Menstrual cup

A menstrual cup is a menstrual hygiene device which is inserted into the vagina during menstruation. Its purpose is to collect menstrual fluid (blood from the uterine lining mixed with other fluids). Menstrual cups are usually made of flexible medical grade silicone, latex, or a thermoplastic isomer. They are shaped like a bell with a stem or a ring. The stem is used for insertion and removal. The bell-shaped cup seals against the vaginal wall just below the cervix. Every 4–12 hours (depending on the amount of flow), the cup is removed, emptied, rinsed, and reinserted. After each period, the cup requires cleaning.[1]
Unlike tampons and pads, cups collect menstrual fluid rather than absorbing it.[2][3] Menstrual cups typically do not leak if used properly, though incorrect placement or inadequate cup size can cause some women to experience leakage.[4] One cup may be reusable for up to 10 years.[4] This makes their long-term cost lower than that of disposable tampons or pads, though the initial cost is higher. As menstrual cups are reusable, they generate less solid waste than tampons and pads, both from the products themselves and from their packaging.[4] Most menstrual cup brands sell a smaller and a larger size. Some menstrual cups are sold colorless and translucent, but several brands also offer colored cups.[5]
Menstrual cups are a safe alternative to other menstrual products; risk of toxic shock syndrome infection is similar or less with menstrual cups compared to pads or tampons.[4]
Use
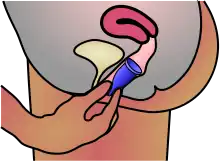
The menstrual cup is first folded or pinched and then inserted into the vagina. It will normally unfold automatically and create a light seal against the cervix. In some cases, the user may need to twist the cup or flex the vaginal muscles to ensure the cup is fully open. If correctly inserted, the cup should not leak or cause any discomfort.[6] The stem should be completely inside the vagina. If it is not, the stem can be trimmed. There are various folding techniques for insertion; common folds include the c-fold, as well as the punch-down fold.[7]
If lubrication is necessary for insertion, it should be water-based, as silicone lubricant can be damaging to the silicone.
After 4–12 hours of use (depending on the amount of flow), the cup is removed by reaching up to its stem to find the base. Simply pulling on the stem is not recommended to remove the cup, as this can create suction. The base of the cup is pinched to release the seal, and the cup is removed.[6] After emptying, a menstrual cup should be rinsed or wiped and reinserted. It can be washed with a mild soap, and sterilized in boiling water for a few minutes at the end of the cycle. Alternatively, sterilizing solutions (usually developed for baby bottles and breast pump equipment) may be used to soak the cup. Specific cleaning instructions vary by brand.
Advantages
- When using a menstrual cup, the menstrual fluid is collected after it flows from the cervix and is held in liquid form. With tampons, liquid is absorbed and held in semi-coagulated form against the cervix.[8]
- If a user needs to track the amount of menses produced (e.g., for medical reasons), a menstrual cup allows one to do so accurately.
- Users employ about 1-2 liters of water to clear menstrual cups.[9]
Acceptability studies

A 2011 randomized controlled trial in Canada investigated whether silicone menstrual cups are a viable alternative to tampons and found that approximately 91% of women in the menstrual cup group said they would continue to use the cup and recommend it to others.[10] In a 1991 clinical study involving 51 women, 23 of the participants (45%) found rubber menstrual cups to be an acceptable way of managing menstrual flow.[11]
In a pilot project among refugees in Uganda, 87% used the menstrual cup consistently over 3-months.[9]
In a randomized controlled feasibility study in rural western Kenya, adolescent primary school girls were provided with menstrual cups or sanitary pads instead of traditional menstrual care items of cloth or tissue.[12] Girls provided with menstrual cups had a lower prevalence of sexually transmitted infections than control groups. Also, the prevalence of bacterial vaginosis was lower among cup users compared with sanitary pad users or those continuing other usual practice.[12] After six months, menstrual cup users were free from embarrassing leakage or odor, and could engage in class activities and sport without humiliation or being teased.[13]
Access to water and hygiene

- Cleaning a menstrual cup in a public toilet can pose problems as the handwashing sinks are usually, though not always, in a public space rather than in the toilet cubicle. Some manufacturers suggest wiping out the cup with a clean tissue and cleaning the cup at the next private opportunity. The user could also carry a small bottle of water to rinse the cup privately over the toilet. Another option is to use wet wipes. Since menstrual cups only need to be emptied after half a day or less often (unless the flow is very heavy) many users do not have to empty them in public toilets, but rather wait until they return home.
