Menstruation
Menstruation, also known as a period or monthly,[1] is the regular discharge of blood and mucosal tissue (known as menses) from the inner lining of the uterus through the vagina.[2] The first period usually begins between twelve and fifteen years of age, a point in time known as menarche.[1] However, periods may occasionally start as young as eight years old and still be considered normal.[2] The average age of the first period is generally later in the developing world, and earlier in the developed world.[3] The typical length of time between the first day of one period and the first day of the next is 21 to 45 days in young women, and 21 to 31 days in adults (an average of 28 days).[2][3] Bleeding usually lasts around 2 to 7 days.[2] Menstruation stops occurring after menopause, which usually occurs between 45 and 55 years of age.[4] Periods also stop during pregnancy and typically do not resume during the initial months of breastfeeding.[2]
Up to 80% of women report having some symptoms prior to menstruation.[5] Common signs and symptoms include acne, tender breasts, bloating, feeling tired, irritability, and mood changes.[6] These may interfere with normal life, therefore qualifying as premenstrual syndrome, in 20 to 30% of women.[5] In 3 to 8%, symptoms are severe.[5]
A lack of periods, known as amenorrhea, is when periods do not occur by age 15 or have not occurred in 90 days.[2] Other problems with the menstrual cycle include painful periods and abnormal bleeding such as bleeding between periods or heavy bleeding.[2] Menstruation in other animals occur in primates (apes and monkeys).[7][8]
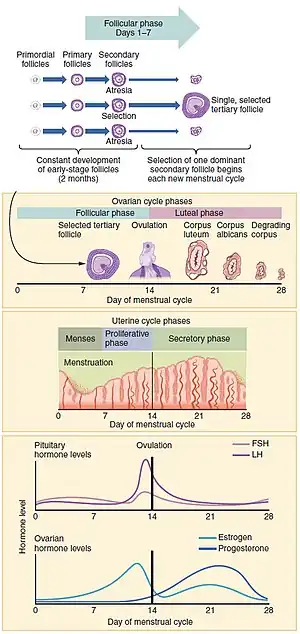
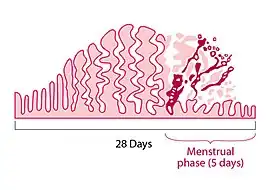
The menstrual cycle occurs due to the rise and fall of hormones.[2] This cycle results in the thickening of the lining of the uterus, and the growth of an egg, (which is required for pregnancy).[2] The egg is released from an ovary around day fourteen in the cycle; the thickened lining of the uterus provides nutrients to an embryo after implantation.[2] If implantation does not occur, the lining is released in what is known as menstruation.[2]
Onset and frequency
The first menstrual period occurs after the onset of pubertal growth, and is called menarche. The average age of menarche is 12 to 15.[1][9] However, it may start as early as eight.[2] The average age of the first period is generally later in the developing world, and earlier in the developed world.[3] The average age of menarche has changed little in the United States since the 1950s.[3]
Menstruation is the most visible phase of the menstrual cycle and its beginning is used as the marker between cycles. The first day of menstrual bleeding is the date used for the last menstrual period (LMP). The typical length of time between the first day of one period and the first day of the next is 21 to 45 days in young women, and 21 to 31 days in adults.[2][3] The average length is 28 days; one study estimated it at 29.3 days.[10]
Perimenopause is when fertility in a female declines, and menstruation occurs less regularly in the years leading up to the final menstrual period, when a female stops menstruating completely and is no longer fertile. The medical definition of menopause is one year without a period and typically occurs between 45 and 55 in Western countries.[4][11]: p. 381
During pregnancy and for some time after childbirth, menstruation does not occur. The average length of postpartum amenorrhoea is longer when breastfeeding; this is termed lactational amenorrhoea.
Health effects
In most women, various physical changes are brought about by fluctuations in hormone levels during the menstrual cycle. This includes muscle contractions of the uterus (menstrual cramping) that can precede or accompany menstruation. Some may notice bloating, changes in sex drive, fatigue, breast tenderness, headaches, or irritability before the onset of their period.[12][13][14] It is unclear if the breast discomfort and bloating is related to electrolyte changes or water retention.[15] Some women have mild or no symptoms before the onset of their periods.[13] A healthy diet, reduced consumption of salt, caffeine and alcohol, and regular exercise may be effective for women in controlling water retention.[16] Severe symptoms that disrupt daily activities and functioning may be diagnosed as premenstrual dysphoric disorder.[13]
Cramps
Many women experience painful cramps, also known as dysmenorrhea, during menstruation.[17]
Painful menstrual cramps that result from an excess of prostaglandin release are referred to as primary dysmenorrhea. Primary dysmenorrhea usually begins within a year or two of menarche, typically with the onset of ovulatory cycles.[18] Treatments that target the mechanism of pain include non-steroidal anti-inflammatory drugs (NSAIDs) and hormonal contraceptives. NSAIDs inhibit prostaglandin production. With long-term treatment, hormonal birth control reduces the amount of uterine fluid/tissue expelled from the uterus. Thus resulting in shorter, less painful menstruation.[19] These drugs are typically more effective than treatments that do not target the source of the pain (e.g. acetaminophen).[20] Risk factors for primary dysmenorrhea include: early age at menarche, long or heavy menstrual periods, smoking, and a family history of dysmenorrhea.[18] Regular physical activity may limit the severity of uterine cramps.[18]
For many women, primary dysmenorrhea gradually subsides in late second generation. Pregnancy has also been demonstrated to lessen the severity of dysmenorrhea, when menstruation resumes. However, dysmenorrhea can continue until menopause. 5–15% of women with dysmenorrhea experience symptoms severe enough to interfere with daily activities.[18]
