Allopregnanolone
 | |
 | |
| Names | |
|---|---|
| Trade names | Zulresso |
| Other names | Brexanolone; Allo; AlloP; SAGE-547; SGE-102; 5α-Pregnan-3α-ol-20-one; 5α-Pregnane-3α-ol-20-one;[1][2][3][4][5] 3α-Hydroxy-5α-pregnan-20-one; 3α,5α-Tetrahydroprogesterone; 3α,5α-THP |
IUPAC name
| |
| Clinical data | |
| Drug class | Neurosteroid |
| Main uses | Postpartum depression[6] |
| Side effects | Sleepiness, dry mouth, hot flashes, loss of consciousness[6] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Intravenous infusion[6] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a619037 |
| Legal | |
| License data |
|
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | Oral: <5%[8] |
| Protein binding | >99%[6][8] |
| Metabolism | Non-CYP450 (keto-reduction via aldo-keto reductases (AKR), glucuronidation via glucuronosyltransferases (UGT), sulfation via sulfotransferases (SULT))[6][8] |
| Elimination half-life | 9 hours[6][8] |
| Excretion | Feces: 47%[6][8] Urine: 42%[6][8] |
| Chemical and physical data | |
| Formula | C21H34O2 |
| Molar mass | 318.501 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Allopregnanolone is a naturally occurring hormone which is also used as a medication.[9][6] As a medication, it is known as brexanolone, sold under the brand name Zulresso, and used to treat postpartum depression.[6] It is given by injection into a vein over a 60-hour period under medical supervision.[6]
Common side effects include sleepiness, dry mouth, hot flashes, and loss of consciousness.[6] Other side effects may include suicidal thoughts.[6] Use in pregnancy may harm the baby.[6] It is a neurosteroid and acts as a positive allosteric modulator of the GABAA receptor.[6]
Brexanolone was approved for medical use in the United States in 2019.[6] It is not approved in either Europe or the United Kingdom as of 2022.[10] In the United States a course of medication costs 34,000 USD as of 2019.[11] The long administration time, price, and need for hospitalization, have raised concerns about accessibility.[11]
Medical uses
Brexanolone is used to treat postpartum depression in adult women.[12]
Side effects
Side effects of brexanolone include sedation (13–21%), dry mouth (3–11%), loss of consciousness (3–5%), and flushing (2–5%).[6][12][8] It can also produce euphoria to a degree similar to that of alprazolam (3–13% at infusion doses of 90–270 μg over a one-hour period).[6]
Mechanism of action
Biological function
Allopregnanolone possesses a wide variety of effects, including, in no particular order, antidepressant, anxiolytic, stress-reducing, rewarding,[13] prosocial,[14] antiaggressive,[15] prosexual,[14] sedative, pro-sleep,[16] cognitive, memory-impairment, analgesic,[17] anesthetic, anticonvulsant, neuroprotective, and neurogenic effects.[9] Fluctuations in the levels of allopregnanolone and the other neurosteroids seem to play an important role in the pathophysiology of mood, anxiety, premenstrual syndrome, catamenial epilepsy, and various other neuropsychiatric conditions.[18][19][20]
During pregnancy, allopregnanolone and pregnanolone are involved in sedation and anesthesia of the fetus.[21][22]
Molecular interactions
Allopregnanolone is an endogenous inhibitory pregnane neurosteroid.[9] It is made from progesterone, and is a positive allosteric modulator of the action of γ-aminobutyric acid (GABA) at GABAA receptor.[9] Allopregnanolone has effects similar to those of other positive allosteric modulators of the GABA action at GABAA receptor such as the benzodiazepines, including anxiolytic, sedative, and anticonvulsant activity.[9][23][24] Endogenously produced allopregnanolone exerts a neurophysiological role by fine-tuning of GABAA receptor and modulating the action of several positive allosteric modulators and agonists at GABAA receptor.[25]