- A lack of clean water and soap for handwashing, needed before inserting the cup, presents a problem to women in developing countries.[13] Insertion requires thorough washing of the cup and hands to avoid introducing new bacteria into the vagina, which may heighten the risk of UTIs and other infections.[14] Disposable and reusable pads do not demand the same hand hygiene, though reusable pads also require access to water for washing out pads.
- Because menstrual cups require boiling once a month, this can be a problem in developing countries if there is a lack of water, firewood, and good hygiene practices.[15] Other options currently in use, such as rags that are washed, may be less hygienic.
- Removing a menstrual cup can be messy. Sometimes menstrual blood can spill during removal, although many women remove the device while hovering over a toilet to catch such spillage.
When using a urine-diverting dry toilet, menstrual blood can be emptied into the part that receives the feces. If any menstrual blood falls into the funnel for urine, it can be rinsed away with water.[16]
Leakage
Menstrual cups collect menstrual fluid inside the vagina and generally do not leak (if emptied often enough and inserted properly). Some women have experienced leakage due to improper use or cup size. For example, a menstrual cup may leak if it is not inserted correctly and does not pop open completely and seal against the walls of the vagina. Some factors mentioned in association with leakage included menorrhagia, unusual anatomy of the uterus, need for a larger size of menstrual cup, and incorrect placement of the menstrual cup, or that it had filled to capacity.[4] However, a proper seal may continue to contain fluid in the upper vagina even if the cup is full.
The frequency of reported leakage for menstrual cups is similar or lower than for tampons and pads.[4]
Safety
Menstrual cups are safe when used as directed and no health risks related to their use have been found.[17][18]
No medical research was conducted to ensure that menstrual cups were safe prior to introduction on the market.[19] Early research in 1962 evaluated 50 women using a bell-shaped cup. The researchers obtained vaginal smears, gram stains, and basic aerobic cultures of vaginal secretions. Vaginal speculum examination was performed, and pH was measured. No significant changes were noted. This report was the first containing extensive information on the safety and acceptability of a widely used menstrual cup that included both preclinical and clinical testing and over 10 years of post-marketing surveillance.[20]
One case report noted the development of endometriosis and adenomyosis in one menstrual cup user.[21] Additionally, one survey with a small sample size indicated a possible link. Therefore, two organizations have issued a combined statement that urged further research.[19] However, the U.S. Food and Drug Administration declined to remove menstrual cups from the market, saying that there was insufficient evidence of risk.[22]
A 2011 randomized controlled trial measured urovaginal infection in a comparison of menstrual cup and tampon use, and found no difference.[10]
No differences in the growth of Staphylococcus aureus or health harms were identified among school girls provided with menstrual cups compared to those using sanitary pads, or continuing their usual practice in rural western Kenya.[12][23]
Menstrual cups can be used with an IUD; however, there is an unclear association with respect to IUD expulsion.[24][25]
Toxic shock syndrome
Toxic shock syndrome (TSS) is a potentially fatal bacterial illness. Scientists have recognized an association between TSS and tampon use, although the exact connection remains unclear.[26] TSS caused by menstrual cup use appears to be very rare.[10][27] The probable reason for this is that menstrual cups are not absorbent, do not irritate the vaginal mucosal tissue, and so do not change the vaginal flora in any measurable amount.[28] Conversely, vaginal dryness and abrasions may occur if the tampon used is more absorbent than needed for the menstrual flow, and normal liquid that should line the vaginal wall is also absorbed.[26] Research has shown that the cup has no impact on the vaginal flora, which means there is no effect on the presence of S. aureus, the bacterium that can cause TSS.[28] The risk of TSS associated with cervical caps used for contraception in the female barrier method is also very low.[29] Cervical caps and menstrual cups both use mostly medical grade silicone or latex.