Secondary dysmenorrhea is the diagnosis given when menstruation pain is a secondary cause to another disorder. Conditions causing secondary dysmenorrhea include endometriosis, uterine fibroids, and uterine adenomyosis. Rarely, congenital malformations, intrauterine devices, certain cancers, and pelvic infections cause secondary dysmenorrhea.[18] If the pain occurs between menstrual periods, lasts longer than the first few days of the period, or is not adequately relieved by the use of non-steroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives, women should be evaluated for secondary causes of dysmenorrhea.[11]: p. 379
When severe pelvic pain and bleeding suddenly occur or worsen during a cycle, the woman or girl should be evaluated for ectopic pregnancy and spontaneous abortion. This evaluation begins with a pregnancy test and should be done as soon as unusual pain begins, because ectopic pregnancies can be life‑threatening.[21]
In some cases, stronger physical and emotional or psychological sensations may interfere with normal activities, and include menstrual pain (dysmenorrhea), migraine headaches, and depression. Dysmenorrhea, or severe uterine pain, is particularly common for young females (one study found that 67.2% of girls aged 13–19 have it).[22]
Mood and behavior
Some women experience emotional disturbances starting one or two weeks before their period, and stopping within a few days of the period starting.[6][23] Symptoms may include mental tension, irritability, mood swings, and crying spells. Problems with concentration and memory may occur.[6] There may also be depression or anxiety.[6]
These symptoms can be severe enough to impact a person's performance at work, school, and in every day activities. Greater loss in workplace productivity, quality of life, and greater healthcare costs occur in those with moderate to severe symptoms in comparison to those without these symptoms.[24]
This is part of premenstrual syndrome (PMS) and is estimated to occur in 20 to 30% of women.[5] In 3 to 8% it is severe.[5]
More severe symptoms of anxiety or depression may be signs of premenstrual dysphoric disorder (PMDD). This disorder is listed in the DSM-5 as a depressive disorder.[24] Rarely, in individuals who are susceptible, menstruation may be a trigger for menstrual psychosis.
Extreme psychological stress can also result in periods stopping.[25]
Bleeding
The average volume of menstrual fluid during a monthly menstrual period is 35 milliliters (2.4 tablespoons of menstrual fluid) with 10–80 milliliters (1–6 tablespoons of menstrual fluid) considered typical. Menstrual fluid is the correct name for the flow, although many people prefer to refer to it as menstrual blood. Menstrual fluid is reddish-brown, a slightly darker color than venous blood.[11]: p. 381
About half of menstrual fluid is blood. This blood contains sodium, calcium, phosphate, iron, and chloride, the extent of which depends on the woman. As well as blood, the fluid consists of cervical mucus, vaginal secretions, and endometrial tissue. Vaginal fluids in menses mainly contribute water, common electrolytes, organ moieties, and at least 14 proteins, including glycoproteins.[26]
Many mature females notice blood clots during menstruation. These appear as clumps of blood that may look like tissue. If there are questions (for example, was there an miscarriage or an stillbirth?), examination under a microscope can confirm if it was endometrial tissue or pregnancy tissue (products of conception) that was shed.[27] Sometimes menstrual clots or shed endometrial tissue is incorrectly thought to indicate an early-term miscarriage of an embryo. An enzyme called plasmin – contained in the endometrium – tends to inhibit the blood from clotting.
The amount of iron lost in menstrual fluid is relatively small for most women.[28] In one study, premenopausal women who exhibited symptoms of iron deficiency were given endoscopies. 86% of them actually had gastrointestinal disease and were at risk of being misdiagnosed simply because they were menstruating.[29] Heavy menstrual bleeding, occurring monthly, can result in anemia.
Menstrual disorders
There is a wide spectrum of differences in how women experience menstruation. There are several ways that someone's menstrual cycle can differ from the norm, any of which should be discussed with a doctor to identify the underlying cause:
| Term | Meaning |
|---|---|
| Oligomenorrhea | Infrequent periods |
| Hypomenorrhea | Short or light periods |
| Polymenorrhea | Frequent periods (more frequently than every 21 days) |
| Hypermenorrhea | Heavy or long periods (soaking a sanitary napkin or tampon every hour, menstruating longer than 7 days) |
| Dysmenorrhea | Painful periods |
| Intermenstrual bleeding | Breakthrough bleeding (also called spotting) |
| Amenorrhea | Absent periods |
There is a movement among gynecologists to discard the terms noted above, which although they are widely used, do not have precise definitions. Many now argue to describe menstruation in simple terminology, including:
- Cycle regularity (irregular, regular, or absent)
- Frequency of menstruation (frequent, normal, or infrequent)
- Duration of menstrual flow (prolonged, normal, or shortened)
- Volume of menstrual flow (heavy, normal, or light)[30]
Dysfunctional uterine bleeding is a hormonally caused bleeding abnormality. Dysfunctional uterine bleeding typically occurs in premenopausal women who do not ovulate normally (i.e. are anovulatory). All these bleeding abnormalities need medical attention; they may indicate hormone imbalances, uterine fibroids, or other problems. As pregnant women may bleed, a pregnancy test forms part of the evaluation of abnormal bleeding.