Allopregnanolone acts as a highly potent positive allosteric modulator of the GABAA receptor.[9] While allopregnanolone, like other inhibitory neurosteroids such as THDOC, positively modulates all GABAA receptor isoforms, those isoforms containing δ subunits exhibit the greatest potentiation.[26] Allopregnanolone has also been found to act as a positive allosteric modulator of the GABAA-ρ receptor, though the implications of this action are unclear.[27][28] In addition to its actions on GABA receptors, allopregnanolone, like progesterone, is known to be a negative allosteric modulator of nACh receptors,[29] and also appears to act as a negative allosteric modulator of the 5-HT3 receptor.[30] Along with the other inhibitory neurosteroids, allopregnanolone appears to have little or no action at other ligand-gated ion channels, including the NMDA, AMPA, kainate, and glycine receptors.[31]
Unlike progesterone, allopregnanolone is inactive at the classical nuclear progesterone receptor (PR).[31] However, allopregnanolone can be intracellularly oxidized into 5α-dihydroprogesterone, which does act as an agonist of the PR, and for this reason, allopregnanolone can produce PR-mediated progestogenic effects.[32][33] In addition, allopregnanolone was reported in 2012 to be an agonist of the membrane progesterone receptors (mPRs) discovered shortly before, including mPRδ, mPRα, and mPRβ, with its activity at these receptors about a magnitude more potent than at the GABAA receptor.[34][35] The action of allopregnanolone at these receptors may be related, in part, to its neuroprotective and antigonadotropic properties.[34][36] Also like progesterone, recent evidence has shown that allopregnanolone is an activator of the pregnane X receptor.[31][37]
Similarly to many other GABAA receptor positive allosteric modulators, allopregnanolone has been found to act as an inhibitor of L-type voltage-gated calcium channels (L-VGCCs),[38] including α1 subtypes Cav1.2 and Cav1.3.[39] However, the threshold concentration of allopregnanolone to inhibit L-VGCCs was determined to be 3 μM (3,000 nM), which is far greater than the concentration of 5 nM that has been estimated to be naturally produced in the human brain.[39] Thus, inhibition of L-VGCCs is unlikely of any actual significance in the effects of endogenous allopregnanolone.[39] Also, allopregnanolone, along with several other neurosteroids, has been found to activate the G protein-coupled bile acid receptor (GPBAR1, or TGR5).[40] However, it is only able to do so at micromolar concentrations, which, similarly to the case of the L-VGCCs, are far greater than the low nanomolar concentrations of allopregnanolone estimated to be present in the brain.[40]
Biphasic actions at the GABAA receptor
Increased levels of allopregnanolone can produce paradoxical effects, including negative mood, anxiety, irritability, and aggression.[41][42][43] This appears to be because allopregnanolone possesses biphasic, U-shaped actions at the GABAA receptor – moderate level increases (in the range of 1.5–2 nmol/L total allopregnanolone, which are approximately equivalent to luteal phase levels) inhibit the activity of the receptor, while lower and higher concentration increases stimulate it.[41][42] This seems to be a common effect of many GABAA receptor positive allosteric modulators.[18][43] In accordance, acute administration of low doses of micronized progesterone (which reliably elevates allopregnanolone levels) has been found to have negative effects on mood, while higher doses have a neutral effect.[44]