A widely reported study showed that in vitro, bacteria associated with toxic shock syndrome (TSS) are capable of growing on menstrual cups.[30][31][32]
A 2019 review found the risk of toxic shock syndrome with menstrual cup use to be low, with five cases identified via their literature search.[4] Data from the United States showed rates of TSS to be lower in women using menstrual cups versus high-absorbency tampons.[4] Infection risk is similar or less with menstrual cups compared to pads or tampons.[4]
Types
Menstrual cups are generally bell-shaped, with a few exceptions. Most brands use medical grade silicone as the material for the menstrual cup, although latex and thermoplastic elastomer are also options. Menstrual cups made from silicone are generally designed to last for 1–5 years.
The majority of menstrual cups on the market are reusable, rather than disposable.[33]
Size, shape, and flexibility
Most menstrual cup brands sell a smaller and a larger size. The smaller size is typically recommended for women under 30 or women who have not given birth vaginally. The larger size is typically recommended for women over 30 or have given birth vaginally, or have a heavy flow.[34][33] However, there have been no studies that show any need for a different sized cup base on age or parity.[34] Cups with even smaller sizes are recommended for teenagers, as well as women and girls who are more physically fit, as those with stronger pelvic floor muscles may find a larger cup uncomfortable. If the cervix sits particularly low or is tilted, a shorter cup may be more suitable.[33] Capacity is important for women who have a heavier flow. The average menstrual cup holds around 20 ml. Some cups are designed to be larger and hold 37–51 ml. Most sizes have a larger capacity than a regular tampon, which is 10–12 ml.
Menstrual cups also vary by firmness or flexibility. Some companies offer a range of firmness levels in their cups. A firmer cup pops open more easily after insertion and may hold a more consistent seal against the vaginal wall (preventing leaks), but some women find softer cups more comfortable to insert.[35]
Color
The silicone of which most brands of cups are produced is naturally colorless and translucent. Several brands offer colored cups as well as, or instead of the colorless ones. Translucent cups lose their initial appearance faster than colored – they tend to get yellowish stains with use.[35] The shade of a colored cup may change over time, though stains are often not as obvious on colored cups. Stains on any color of the cup can often be removed or at least lightened by soaking the cup in diluted hydrogen peroxide and/or leaving it out in the sun for a few hours.
Most cups produced do not have any other additives to them, except for the colored cups. The coloring used is reported to be safe and approved by the FDA for medical use and food coloring.
Similar devices
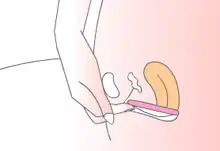
Menstrual discs (also called cervical cup)[4] are disc-shaped, like a diaphragm, with a flexible outer ring and a soft, collapsible center. They collect menstrual fluid like menstrual cups, but stay in place by hooking behind the pubic bone instead of relying on suction. Menstrual discs come in both disposable and reusable varieties.
Cost
The costs for menstrual cups vary widely, from US$0.7 to $47 per cup (based on a 2019 review of 199 brands of menstrual cups available in 99 countries).[4]
Reusable menstrual products (including menstrual cups, but not disposable menstrual cups) are more economical than disposable products. Money will be saved using a menstrual cup, compared with other options such as tampons.[10] A woman in a developed country spends an average of US$60 per year on pads and tampons.[37] If a woman menstruates for 40 years, the lifetime expense for pads and tampons is US$2,400. If the average silicone menstrual cup lasts between one and five years, then between eight and 40 would be needed in 40 years. If a menstrual cup costs US$30 (costs vary by manufacturer), the lifetime cost for a menstrual cup would be between US$240 and US$1,200.[38]
The up-front cost of a menstrual cup may be expensive for women from low-income households, especially in developing countries. Buying pads or using rags monthly may seem more affordable than purchasing a menstrual cup, though the lifetime cost is higher.[14]
Environmental impact
Since they are reusable, menstrual cups help to reduce solid waste.[39] Some disposable sanitary napkins and plastic tampon applicators can take 25 years to break down in the ocean and can cause a significant environmental impact.[40] Biodegradable sanitary options are also available,[41] and these decompose in a short period of time, but they must be composted, and not disposed of in a landfill.