Women who had undergone female genital mutilation (particularly type III- infibulation) a practice common in parts of Africa, may experience menstrual problems, such as slow and painful menstruation, that is caused by the near-complete sealing off of the vagina.[31]
Premature or delayed menarche should be investigated if menarche begins before 9 years, if menarche has not begun by age 15, if there is no breast development by age 13, or if there is no period by 3 years after the onset of breast development.[3]
Sexual activity
Sexual feelings and behaviors change during the menstrual cycle. Before and during ovulation, high levels of estrogen and androgens result in women having a relatively increased interest in sexual activity, and relatively lower interest directly prior to and during menstruation.[32] Unlike other mammals, women may show interest in sexual activity across all days of the menstrual cycle, regardless of fertility.[33]
There are no specific risks associated with sexual intercourse during menstruation, that are different than any other time during the menstrual cycle.[34][35]
Ovulation suppression
Birth control
Hormonal contraception affects the frequency, duration, severity, volume, and regularity of menstruation and menstrual symptoms.
The most common form of hormonal contraception is the combined birth control pill, which contains both estrogen and progestogen. It is typically taken in 28-day cycles, 21 hormonal pills with either a 7-day break from pills, or 7 placebo pills during which the woman menstruates. Although the primary function of the pill is to prevent pregnancy, it may be used to improve some menstrual symptoms and syndromes which affect menstruation, such as polycystic ovary syndrome (PCOS), endometriosis, adenomyosis, amenorrhea, menstrual cramps, menstrual migraines, menorrhagia (excessive menstrual bleeding), menstruation-related or fibroid-related anemia and dysmenorrhea (painful menstruation) by creating regularity in menstrual cycles and reducing overall menstrual flow.[36][37]
Using the combined birth control pill, it is also possible for a woman to delay or completely eliminate menstrual periods, a practice called menstrual suppression.[38] Some women do this simply for convenience in the short-term,[39] while others prefer to eliminate periods altogether when possible. This can be done either by skipping the placebo pills, or using an extended cycle combined oral contraceptive pill, which were first marketed in the U.S. in the early 2000s. This continuous administration of active pills without the placebo can lead to the achievement of amenorrhea in 80% of users within 1 year of use.[40]
Injections such as depo-provera (DMPA) became available in the 1960s and later became used to also achieve amenorrhea. A majority of patients will achieve amenorrhea within 1 year of initiating DMPA therapy. DMPA therapy is typically successful in achieving amenorrhea but also has side effects of decreased bone mineral density that must be considered before beginning therapy.[40]
Levonorgestrel intrauterine devices have also been used been shown to induce amenorrhea. The lower dose device has a lower rate of achieving amenorrhea compared to the higher dose device where 50% of users have been found to achieve amenorrhea within 1 year of use. A concern for usage of these devices is the invasive administration and initial breakthrough bleeding while utilizing these devices however they have the advantage of the most infrequent dosing schedule of every 5 years. Use of intrauterine devices have also shown to reduce menorrhagia and dysmenorrhea.[40][41]
When using the subdermal progestin only implants, unpredictable bleeding continues and amenorrhea is not commonly achieved amongst patients.[40]Progestogen-only contraceptive pills (sometimes called the 'mini pill') are taken continuously without a 7-day span of using placebo pills, and therefore menstrual periods are less likely to occur than with the combined pill with placebo pills. However, disturbance of the menstrual cycle is common with the mini-pill; 1/3-1/2 of women taking it will experience prolonged periods, and up to 70% experience break-through bleeding (metrorrhagia). Irregular and prolonged bleeding is the most common reason that women discontinue using the mini pill.[42]
History
When the first birth control pill was being developed, the researchers were aware that they could use the contraceptive to space menstrual periods up to 90 days apart, but they settled on a 28-day cycle that would mimic a natural menstrual cycle and produce monthly periods. The intention behind this decision was the hope of the inventor, John Rock, to win approval for his invention from the Roman Catholic Church. That attempt failed, but the 28-day cycle remained the standard when the pill became available to the public.[43]
There is debate among medical researchers about the potential long-term impacts of these practices upon female health. Some researchers point to the fact that historically, females have had far fewer menstrual periods throughout their lifetimes, a result of shorter life expectancies, as well as a greater length of time spent pregnant or breast-feeding, which reduced the number of periods experienced by females.[44] There is also the advantage of inducing menstrual suppression amongst people with extreme cognitive and physical disabilities who may not be able to properly manage their menstrual hygiene even with the use of a caregiver.[45] On the other hand, some researchers believe there is a greater potential for negative impacts from exposing females perhaps unnecessarily to regular low doses of synthetic hormones over their reproductive years.[46] There is limited evidence that the act of menstrual suppression directly causes physiologic harm and the primary disadvantages shown to be associated with menstrual suppression are due to side effects of the methods used to achieve amenorrhea.[40][45]
Breastfeeding
Breastfeeding causes negative feedback to occur on pulse secretion of gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH). Depending on the strength of the negative feedback, breastfeeding women may experience complete suppression of follicular development, follicular development but no ovulation, or normal menstrual cycles may resume.[47] Suppression of ovulation is more likely when suckling occurs more frequently.[48] The production of prolactin in response to suckling is important to maintaining lactational amenorrhea.[49] On average, women who are fully breastfeeding whose infants suckle frequently experience a return of menstruation at fourteen and a half months postpartum. There is a wide range of response among individual breastfeeding women, however, with some experiencing return of menstruation at two months and others remaining amenorrheic for up to 42 months postpartum.[50]
Menstrual management
Menstruating women manage menstruation primarily by wearing menstrual products such as tampons, napkins or menstrual cups. These products catch the menstrual blood to prevent it from staining and damaging clothing and inconveniencing the wearer. Menstruation can also be suppressed altogether through certain methods of birth control.[51]
Due to poverty, some cannot afford commercial feminine hygiene products.[52][53] Instead, they use materials found in the environment or other improvised materials. Absorption materials that may be used by women who cannot afford anything else include: sand, ash, small hole in earth,[54] cloth, whole leaf, leaf fiber (such as water hyacinth, banana, papyrus, cotton fibre), paper (toilet paper, re-used newspaper, brown paper bags, pulped and dried paper),[55] animal pelt (such as goat skin),[54] double layer of underwear, socks, skirt, or sari.[53][56]
Menstrual products
Menstrual products (also called "feminine hygiene" products) are made to absorb or catch menstrual blood. A number of different products are available - some are disposable, some are reusable. Where women can afford it, items used to absorb or catch menses are usually commercially manufactured products.