Antidepressant effects
The mechanism by which neurosteroid GABAA receptor PAMs like brexanolone have antidepressant effects is unknown.[45] Other GABAA receptor PAMs, such as benzodiazepines, are not thought of as antidepressants and have no proven efficacy,[45] despite clinicians prescribing Alprazolam for depression in the past.[46][47] Neurosteroid GABAA receptor PAMs are known to interact with GABAA receptors and sub-populations differently than benzodiazepines.[45] As examples, GABAA receptor-potentiating neurosteroids may preferentially target δ subunit-containing GABAA receptors, and enhance both tonic and phasic inhibition mediated by GABAA receptors.[45] It is also possible that neurosteroids like allopregnanolone may act on other targets, including membrane progesterone receptors, T-type voltage-gated calcium channels, and others, to mediate antidepressant effects.[45]
Pharmacology
Pharmacokinetics
Brexanolone has low oral bioavailability of less than 5%, necessitating non-oral administration.[8] The volume of distribution of brexanolone is approximately 3 L/kg.[8] Its plasma protein binding is more than 99%.[6][8] Brexanolone is metabolized by keto-reduction mediated via aldo-keto reductases.[6][8] The compound is also conjugated by glucuronidation via glucuronosyltransferases and sulfation via sulfotransferases.[6] It is not metabolized importantly by the cytochrome P450 system.[6][8] The three main metabolites of brexanolone are inactive.[8] The elimination half-life of brexanolone is 9 hours.[6][8] Its total plasma clearance is 1 L/h/kg.[8] It is excreted 47% in feces and 42% in urine.[6][8] Less than 1% is excreted as unchanged brexanolone.[8]
Chemistry
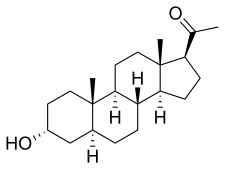
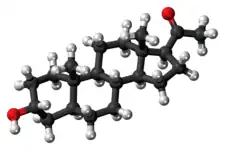
Allopregnanolone is a pregnane (C21) steroid and is also known as 5α-pregnan-3α-ol-20-one, 5α-Pregnane-3α-ol-20-one,[1][2][3][4][5] 3α-hydroxy-5α-pregnan-20-one, or 3α,5α-tetrahydroprogesterone (3α,5α-THP). It is closely related structurally to 5-pregnenolone (pregn-5-en-3β-ol-20-dione), progesterone (pregn-4-ene-3,20-dione), the isomers of pregnanedione (5-dihydroprogesterone; 5-pregnane-3,20-dione), the isomers of 4-pregnenolone (3-dihydroprogesterone; pregn-4-en-3-ol-20-one), and the isomers of pregnanediol (5-pregnane-3,20-diol). In addition, allopregnanolone is one of four isomers of pregnanolone (3,5-tetrahydroprogesterone), with the other three isomers being pregnanolone (5β-pregnan-3α-ol-20-one), isopregnanolone (5α-pregnan-3β-ol-20-one), and epipregnanolone (5β-pregnan-3β-ol-20-one).
Biosynthesis
The biosynthesis of allopregnanolone in the brain starts with the conversion of progesterone into 5α-dihydroprogesterone by 5α-reductase. After that, 3α-hydroxysteroid dehydrogenase converts this intermediate into allopregnanolone.[9] Allopregnanolone in the brain is produced by cortical and hippocampus pyramidal neurons and pyramidal-like neurons of the basolateral amygdala.[48]
Derivatives
A variety of synthetic derivatives and analogues of allopregnanolone with similar activity and effects exist, including alfadolone (3α,21-dihydroxy-5α-pregnane-11,20-dione), alfaxolone (3α-hydroxy-5α-pregnane-11,20-dione), ganaxolone (3α-hydroxy-3β-methyl-5α-pregnan-20-one), hydroxydione (21-hydroxy-5β-pregnane-3,20-dione), minaxolone (11α-(dimethylamino)-2β-ethoxy-3α-hydroxy-5α-pregnan-20-one), Org 20599 (21-chloro-3α-hydroxy-2β-morpholin-4-yl-5β-pregnan-20-one), Org 21465 (2β-(2,2-dimethyl-4-morpholinyl)-3α-hydroxy-11,20-dioxo-5α-pregnan-21-yl methanesulfonate), and renanolone (3α-hydroxy-5β-pregnan-11,20-dione).