When considering a 10-year time period, waste from consistent use of a menstrual cup is only a small fraction of the waste of pads or tampons.[4] For example, if compared with using 12 pads per period, use of a menstrual cup would comprise only 0.4% of the plastic waste.[4]
Each year, an estimated 20 billion pads and tampons are discarded in North America. They typically end up in landfills or are incinerated, which can have a great impact on the environment. Most of the pads and tampons are made of cotton and plastic. Plastic takes about 50 or more years and cotton starts degrading after 90 days if it is composted.[42]
Given that the menstrual cup is reusable, its use greatly decreases the amount of waste generated from menstrual cycles, as there is no daily waste and the amount of discarded packaging decreases as well. After their life span is over, the silicone cups are put in landfills or incinerated.
Menstrual cups may be emptied into a small hole in the soil or in compost piles, since menstrual fluid is a valuable fertilizer for plants and any pathogens of sexually transmitted diseases will quickly be destroyed by soil microbes.[43] The water used to rinse the cups can be disposed of in the same way. This reduces the amount of wastewater that needs to be treated.
In developing countries, solid waste management is often lacking. Here, menstrual cups have an advantage over disposable pads or tampons as they do not contribute to the solid waste issues in the communities or generate embarrassing refuse that others may see.
History
An early version of a bullet-shaped menstrual cup was patented in 1932, by the midwifery group of McGlasson and Perkins.[44] Leona Chalmers patented the first usable commercial cup in 1937.[45] Other menstrual cups were patented in 1935, 1937, and 1950.[46][47][48] The Tassaway brand of menstrual cups was introduced in the 1960s, but it was not a commercial success.[49] Early menstrual cups were made of rubber.[17]
In 1987, another latex rubber menstrual cup, The Keeper, was manufactured in the United States. This proved to be the first commercially viable menstrual cup and it is still available today. The first silicone menstrual cup was the UK-manufactured Mooncup in 2001. Most menstrual cups are now manufactured from medical grade silicone because of its durability and hypoallergenic properties, though there are also brands made of TPE (thermoplastic elastomer). Menstrual cups are becoming more popular worldwide, with many different brands, shapes, and sizes on the market.[8] Most are reusable, though there is at least one brand of disposable menstrual cups currently manufactured.[8]
Some non-governmental organizations (NGOs) and companies have begun to propose menstrual cups to females in developing countries since about 2010, for example in Kenya and South Africa.[50] Menstrual cups are regarded as a low-cost and environmentally friendly alternative to sanitary cloth, expensive disposable pads, or "nothing" – the reality for many females in developing countries.[15]
While numerous companies all over the world offer this product it was still not well known in around 2010. It may be difficult for companies to make profit from this product as one single menstrual cup can last a girl or woman five years or longer. Most women hear of menstrual cups through the internet or word of mouth, rather than through conventional advertising on TV for example.
Society and culture
Developing countries
.jpg.webp)
Menstrual cups can be useful as a means of menstrual hygiene management for women in developing countries where access to affordable sanitary products may be limited.[13][51] A lack of affordable hygiene products means inadequate, unhygienic alternatives are often used, which can present a serious health risk.[52][53] Menstrual cups offer a long-term solution compared to some other feminine hygiene products because they do not need to be replaced monthly.
The municipality of Alappuzha in Kerala, India has launched a project in 2019 and gave away 5,000 menstrual cups for free to female residents.[54] This is to encourage the use of these cups instead of non-biodegradable sanitary pads to reduce waste production.[54]
Cultural aspects
Feminine hygiene products that need to be inserted into the vagina can be unacceptable for cultural reasons. There are myths that they interfere with female reproductive organs and that they cause females to lose their virginity.[14] Use of a menstrual cup could stretch or break the hymen. Since some cultures value the preservation of the hymen as evidence of virginity (see also virginity test); this can discourage young women from using cups.