There are disposable products:


- Sanitary napkins (also called sanitary towels or pads) – Rectangular pieces of material worn attached to the underwear to absorb menstrual flow, often with an adhesive backing to hold the pad in place. Disposable pads may contain wood pulp or gel products, usually with a plastic lining and bleached.
- Tampons – Disposable cylinders of treated rayon/cotton blends or all-cotton fleece, usually bleached, that are inserted into the vagina to absorb menstrual flow.
- Disposable menstrual cups made of soft plastic – A firm, flexible cup-shaped device worn inside the vagina to collect menstrual flow.
Reusable products include:
- Menstrual cups – A firm, flexible bell-shaped device worn inside the vagina to collect menstrual flow. Menstrual cups are usually made of silicone and can last 5 years or longer.
- Reusable cloth pads – Pads that are made of cotton (often organic), terrycloth, or flannel, and may be handsewn (from material or reused old clothes and towels) or storebought.
- Padded panties or period-proof underwear – Reusable cloth (usually cotton) underwear with extra absorbent layers sewn in to absorb flow. Some also use patented technology to be leak resistant, such as the brand THINX.
- Sea sponges – Natural sponges, worn internally like a tampon to absorb menstrual flow.
- Blanket, towel – (also known as a draw sheet) – large reusable piece of cloth, most often used at night, placed between legs to absorb menstrual flow.
United States and the United Kingdom
Menstrual hygiene products are considered by many states within the United States as "tangible individual property" resulting in additional sales tax. This additional tax increases the overall price and further limits accessibility to menstrual hygiene products to lower income women. These products are classified as medical devices but are not eligible for purchase through government funded assistance programs.[57] The Scottish government have in 2019 begun providing free sanitary products for poorer students at schools, with hopes that this will be rolled out across the entire nation.[58][59]
Lower and middle income countries
In developing countries, women experience the lack of access to affordable menstrual hygiene products in addition to a lack of access to other services such as sanitation and waste disposal systems needed to manage their menstrual cycles. Lack of access to waste disposal leads women to throw used products in toilet systems, pit latrines, or discarded in to open areas such as bodies of water. These practices pose dangers to workers who handle these wastes as it increases possible exposure to bloodborne infections in soaked menstrual products and exposure to chemicals found in menstrual hygiene products. Inappropriate disposal also creates pressures on sanitation systems as menstrual hygiene products create sewage blockages.[52] The effects of these inadequate facilities has been shown to have social effects on girls in developing countries leading to school absenteeism.[60]
Pain management
The most common treatment for menstrual cramps are non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs can be used to reduce moderate to severe pain, and all appear similar.[61] About 1 in 5 women do not respond to NSAIDs and require alternative therapy, such as simple analgesics or heat pads.[62] Other medications for pain management include aspirin or paracetamol and combined oral contraceptives. Although combined oral contraceptives may be used, there is insufficient evidence for the efficacy of intrauterine progestogens.[63]
One review found tentative evidence that acupuncture may be useful, at least in the short term.[64] Another review found insufficient evidence to determine an effect.[65]
Society and culture

Traditions, taboos and education
Period poverty is a global issue affecting women and girls who do not have access to safe, hygienic sanitary products.[66]
Many religions have menstruation-related traditions, for example: Islam prohibits sexual contact with women during menstruation in the 2nd chapter of the Quran. Some scholars argue that menstruating women are in a state in which they are unable to maintain wudhu, and are therefore prohibited from touching the Arabic version of the Qur'an. Other biological and involuntary functions such as vomiting, bleeding, sexual intercourse, and going to the bathroom also invalidate one's wudhu.[67] In Judaism, a woman during menstruation is called Niddah and may be banned from certain actions. For example, the Jewish Torah prohibits sexual intercourse with a menstruating woman.[68] In Hinduism, menstruating women are traditionally considered ritually impure and given rules to follow. Western civilization, which has been predominantly Christian, has a history of menstrual taboos.