The 21-hydroxylated derivative of this compound, tetrahydrodeoxycorticosterone (THDOC), is an endogenous inhibitory neurosteroid with similar properties to those of allopregnanolone, and the 3β-methyl analogue of allopregnanolone, ganaxolone, is under development to treat epilepsy and other conditions, including post-traumatic stress disorder (PTSD).[9]
History
In March 2019, brexanolone was approved in the United States for the treatment of postpartum depression (PPD) in adult women,[12][49] the first drug approved by the U.S. Food and Drug Administration (FDA) specifically for PPD.[12]
The efficacy of brexanolone was shown in two clinical studies in participants who received a 60-hour continuous intravenous infusion of brexanolone or placebo and were then followed for four weeks.[12] The FDA approved allopregnanolone based on evidence from three clinical trials, conducted in the United States, (Trial 1/NCT02942004, Trial 3/NCT02614541, Trial 2/ NCT02942017) of 247 women with moderate or severe postpartum depression.[50]
The FDA granted the application for brexanolone priority review designation, breakthrough therapy designation, and granted approval of allopregnanolone to Sage Therapeutics, Inc.[12] The U.S. Food and Drug Administration (FDA) considers it to be a first-in-class medication.[51]
Society and culture
Names
Allopregnanolone is the name of the molecule commonly used in the literature when it is discussed as an endogenous neurosteroid. Brexanolone is both the INN and the USAN in the context of its use as a medication.[52][53]
Zulresso is a brand name of the medication.[6]
Legal status
In the United States, brexanolone is a Schedule IV controlled substance.[7][6] Allopregnanolone is available only through a restricted program called the Zulresso REMS Program that requires the drug to be administered by a healthcare provider in a certified healthcare facility. The REMS requires that patients be enrolled in the program prior to administration of the drug.[12]
Dose
It is given continuously by intravenous infusion over a period of 60 hours (2.5 days).[6] The dosage of brexanolone is progressively adjusted over a range of 30 to 90 μg/kg/hour during this period.[6]
Several warnings and precautions are addressed in a Boxed Warning in the drug's prescribing information.[12] Because of the risk of serious harm due to the sudden loss of consciousness, patients must be monitored for excessive sedation and sudden loss of consciousness and have continuous pulse oximetry monitoring (monitors oxygen levels in the blood).[12] While receiving the infusion, women must be accompanied during interactions with children.[12] Women should be counseled on the risks of allopregnanolone treatment and instructed that they must be monitored for these effects at a healthcare facility for the entire 60 hours of infusion.[12] Women who have received the treatment should not drive, operate machinery, or do other dangerous activities until feelings of sleepiness from the treatment have completely gone away.[12]
Available forms
Brexanolone is an aqueous mixture of synthetic allopregnanolone and sulfobutyl ether β-cyclodextrin (betadex sulfobutyl ether sodium), a solubilizing agent.[6][8] It is provided at an allopregnanolone concentration of 100 mg/20 mL (5 mg/mL) in single-dose vials for use by intravenous infusion.[6] Each mL of brexanolone solution contains 5 mg allopregnanolone, 250 mg sulfobutyl ether β-cyclodextrin, 0.265 mg citric acid monohydrate, 2.57 mg sodium citrate dihydrate, and water for injection.[6] The solution is hypertonic and must be diluted to a target concentration of 1 mg/mL with sterile water and sodium chloride prior to administration.[6] Five infusion bags are generally required for the full infusion.[6] More than five infusion bags are necessary for patients weighing more than 90 kg (200 lbs).[6]
Research
Brexanolone was under development as an intravenously administered medication for the treatment of major depressive disorder, super-refractory status epilepticus, and essential tremor, but development for these indications was discontinued.[54]
Exogenous progesterone, such as oral progesterone, elevates allopregnanolone levels in the body with good dose-to-serum level correlations.[55] Due to this, it has been suggested that oral progesterone could be described as a prodrug of sorts for allopregnanolone.[55] As a result, there has been some interest in using oral progesterone to treat catamenial epilepsy,[56] as well as other menstrual cycle-related and neurosteroid-associated conditions. In addition to oral progesterone, oral pregnenolone has also been found to act as a prodrug of allopregnanolone,[57][58][59] though also of pregnenolone sulfate.[60]
References
- 1 2 Krieger NR, Mok WM, Herschkowitz S (September 1990). "5α-Pregnane-3α-ol-20-one Identified as an Active Molecular Species of Steroid Anesthetic in Brain". Anesthesiology. 73. doi:10.1097/00000542-199009001-00702.