Industry Insights
According to the report published by the Facts & Factors Market Research Company, global demand for the menstrual cups market was estimated at approximately USD 720.6 Million in 2020 and is expected to generate revenue of around USD 980.4 Million by the end of 2026, growing at a CAGR of around 5.5% between 2021 and 2026. [55]
See also
- Cervical cap
- Diaphragm (contraceptive)
- Menstrual Hygiene Day
- Period panties
References
- ↑ Hillard, Paula J. Adams; Hillard, Paula Adams (2008). The 5-minute Obstetrics and Gynecology Consult. Lippincott Williams & Wilkins. p. 322. ISBN 978-0-7817-6942-6.
- ↑ Elizabeth Gunther Stewart, Paula Spencer: The V Book: A Doctor's Guide to Complete Vulvovaginal Health, Bantam Books, 2002, Seiten 96 und 97, ISBN 0-553-38114-8.
- ↑ Leslie Garrett, Peter Greenberg: The Virtuous Consumer: Your Essential Shopping Guide for a Better, Kinder and Healthier World, New World Library, 2007, Seiten 17 bis 19, ISBN 1-930722-74-5.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 van Eijk AM, Zulaika G, Lenchner M, Mason L, Sivakami M, Nyothach E, et al. (August 2019). "Menstrual cup use, leakage, acceptability, safety, and availability: a systematic review and meta-analysis". The Lancet. Public Health. 4 (8): e376–e393. doi:10.1016/S2468-2667(19)30111-2. PMC 6669309. PMID 31324419.
- ↑ Parker, Erin (28 July 2020). "These Period Cup Reviews Might Convince You to Ditch Pads and Tampons for Good". Glamour. Retrieved 2021-04-10.
- 1 2 "Vagina Anatomy - Learn Your Parts". Lunette UK. Retrieved 2018-08-31.
- ↑ "How to Use a Menstrual Cup". wikiHow. March 2, 2015. Archived from the original on July 19, 2020. Retrieved 2018-08-31.
- 1 2 3 "Alternative Menstrual Products". Center for Young Women's Health. Boston Children's Hospital. 28 March 2013. Retrieved 30 March 2013.
- 1 2 CARE International and WoMena Uganda., 2018. Ruby Cups: Girls in Imvepi Refugee Settlement Taking Control. Available from: http://womena.dk/wp-content/uploads/2018/12/Ruby-Cups-Girls-in-Imvepi-Refugee-Settlement-Taking-Control-03.12.18-Final-report.pdf
- 1 2 3 4 Howard C, Rose CL, Trouton K, Stamm H, Marentette D, Kirkpatrick N, et al. (June 2011). "FLOW (finding lasting options for women): multicentre randomized controlled trial comparing tampons with menstrual cups". Canadian Family Physician. 57 (6): e208-15. PMC 3114692. PMID 21673197.
- ↑ Cheng M, Kung R, Hannah M, Wilansky D, Shime J (September 1995). "Menses cup evaluation study". Fertility and Sterility. 64 (3): 661–3. doi:10.1016/S0015-0282(16)57812-1. PMID 7641929.
- 1 2 3 Phillips-Howard PA, Nyothach E, Ter Kuile FO, Omoto J, Wang D, Zeh C, et al. (November 2016). "Menstrual cups and sanitary pads to reduce school attrition, and sexually transmitted and reproductive tract infections: a cluster randomised controlled feasibility study in rural Western Kenya". BMJ Open. 6 (11): e013229. doi:10.1136/bmjopen-2016-013229. PMC 5168542. PMID 27881530.
- 1 2 3 Mason L, Laserson K, Oruko K, Nyothach E, Alexander K, Odhiambo F, Eleveld A, Isiye E, Ngere I, Omoto J, Mohammed A (2015). "Adolescent schoolgirls' experiences of menstrual cups and pads in rural western Kenya: a qualitative study". Waterlines. 34 (1): 15–30. doi:10.3362/1756-3488.2015.003.
- 1 2 3 Crofts, T. (2012). Menstruation hygiene management for schoolgirls in low-income countries. Loughborough: Water, Engineering and Development Center (WEDC), Loughborough University.