Menstruation education is frequently taught in combination with sex education at school in Western countries, although girls may prefer their mothers to be the primary source of information about menstruation and puberty.[69] Information about menstruation is often shared among friends and peers, which may promote a more positive outlook on puberty.[70] The quality of menstrual education in a society determines the accuracy of people's understanding of the process.[71] In many Western countries where menstruation is a taboo subject, girls tend to conceal the fact that they may be menstruating and struggle to ensure that they give no sign of menstruation.[71] Effective educational programs are essential to providing children and adolescents with clear and accurate information about menstruation. Schools can be an appropriate place for menstrual education to take place.[72] Programs led by peers or third-party agencies are another option.[72] Low-income girls are less likely to receive proper sex education on puberty, leading to a decreased understanding of why menstruation occurs and the associated physiological changes that take place. This has been shown to cause the development of a negative attitude towards menstruation.[73]
Evolution
Most female mammals have an estrous cycle, yet only ten primate species, four bat species, the elephant shrew and the spiny mouse have a menstrual cycle.[74][75] The lack of immediate relationship between these groups suggests that four distinct evolutionary events have caused menstruation to arise.[76]
Some anthropologists have questioned the energy cost of rebuilding the endometrium every fertility cycle. It has proposed that the energy savings of not having to continuously maintain the uterine lining more than offsets energy cost of having to rebuild the lining in the next fertility cycle, even in species such as humans where much of the lining is lost through bleeding (overt menstruation) rather than reabsorbed (covert menstruation).[77][78]
Many have questioned the evolution of overt menstruation in humans and related species, speculating on what advantage there could be to losing blood associated with dismantling the endometrium, rather than absorbing it, as most mammals do. Humans do, in fact, reabsorb about two-thirds of the endometrium each cycle. Some work asserts that overt menstruation does not occur because partial endometrial loss is beneficial in itself. Rather, the fetal development of these species requires a more developed endometrium, one which is too thick to reabsorb completely. There is a correlation between species that have overt menstruation to those that have a large uterus relative to the adult female body size.[77]
Recent reviews suggest that menstruation itself is not an evolved, adaptive trait. Rather, it is an inherent consequence of spontaneous decidualization evolving as a derived trait from non-spontaneous decidualization.[76]
The grandmother hypothesis is a hypothesis to explain the existence of menopause in human life history by identifying the adaptive value of extended kin networking.
Beginning in 1971, some research suggested that menstrual cycles of cohabiting human females became synchronized (menstrual synchrony). However, there is currently significant dispute as to whether menstrual synchrony exists.[79] A 2013 review concluded that menstrual synchrony likely does not exist.[80]
References
- 1 2 3 Women's Gynecologic Health. Jones & Bartlett Publishers. 2011. p. 94. ISBN 9780763756376. Archived from the original on 26 June 2015.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Menstruation and the menstrual cycle fact sheet". Office of Women's Health. 23 December 2014. Archived from the original on 26 June 2015. Retrieved 25 June 2015.
- 1 2 3 4 5 6 Diaz A, Laufer MR, Breech LL, American Academy of Pediatrics Committee on Adolescence, American College of Obstetricians and Gynecologists Committee on Adolescent Health (November 2006). "Menstruation in girls and adolescents: using the menstrual cycle as a vital sign". Pediatrics. 118 (5): 2245–50. doi:10.1542/peds.2006-2481. PMID 17079600.
- 1 2 "Menopause: Overview". nichd.nih.gov. 28 June 2013. Archived from the original on 2 April 2015. Retrieved 8 March 2015.
- 1 2 3 4 5 Biggs WS, Demuth RH (October 2011). "Premenstrual syndrome and premenstrual dysphoric disorder". American Family Physician. 84 (8): 918–24. PMID 22010771.
- 1 2 3 4 "Premenstrual syndrome (PMS) fact sheet". Office on Women's Health. 23 December 2014. Archived from the original on 28 June 2015. Retrieved 23 June 2015.
- ↑ Kristin H. Lopez (2013). Human Reproductive Biology. Academic Press. p. 53. ISBN 9780123821850. Archived from the original on 21 June 2015.
- ↑ Martin RD (2007). "The evolution of human reproduction: a primatological perspective". American Journal of Physical Anthropology. Suppl 45: 59–84. doi:10.1002/ajpa.20734. PMID 18046752.
- ↑ Karapanou O, Papadimitriou A (September 2010). "Determinants of menarche". Reproductive Biology and Endocrinology. 8: 115. doi:10.1186/1477-7827-8-115. PMC 2958977. PMID 20920296.
- ↑ Bull, Jonathan R.; Rowland, Simon P.; Scherwitzl, Elina Berglund; Scherwitzl, Raoul; Danielsson, Kristina Gemzell; Harper, Joyce (27 August 2019). "Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles". NPJ Digital Medicine. 2 (1): 83. doi:10.1038/s41746-019-0152-7. ISSN 2398-6352. PMC 6710244. PMID 31482137.
- 1 2 3 Carlson, Karen J; Eisenstat, Stephanie A; Ziporyn, Terra Diane (2004). The new Harvard guide to women's health. Cambridge, Massachusetts: Harvard University Press. ISBN 0-674-01343-3.
- ↑ "PMS (premenstrual syndrome)". nhs.uk. 23 April 2018. Archived from the original on 2 January 2020. Retrieved 2 January 2020.
- 1 2 3 "Premenstrual syndrome (PMS)". womenshealth.gov. 12 July 2017. Archived from the original on 8 December 2016. Retrieved 3 January 2020.
- ↑ Hofmeister, S; Bodden, S (1 August 2016). "Premenstrual Syndrome and Premenstrual Dysphoric Disorder". American Family Physician. 94 (3): 236–40. PMID 27479626.
- ↑ Shaw, Robert W.; Luesley, David; Monga, Ash K. (2010). Gynaecology E-Book: Expert Consult: Online and Print. Elsevier Health Sciences. p. 394. ISBN 978-0-7020-4838-8. Archived from the original on 8 March 2021. Retrieved 3 January 2020.
- ↑ "Water retention: Relieve this premenstrual symptom". Mayo Clinic. Archived from the original on 25 September 2011. Retrieved 20 September 2011.
- ↑ Ju H, Jones M, Mishra G (1 January 2014). "The prevalence and risk factors of dysmenorrhea". Epidemiologic Reviews. 36 (1): 104–13. doi:10.1093/epirev/mxt009. PMID 24284871.
- 1 2 3 4 5 "Dysmenorrhea - Gynecology and Obstetrics". Merck Manuals Professional Edition. Archived from the original on 10 September 2017.