- 1 2 Yagen B, Gallili GE, Mateles RI (August 1978). "Progesterone biotransformation by plant cell suspension cultures". Applied and Environmental Microbiology. 36 (2): 213–6. Bibcode:1978ApEnM..36..213Y. doi:10.1128/AEM.36.2.213-216.1978. PMC 291203. PMID 697360.
- 1 2 Meyer HH, Jewgenow K, Hodges JK (February 1997). "Binding activity of 5alpha-reduced gestagens to the progestin receptor from African elephant (Loxodonta africana)". General and Comparative Endocrinology. 105 (2): 164–7. doi:10.1006/gcen.1996.6813. PMID 9038248.
- 1 2 Frye C, Seliga A (May 2002). "Olanzapine and progesterone have dose-dependent and additive effects to enhance lordosis and progestin concentrations of rats". Physiology & Behavior. 76 (1): 151–8. doi:10.1016/s0031-9384(02)00689-3. PMID 12175598. S2CID 38249308.
- 1 2 Mahendroo M, Wilson JD, Richardson JA, Auchus RJ (July 2004). "Steroid 5alpha-reductase 1 promotes 5alpha-androstane-3alpha,17beta-diol synthesis in immature mouse testes by two pathways". Molecular and Cellular Endocrinology. 222 (1–2): 113–20. doi:10.1016/j.mce.2004.04.009. PMID 15249131. S2CID 54297812.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 "Zulresso- brexanolone injection, solution". DailyMed. 18 November 2019. Archived from the original on 2 July 2019. Retrieved 23 November 2019.
- 1 2 "DEA Schedules Postpartum Depression Treatment Zulresso". Monthly Prescribing Reference. 17 June 2019. Archived from the original on 3 September 2019. Retrieved 24 November 2019.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Scott LJ (May 2019). "Brexanolone: First Global Approval". Drugs. 79 (7): 779–783. doi:10.1007/s40265-019-01121-0. PMID 31006078. S2CID 123095177.
- 1 2 3 4 5 6 7 8 Reddy DS (2010). Neurosteroids: endogenous role in the human brain and therapeutic potentials. Prog. Brain Res. Progress in Brain Research. Vol. 186. pp. 113–37. doi:10.1016/B978-0-444-53630-3.00008-7. ISBN 9780444536303. PMC 3139029. PMID 21094889.
- ↑ "Brexanolone". SPS - Specialist Pharmacy Service. 21 January 2016. Archived from the original on 1 November 2019. Retrieved 11 January 2022.
- 1 2 Chatterjee R (21 March 2019). "New Postpartum Depression Drug Could Be Hard To Access For Moms Most In Need". NPR. Archived from the original on 21 March 2019. Retrieved 22 March 2019.
- 1 2 3 4 5 6 7 8 9 10 11 12 "FDA approves first treatment for post-partum depression". U.S. Food and Drug Administration (FDA) (Press release). 19 March 2019. Archived from the original on 11 October 2019. Retrieved 21 March 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Rougé-Pont F, Mayo W, Marinelli M, Gingras M, Le Moal M, Piazza PV (July 2002). "The neurosteroid allopregnanolone increases dopamine release and dopaminergic response to morphine in the rat nucleus accumbens". The European Journal of Neuroscience. 16 (1): 169–73. doi:10.1046/j.1460-9568.2002.02084.x. PMID 12153544. S2CID 9953445.
