Rationales. Humana Press: 73–96. doi:10.1007/978-3-030-46391-5_5. Archived from the original on 2021-08-28. Retrieved 2021-02-22.
- ↑ Lenobel, Dana (2021). Geyer, Jane; Dietrich, Jennifer (eds.). NASPAG’s Protocols for Pediatric and Adolescent Gynecology: A Ready-Reference Guide for Nurses. Springer Publishing Company. pp. 29–38. ISBN 978-0-8261-5194-0. Archived from the original on 2021-08-28. Retrieved 2021-02-22.
External links
| Identifiers: |
|---|
- FDA safety information on NuvaRing Archived 2009-05-21 at the Wayback Machine
- DrugLib.com - NuvaRing prescribing information, published studies, current trials Archived 2016-12-29 at the Wayback Machine
- Estrogen-Progestin Combinations by AHFS Archived 2016-12-23 at the Wayback Machine