- 1 2 APHRC (2010). Attitudes towards, and acceptability of, menstrual cups as a method for managing menstruation: Experiences of women and schoolgirls in Nairobi, Kenya - Policy Brief No. 21. The African Population and Health Research Center (APHRC), Nairobi, Kenya
- ↑ WECF (2006). Ecological sanitation and hygienic considerations for women - Fact Sheet. Women in Europe for a Common Future, Netherlands and Germany
- 1 2 Pruthi, Sandhya (January 30, 2008). "Menstrual cup: What is it?". Mayoclinic.com.
- ↑ Stewart, Elizabeth B. (2002). The V Book: A Doctor's Guide to Complete Vulvovaginal Health. Bantam. p. 96. ISBN 978-0-553-38114-6.
- 1 2 Lione A, Guidone HC. "The ERC online questionnaire of women who used menstrual cups: summary statement of results and a call for additional research". assocpharmtox.org. Endometriosis Research Centre, Associated Pharmacologists & Toxicologists (APT).
- ↑ North BB, Oldham MJ (February 2011). "Preclinical, clinical, and over-the-counter postmarketing experience with a new vaginal cup: menstrual collection". Journal of Women's Health. 20 (2): 303–11. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Spechler S, Nieman LK, Premkumar A, Stratton P (2003). "The Keeper, a menstrual collection device, as a potential cause of endometriosis and adenomyosis". Gynecologic and Obstetric Investigation. 56 (1): 35–7. doi:10.1159/000072329. PMID 12867766. S2CID 2419337.
- ↑ Lione, Armand. "Citizen Petition on Menstrual Cups & Endometriosis" (PDF). Food and Drug Administration. Retrieved 19 December 2010.
- ↑ Juma J, Nyothach E, Laserson KF, Oduor C, Arita L, Ouma C, et al. (May 2017). "Examining the safety of menstrual cups among rural primary school girls in western Kenya: observational studies nested in a randomised controlled feasibility study". BMJ Open. 7 (4): e015429. doi:10.1136/bmjopen-2016-015429. PMC 5566618. PMID 28473520.
- ↑ Schnyer, Ariela N.; Jensen, Jeffrey T.; Edelman, Alison; Han, Leo (October 2019). "Do menstrual cups increase risk of IUD expulsion? A survey of self-reported IUD and menstrual hygiene product use in the United States". The European Journal of Contraception & Reproductive Health Care. 24 (5): 368–372. doi:10.1080/13625187.2019.1643836. ISSN 1473-0782. PMID 31335218. S2CID 198191442.
- ↑ Wiebe ER, Trouton KJ (August 2012). "Does using tampons or menstrual cups increase early IUD expulsion rates?". Contraception. 86 (2): 119–21. doi:10.1016/j.contraception.2011.12.002. PMID 22464406.
- 1 2 "Tampons and Asbestos, Dioxin, & Toxic Shock Syndrome". FDA U.S. Food and Drug Administration, U.S. Department of Health and Human Services. 13 May 2015. Retrieved 8 September 2015.
- ↑ Mitchell MA, Bisch S, Arntfield S, Hosseini-Moghaddam SM (August 2015). "A confirmed case of toxic shock syndrome associated with the use of a menstrual cup". The Canadian Journal of Infectious Diseases & Medical Microbiology. 26 (4): 218–20. doi:10.1155/2015/560959. PMC 4556184. PMID 26361491.
- 1 2 North BB, Oldham MJ (February 2011). "Preclinical, clinical, and over-the-counter postmarketing experience with a new vaginal cup: menstrual collection". Journal of Women's Health. 20 (2): 303–11. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Faculty of Family Planning & Reproductive Health Care (2007). Female Barrier Methods. Archived 2015-11-26 at the Wayback Machine London: p.3
- ↑ "Menstrual Cup Linked to Toxic Shock Syndrome, New Study Finds". Consumer Reports. Retrieved 2018-12-03.
- ↑ "Toxic shock syndrome risks: Are tampons or menstrual cups safer?". TODAY.com. Retrieved 2018-12-03.
- ↑ Nonfoux L, Chiaruzzi M, Badiou C, Baude J, Tristan A, Thioulouse J, et al. (June 2018). "In Vitro". Applied and Environmental Microbiology. 84 (12): e00351–18. doi:10.1128/aem.00351-18. PMC 5981080. PMID 29678918.