- 1 2 Frye CA (December 2009). "Neurosteroids' effects and mechanisms for social, cognitive, emotional, and physical functions". Psychoneuroendocrinology. 34 Suppl 1: S143-61. doi:10.1016/j.psyneuen.2009.07.005. PMC 2898141. PMID 19656632.
- ↑ Pinna G, Costa E, Guidotti A (February 2005). "Changes in brain testosterone and allopregnanolone biosynthesis elicit aggressive behavior". Proceedings of the National Academy of Sciences of the United States of America. 102 (6): 2135–40. Bibcode:2005PNAS..102.2135P. doi:10.1073/pnas.0409643102. PMC 548579. PMID 15677716.
- ↑ Terán-Pérez G, Arana-Lechuga Y, Esqueda-León E, Santana-Miranda R, Rojas-Zamorano JÁ, Velázquez Moctezuma J (October 2012). "Steroid hormones and sleep regulation". Mini Reviews in Medicinal Chemistry. 12 (11): 1040–8. doi:10.2174/138955712802762167. PMID 23092405.
- ↑ Patte-Mensah C, Meyer L, Taleb O, Mensah-Nyagan AG (February 2014). "Potential role of allopregnanolone for a safe and effective therapy of neuropathic pain". Progress in Neurobiology. 113: 70–8. doi:10.1016/j.pneurobio.2013.07.004. PMID 23948490. S2CID 207407077.
- 1 2 Bäckström T, Andersson A, Andreé L, Birzniece V, Bixo M, Björn I, et al. (December 2003). "Pathogenesis in menstrual cycle-linked CNS disorders". Annals of the New York Academy of Sciences. 1007 (1): 42–53. Bibcode:2003NYASA1007...42B. doi:10.1196/annals.1286.005. PMID 14993039. S2CID 20995334.
- ↑ Guille C, Spencer S, Cavus I, Epperson CN (July 2008). "The role of sex steroids in catamenial epilepsy and premenstrual dysphoric disorder: implications for diagnosis and treatment". Epilepsy & Behavior. 13 (1): 12–24. doi:10.1016/j.yebeh.2008.02.004. PMC 4112568. PMID 18346939.
- ↑ Finocchi C, Ferrari M (May 2011). "Female reproductive steroids and neuronal excitability". Neurological Sciences. 32 Suppl 1: S31-5. doi:10.1007/s10072-011-0532-5. PMID 21533709. S2CID 8885335.
- ↑ Mellor DJ, Diesch TJ, Gunn AJ, Bennet L (November 2005). "The importance of 'awareness' for understanding fetal pain". Brain Research. Brain Research Reviews. 49 (3): 455–71. doi:10.1016/j.brainresrev.2005.01.006. PMID 16269314. S2CID 9833426.
- ↑ Lagercrantz H, Changeux JP (March 2009). "The emergence of human consciousness: from fetal to neonatal life". Pediatric Research. 65 (3): 255–60. doi:10.1203/PDR.0b013e3181973b0d. PMID 19092726. S2CID 39391626. Archived from the original on 15 October 2021. Retrieved 16 September 2021.
[...] the fetus is sedated by the low oxygen tension of the fetal blood and the neurosteroid anesthetics pregnanolone and the sleep-inducing prostaglandin D2 provided by the placenta (36).
- ↑ Reddy DS, Rogawski MA (2012). "Neurosteroids — Endogenous Regulators of Seizure Susceptibility and Role in the Treatment of Epilepsy". Jasper's Basic Mechanisms of the Epilepsies, 4th Edition: 984–1002. doi:10.1093/med/9780199746545.003.0077. ISBN 9780199746545. PMID 22787590. Archived from the original on 25 September 2019. Retrieved 16 September 2021.
- ↑ Kokate TG, Svensson BE, Rogawski MA (September 1994). "Anticonvulsant activity of neurosteroids: correlation with gamma-aminobutyric acid-evoked chloride current potentiation". The Journal of Pharmacology and Experimental Therapeutics. 270 (3): 1223–9. PMID 7932175.