- ↑ Miller L, Notter KM (November 2001). "Menstrual reduction with extended use of combination oral contraceptive pills: randomized controlled trial". Obstetrics and Gynecology. LWW Journals. 98 (5 Pt 1): 771–8. doi:10.1016/s0029-7844(01)01555-1. PMID 11704167.
- ↑ Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M (July 2015). "Nonsteroidal anti-inflammatory drugs for dysmenorrhoea". The Cochrane Database of Systematic Reviews (7): CD001751. doi:10.1002/14651858.CD001751.pub3. PMC 6953236. PMID 26224322.
- ↑ "Ectopic Pregnancy Clinical Presentation: History, Physical Examination". emedicine.medscape.com. Archived from the original on 29 March 2013.
- ↑ Sharma P, Malhotra C, Taneja DK, Saha R (February 2008). "Problems related to menstruation amongst adolescent girls". Indian Journal of Pediatrics. 75 (2): 125–9. doi:10.1007/s12098-008-0018-5. PMID 18334791.
- ↑ Ryu, Aeli; Kim, Tae-Hee (December 2015). "Premenstrual syndrome: A mini review". Maturitas. 82 (4): 436–440. doi:10.1016/j.maturitas.2015.08.010. PMID 26351143.
- 1 2 Mishra, Sanskriti; Marwaha, Raman (2019), "Premenstrual Dysphoric Disorder", StatPearls, StatPearls Publishing, PMID 30335340, archived from the original on 27 September 2020, retrieved 5 August 2019
- ↑ Meczekalski B, Katulski K, Czyzyk A, Podfigurna-Stopa A, Maciejewska-Jeske M (November 2014). "Functional hypothalamic amenorrhea and its influence on women's health". Journal of Endocrinological Investigation. 37 (11): 1049–56. doi:10.1007/s40618-014-0169-3. PMC 4207953. PMID 25201001.
- ↑ Farage, Miranda (22 March 2013). The Vulva: Anatomy, Physiology, and Pathology. CRC Press. pp. 155–158.
- ↑ "Menstrual blood problems: Clots, color and thickness". WebMD. Archived from the original on 23 September 2011. Retrieved 20 September 2011.
- ↑ Clancy, Kate (27 July 2011). "Iron-deficiency is not something you get just for being a lady". SciAm. Archived from the original on 17 March 2012.
{{cite web}}: External link in|author= - ↑ Kepczyk T, Cremins JE, Long BD, Bachinski MB, Smith LR, McNally PR (January 1999). "A prospective, multidisciplinary evaluation of premenopausal women with iron-deficiency anemia". The American Journal of Gastroenterology. 94 (1): 109–15. PMID 9934740.
- ↑ Fraser IS, Critchley HO, Munro MG, Broder M (March 2007). "Can we achieve international agreement on terminologies and definitions used to describe abnormalities of menstrual bleeding?". Human Reproduction. 22 (3): 635–43. doi:10.1093/humrep/del478. PMID 17204526.
- ↑ "Health risks of female genital mutilation (FGM)". World Health Organization. Archived from the original on 29 November 2014.
- ↑ Levay S, Baldwin J, Baldwin J (2015). "Women's Bodies". Discovering Human Sexuality. Massachusetts: Sinauer Associates, Inc. p. 44. ISBN 9781605352756.
- ↑ Thornhill R, Gangestad SW (2008). "Background and Overview of the Book". The Evolutionary Biology of Human Female Sexuality. New York: Oxford University Press. p. 12. ISBN 9780195340990.
- ↑ "Can I have sex during my period? Can I get pregnant during my period?". www.plannedparenthood.org. Retrieved 18 April 2023.
- ↑ "6 Things You Should Know About Having Sex During Your Period". Time. 7 August 2017. Archived from the original on 2 October 2022. Retrieved 18 April 2023.
- ↑ CYWH Staff (18 October 2011). "Medical Uses of the Birth Control Pill". Archived from the original on 5 February 2013. Retrieved 1 February 2013.
- ↑ Curtis, Kathryn M.; Tepper, Naomi K.; Jatlaoui, Tara C.; Berry-Bibee, Erin; Horton, Leah G.; Zapata, Lauren B.; Simmons, Katharine B.; Pagano, H. Pamela; Jamieson, Denise J. (2016). "U.S. Medical Eligibility Criteria for Contraceptive Use, 2016". MMWR. Recommendations and Reports. 65 (3): 1–103. doi:10.15585/mmwr.rr6503a1. ISSN 1057-5987. PMID 27467196.
- ↑ "Delaying your period with birth control pills". Mayo Clinic. Archived from the original on 26 September 2011. Retrieved 20 September 2011.
- ↑ "How can I delay my period while on holiday?". National Health Service, United Kingdom. Archived from the original on 5 August 2011. Retrieved 20 September 2011.
- 1 2 3 4 5 Rome, Ellen S.; Strandjord, Sarah E. (22 September 2015). "Monthly Periods—Are They Necessary?". Pediatric Annals. 44 (9): e231–e236. doi:10.3928/00904481-20150910-11. ISSN 0090-4481. PMID 26431242.
- ↑ Schmidt, Elizabeth O.; James, Aimee; Curran, K. Michele; Peipert, Jeffrey F.; Madden, Tessa (October 2015). "Adolescent Experiences With Intrauterine Devices: A Qualitative Study". The Journal of Adolescent Health. 57 (4): 381–386. doi:10.1016/j.jadohealth.2015.05.001. ISSN 1879-1972. PMC 4583802. PMID 26126950.
- ↑ Kovacs, G. (October 1996). "Progestogen-only pills and bleeding disturbances". Human Reproduction (Oxford, England). 11 Suppl 2: 20–23. doi:10.1093/humrep/11.suppl_2.20. ISSN 0268-1161. PMID 8982741.