- 1 2 3 "What's a Menstrual Cup?". WebMD. Retrieved 2020-05-22.
- 1 2 Gunter, Jen (20 August 2019). The vagina bible : the vulva and the vagina--separating the myth from the medicine. p. 304. ISBN 978-0-7352-7738-0. OCLC 1099676519.
- 1 2 Eijk, Anna Maria van; Zulaika, Garazi; Lenchner, Madeline; Mason, Linda; Sivakami, Muthusamy; Nyothach, Elizabeth; Unger, Holger; Laserson, Kayla; Phillips-Howard, Penelope A. (2019-08-01). "Menstrual cup use, leakage, acceptability, safety, and availability: a systematic review and meta-analysis". The Lancet Public Health. 4 (8): e376–e393. doi:10.1016/S2468-2667(19)30111-2. ISSN 2468-2667. PMC 6669309. PMID 31324419.
- ↑ How to use an Instead Softcup, Wikihow
- ↑ "Why Choose Reusables?". GladRags. Retrieved 2019-02-22.
- ↑ Caitlyn Shaye Weir, BSc Combined Honours, Environmental Science and Gender and Women Studies, Dalhousie University (2015) April 3rd, 2015
- ↑ Bharadwaj S, Patkar A. Menstrual hygiene and management in developing countries: Taking stock Archived 2015-12-26 at the Wayback Machine; Junction Social 2004.
- ↑ "The Environmental Impact of Everyday Things". The Chic Ecologist. 2010-04-05. Retrieved 22 August 2014.
- ↑ van Schagen, Sarah (8 November 2008). "A review of eco-minded feminine products". Grist. Retrieved 22 August 2014.
- ↑ Li L, Frey M, Browning KJ (2010). "Biodegradability Study on Cotton and Polyester Fabrics" (PDF). Journal of Engineered Fibers and Fabrics. 5 (4): 155892501000500. doi:10.1177/155892501000500406. S2CID 38815400.
- ↑ CalRecycle. "Composting Reduces Growers' Concerns About Pathogens". Retrieved May 15, 2017.
- ↑ Goddard, L.J. US Patent #1,891,761 (issued December 1932).
- ↑ North BB, Oldham MJ (February 2011). "Preclinical, clinical, and over-the-counter postmarketing experience with a new vaginal cup: menstrual collection". Journal of Women's Health. 20 (2): 303–11. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Hagedora, Arthur F. US Patent #1,996,242 (issued April 1935).
- ↑ Chalmers, Leona. US Patent #2,089,113 (issued August 1937).
- ↑ Chalmers, Ileona W. US Patent #2,534,900 (issued December 1950).
- ↑ Wysocki, Susan. "New Options in Menstrual Protection" Archived 2009-05-24 at the Wayback Machine. Advance for Nurse Practitioners (November 1997).
- ↑ African Population and Health Research Center (APHRC). Use of Menstrual Cup by Adolescent Girls and Women: Potential Benefits and Key Challenges. In: Policy Brief No. 22. Nairobi: APHRC, 2010.
- ↑ Tellier M, Hyttel M, Gad M. Assessing acceptability and hygienic safety of menstrual cups as a menstrual management method for vulnerable young women in Uganda Red Cross Society’s Life Planning Skills Project, Kampala: WoMena, 2012.
- ↑ African Population and Health Research Center (APHRC). Experiences and Problems with Menstruation Among Poor Women and Schoolgirls in Nairobi. In: Policy Brief No. 20. Nairobi, Kenya: APHRC, 2010.
- ↑ Obiria M. Kenyan students could solve sanitary problem with banana-fibre pad. The Guardian. https://www.theguardian.com/global-development/2014/sep/26/kenyan-girls-sanitary-problem-banana-fibre-pad. 26 Sep 2014.
- 1 2 Bechu, S (18 June 2019). "A Kerala civic body is distributing 5,000 menstrual cups for free; here's why!". The New India. Retrieved 8 July 2019.
- ↑ (56) menstrual cups market
| Wikimedia Commons has media related to Menstrual cup. |