- ↑ Pinna G, Uzunova V, Matsumoto K, Puia G, Mienville JM, Costa E, et al. (January 2000). "Brain allopregnanolone regulates the potency of the GABA(A) receptor agonist muscimol". Neuropharmacology. 39 (3): 440–8. doi:10.1016/S0028-3908(99)00149-5. PMID 10698010. S2CID 42753647.
- ↑ Nik AM, Pressly B, Singh V, Antrobus S, Hulsizer S, Rogawski MA, et al. (July 2017). "Rapid Throughput Analysis of GABAA Receptor Subtype Modulators and Blockers Using DiSBAC1(3) Membrane Potential Red Dye". Molecular Pharmacology. 92 (1): 88–99. doi:10.1124/mol.117.108563. PMC 5452057. PMID 28428226.
- ↑ Morris KD, Moorefield CN, Amin J (October 1999). "Differential modulation of the gamma-aminobutyric acid type C receptor by neuroactive steroids". Molecular Pharmacology. 56 (4): 752–9. PMID 10496958.
- ↑ Li W, Jin X, Covey DF, Steinbach JH (October 2007). "Neuroactive steroids and human recombinant rho1 GABAC receptors". The Journal of Pharmacology and Experimental Therapeutics. 323 (1): 236–47. doi:10.1124/jpet.107.127365. PMC 3905684. PMID 17636008. S2CID 12294587.
- ↑ Bullock AE, Clark AL, Grady SR, Robinson SF, Slobe BS, Marks MJ, et al. (June 1997). "Neurosteroids modulate nicotinic receptor function in mouse striatal and thalamic synaptosomes". Journal of Neurochemistry. 68 (6): 2412–23. doi:10.1046/j.1471-4159.1997.68062412.x. PMID 9166735. S2CID 26195479.
- ↑ Wetzel CH, Hermann B, Behl C, Pestel E, Rammes G, Zieglgänsberger W, et al. (September 1998). "Functional antagonism of gonadal steroids at the 5-hydroxytryptamine type 3 receptor". Molecular Endocrinology. 12 (9): 1441–51. doi:10.1210/mend.12.9.0163. PMID 9731711.
- 1 2 3 Mellon SH (October 2007). "Neurosteroid regulation of central nervous system development". Pharmacology & Therapeutics. 116 (1): 107–24. doi:10.1016/j.pharmthera.2007.04.011. PMC 2386997. PMID 17651807.
- ↑ Rupprecht R, Reul JM, Trapp T, van Steensel B, Wetzel C, Damm K, et al. (September 1993). "Progesterone receptor-mediated effects of neuroactive steroids". Neuron. 11 (3): 523–30. doi:10.1016/0896-6273(93)90156-l. PMID 8398145. S2CID 11205767.
- ↑ Reddy DS, Estes WA (July 2016). "Clinical Potential of Neurosteroids for CNS Disorders". Trends in Pharmacological Sciences. 37 (7): 543–561. doi:10.1016/j.tips.2016.04.003. PMC 5310676. PMID 27156439.
- 1 2 Thomas P, Pang Y (2012). "Membrane progesterone receptors: evidence for neuroprotective, neurosteroid signaling and neuroendocrine functions in neuronal cells". Neuroendocrinology. 96 (2): 162–71. doi:10.1159/000339822. PMC 3489003. PMID 22687885.
- ↑ Pang Y, Dong J, Thomas P (January 2013). "Characterization, neurosteroid binding and brain distribution of human membrane progesterone receptors δ and {epsilon} (mPRδ and mPR{epsilon}) and mPRδ involvement in neurosteroid inhibition of apoptosis". Endocrinology. 154 (1): 283–95. doi:10.1210/en.2012-1772. PMC 3529379. PMID 23161870.
- ↑ Sleiter N, Pang Y, Park C, Horton TH, Dong J, Thomas P, et al. (August 2009). "Progesterone receptor A (PRA) and PRB-independent effects of progesterone on gonadotropin-releasing hormone release". Endocrinology. 150 (8): 3833–44. doi:10.1210/en.2008-0774. PMC 2717864. PMID 19423765.