- ↑ "Do you really need to have a period every month?". Discovery Health. 27 January 2009. Archived from the original on 8 February 2013. Retrieved 20 September 2011.
- ↑ Lind, Amy; Brzuzy, Stephanie (2007). Battleground: Women, Gender, and Sexuality: Volume 2: M–Z. Greenwood. p. 348. ISBN 978-0-313-34039-0.
- 1 2 Kantartzis, Kelly L.; Sucato, Gina S. (June 2013). "Menstrual suppression in the adolescent". Journal of Pediatric and Adolescent Gynecology. 26 (3): 132–137. doi:10.1016/j.jpag.2012.08.007. ISSN 1873-4332. PMID 23158755.
- ↑ Kam, Katherine. "Eliminate periods with birth control?". WebMD. Archived from the original on 2 September 2011. Retrieved 20 September 2011.
- ↑ McNeilly AS (2001). "Lactational control of reproduction". Reproduction, Fertility, and Development. 13 (7–8): 583–90. doi:10.1071/RD01056. PMID 11999309.
- ↑ Kippley, John; Kippley, Sheila (1996). The Art of Natural Family Planning (4th ed.). Cincinnati, OH: The Couple to Couple League. p. 347. ISBN 0-926412-13-2.
- ↑ Stallings JF, Worthman CM, Panter-Brick C, Coates RJ (February 1996). "Prolactin response to suckling and maintenance of postpartum amenorrhea among intensively breastfeeding Nepali women". Endocrine Research. 22 (1): 1–28. doi:10.3109/07435809609030495. PMID 8690004.
- ↑ "Breastfeeding: Does It Really Space Babies?". The Couple to Couple League International. Internet Archive. 17 January 2008. Archived from the original on 17 January 2008. Retrieved 21 September 2008., which cites:
- Kippley SK, Kippley JF (November–December 1972). "The relation between breastfeeding and amenorrhea: report of a survey". JOGN Nursing; Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1 (4): 15–21. doi:10.1111/j.1552-6909.1972.tb00558.x. PMID 4485271.
- Kippley SK (November–December 1986 and January–February 1987). "Breastfeeding survey results similar to 1971 study". The CCL News. 13 (3): 10.
{{cite journal}}: Check date values in:|date=(help) and 13(4): 5.
- ↑ Davis, Nicola (18 July 2019). "'We don't need to bleed': why many women are giving up on periods". The Guardian. Archived from the original on 18 July 2019. Retrieved 18 July 2019.
- 1 2 Kaur, Rajanbir; Kaur, Kanwaljit; Kaur, Rajinder (2018). "Menstrual Hygiene, Management, and Waste Disposal: Practices and Challenges Faced by Girls/Women of Developing Countries". Journal of Environmental and Public Health. 2018: 1730964. doi:10.1155/2018/1730964. ISSN 1687-9805. PMC 5838436. PMID 29675047.
- 1 2 "UK girls 'too poor to afford tampons'". 14 March 2017. Archived from the original on 27 April 2019. Retrieved 27 April 2019.
- 1 2 Tamiru, Selamawit; Mamo, Kuribachew; Acidria, Pasquina; Mushi, Rozalia; Ali, Chemisto Satya; Ndebele, Lindiwe (2015). "Towards a sustainable solution for school menstrual hygiene management: Cases of Ethiopia, Uganda, South-Sudan, Tanzania, and Zimbabwe". Waterlines. 34: 92–102. doi:10.3362/1756-3488.2015.009.
- ↑ House, S., Mahon, T., Cavill, S. (2012). Menstrual hygiene matters - A resource for improving menstrual hygiene around the world Archived 24 September 2015 at the Wayback Machine. WaterAid, UK
- ↑ Chin, L. (2014) Period of shame - The Effects of Menstrual Hygiene Management on Rural Women and Girls' Quality of Life in Savannakhet, Laos [Master's thesis] LUMID International Master programme in applied International Development and Management http://lup.lub.lu.se/student-papers/record/4442938 Archived 28 August 2021 at the Wayback Machine [accessed 10 August 2015]
- ↑ Rozema, Kyle; Cotropia, Christopher Anthony (29 March 2018). "Who Benefits from Repealing Tampon Taxes? Empirical Evidence from New Jersey". Journal of Empirical Legal Studies. Rochester, NY. 15 (3): 620–647. doi:10.1111/jels.12188. SSRN 3233238.
- ↑ Khomami, Nadia (24 August 2018). "Scotland to offer free sanitary products to all students in world first". The Guardian. ISSN 0261-3077. Archived from the original on 27 April 2019. Retrieved 27 April 2019.
- ↑ Stewart, Heather (9 March 2019). "Hammond to promise funds to end period poverty in English schools". The Guardian. ISSN 0261-3077. Archived from the original on 27 April 2019. Retrieved 27 April 2019.
- ↑ Kaur, Rajanbir; Kaur, Kanwaljit; Kaur, Rajinder (20 February 2018). "Menstrual Hygiene, Management, and Waste Disposal: Practices and Challenges Faced by Girls/Women of Developing Countries". Journal of Environmental and Public Health. 2018: 1–9. doi:10.1155/2018/1730964. ISSN 1687-9805. PMC 5838436. PMID 29675047.
- ↑ Latthe, PM; Champaneria, R; Hellman, Kevin M. (21 October 2014). "Dysmenorrhoea". BMJ Clinical Evidence. 2014: 390–400. doi:10.1016/j.ajog.2017.08.108. PMC 4205951. PMID 25338194.
- ↑ Oladosu, Folabomi A.; Tu, Frank F.; Hellman, Kevin M. (April 2018). "Nonsteroidal antiinflammatory drug resistance in dysmenorrhea: epidemiology, causes, and treatment". American Journal of Obstetrics and Gynecology. 218 (4): 390–400. doi:10.1016/j.ajog.2017.08.108. PMC 5839921. PMID 28888592.
- ↑ Latthe, PM; Champaneria, R (21 October 2014). "Dysmenorrhoea". BMJ Clinical Evidence. 2014: 390–400. doi:10.1016/j.ajog.2017.08.108. PMC 4205951. PMID 25338194.
- ↑ Woo, Hye Lin; Ji, Hae Ri; Pak, Yeon Kyoung; Lee, Hojung; Heo, Su Jeong; Lee, Jin Moo; Park, Kyoung Sun (June 2018). "The efficacy and safety of acupuncture in women with primary dysmenorrhea". Medicine. 97 (23): e11007. doi:10.1097/MD.0000000000011007. PMC 5999465. PMID 29879061.
- ↑ Smith, Caroline A; Armour, Mike; Zhu, Xiaoshu; Li, Xun; Lu, Zhi Yong; Song, Jing (18 April 2016). "Acupuncture for dysmenorrhoea". Cochrane Database of Systematic Reviews. 4: CD007854. doi:10.1002/14651858.CD007854.pub3. PMID 27087494.
- ↑ "Archive copy". Archived from the original on 30 October 2019. Retrieved 3 June 2020.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Sahih Bukhari, Chapter: 6, Menstrual Periods". Archived from the original on 30 September 2018. Retrieved 18 September 2018.
- ↑ Leviticus 15:19-30, 18:19, 20:18
- ↑ Sooki Z, Shariati M, Chaman R, Khosravi A, Effatpanah M, Keramat A (March 2016). "The Role of Mother in Informing Girls About Puberty: A Meta-Analysis Study". Nursing and Midwifery Studies. 5 (1): e30360. doi:10.17795/nmsjournal30360. PMC 4915208. PMID 27331056.
- ↑ Hatami M, Kazemi A, Mehrabi T (30 December 2015). "Effect of peer education in school on sexual health knowledge and attitude in girl adolescents". Journal of Education and Health Promotion. 4: 78. doi:10.4103/2277-9531.171791 (inactive 22 May 2020). PMC 4944604. PMID 27462620.
{{cite journal}}: CS1 maint: DOI inactive as of May 2020 (link) - 1 2 Allen KR, Kaestle CE, Goldberg AE (February 2011). "More than just a punctuation mark: How boys and young men learn about menstruation". Journal of Family Issues. 32 (2): 129–56. doi:10.1177/0192513x10371609.
- 1 2 Kirby D (February 2002). "The impact of schools and school programs upon adolescent sexual behavior". Journal of Sex Research. 39 (1): 27–33. doi:10.1080/00224490209552116. PMID 12476253.
- ↑ Herbert, Ann C.; Ramirez, Ana Maria; Lee, Grace; North, Savannah J.; Askari, Melanie S.; West, Rebecca L.; Sommer, Marni (April 2017). "Puberty Experiences of Low-Income Girls in the United States: A Systematic Review of Qualitative Literature From 2000 to 2014". The Journal of Adolescent Health. 60 (4): 363–379. doi:10.1016/j.jadohealth.2016.10.008. ISSN 1879-1972. PMID 28041680.
- ↑ "Why do women menstruate?". ScienceBlogs. 2011. Archived from the original on 27 January 2013. Retrieved 15 January 2013.
- ↑ Bellofiore N, Ellery SJ, Mamrot J, Walker DW, Temple-Smith P, Dickinson H (January 2017). "First evidence of a menstruating rodent: the spiny mouse (Acomys cahirinus)". American Journal of Obstetrics and Gynecology. 216 (1): 40.e1–40.e11. doi:10.1016/j.ajog.2016.07.041. PMID 27503621.
- 1 2 Emera D, Romero R, Wagner G (January 2012). "The evolution of menstruation: a new model for genetic assimilation: explaining molecular origins of maternal responses to fetal invasiveness". BioEssays. 34 (1): 26–35. doi:10.1002/bies.201100099. PMC 3528014. PMID 22057551.
- 1 2 Strassmann BI (June 1996). "The evolution of endometrial cycles and menstruation". The Quarterly Review of Biology. 71 (2): 181–220. doi:10.1086/419369. PMID 8693059.
- ↑ Kathleen O'Grady (2000). "Is Menstruation Obsolete?". The Canadian Women's Health Network. Archived from the original on 13 February 2007. Retrieved 21 January 2007.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Adams, Cecil (20 December 2002). "Does menstrual synchrony really exist?". The Straight Dope. The Chicago Reader. Archived from the original on 15 September 2008. Retrieved 10 January 2007.
- ↑ Harris AL, Vitzthum VJ (2013). "Darwin's legacy: an evolutionary view of women's reproductive and sexual functioning". Journal of Sex Research. 50 (3–4): 207–46. doi:10.1080/00224499.2012.763085. PMID 23480070.
Further reading
- Howie, Gillian; Shail, Andrew (2005). Menstruation: A Cultural History. Palgrave Macmillan. ISBN 1-4039-3935-7. Archived from the original on 15 January 2018. Retrieved 9 November 2013.
- Knight, Chris (1995). Blood Relations: Menstruation and the Origins of Culture. New Haven and London: Yale University. ISBN 0-300-04911-0. Archived from the original on 16 July 2012. Retrieved 9 November 2013.
External links
| Wikiquote has quotations related to: Menstruation |