- ↑ Lamba V, Yasuda K, Lamba JK, Assem M, Davila J, Strom S, et al. (September 2004). "PXR (NR1I2): splice variants in human tissues, including brain, and identification of neurosteroids and nicotine as PXR activators". Toxicology and Applied Pharmacology. 199 (3): 251–65. doi:10.1016/j.taap.2003.12.027. PMID 15364541.
- ↑ Hu AQ, Wang ZM, Lan DM, Fu YM, Zhu YH, Dong Y, et al. (July 2007). "Inhibition of evoked glutamate release by neurosteroid allopregnanolone via inhibition of L-type calcium channels in rat medial prefrontal cortex". Neuropsychopharmacology. 32 (7): 1477–89. doi:10.1038/sj.npp.1301261. PMID 17151597.
- 1 2 3 Earl DE, Tietz EI (April 2011). "Inhibition of recombinant L-type voltage-gated calcium channels by positive allosteric modulators of GABAA receptors". The Journal of Pharmacology and Experimental Therapeutics. 337 (1): 301–11. doi:10.1124/jpet.110.178244. PMC 3063747. PMID 21262851.
- 1 2 Keitel V, Görg B, Bidmon HJ, Zemtsova I, Spomer L, Zilles K, et al. (November 2010). "The bile acid receptor TGR5 (Gpbar-1) acts as a neurosteroid receptor in brain". Glia. 58 (15): 1794–805. doi:10.1002/glia.21049. PMID 20665558. S2CID 37368754.
- 1 2 Bäckström T, Haage D, Löfgren M, Johansson IM, Strömberg J, Nyberg S, et al. (September 2011). "Paradoxical effects of GABA-A modulators may explain sex steroid induced negative mood symptoms in some persons". Neuroscience. 191: 46–54. doi:10.1016/j.neuroscience.2011.03.061. PMID 21600269. S2CID 38928854.
- 1 2 Andréen L, Nyberg S, Turkmen S, van Wingen G, Fernández G, Bäckström T (September 2009). "Sex steroid induced negative mood may be explained by the paradoxical effect mediated by GABAA modulators". Psychoneuroendocrinology. 34 (8): 1121–32. doi:10.1016/j.psyneuen.2009.02.003. PMID 19272715. S2CID 22259026.
- 1 2 Bäckström T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, et al. (February 2014). "Allopregnanolone and mood disorders". Progress in Neurobiology. 113: 88–94. doi:10.1016/j.pneurobio.2013.07.005. PMID 23978486. S2CID 207407084.
- ↑ Andréen L, Sundström-Poromaa I, Bixo M, Nyberg S, Bäckström T (August 2006). "Allopregnanolone concentration and mood--a bimodal association in postmenopausal women treated with oral progesterone". Psychopharmacology. 187 (2): 209–21. doi:10.1007/s00213-006-0417-0. PMID 16724185. S2CID 1933116.
- 1 2 3 4 5 Zorumski CF, Paul SM, Covey DF, Mennerick S (November 2019). "Neurosteroids as novel antidepressants and anxiolytics: GABA-A receptors and beyond". Neurobiology of Stress. 11: 100196. doi:10.1016/j.ynstr.2019.100196. PMC 6804800. PMID 31649968.
- ↑ Warner MD, Peabody CA, Whiteford HA, Hollister LE (April 1988). "Alprazolam as an antidepressant". The Journal of Clinical Psychiatry. 49 (4): 148–50. PMID 3281931.
- ↑ Srisurapanont M, Boonyanaruthee V (1997). "Alprazolam and standard antidepressants in the treatment of depression: a meta-analysis of the antidepressant effect". Journal of the Medical Association of Thailand = Chotmaihet Thangphaet. Centre for Reviews and Dissemination (UK). 80 (3): 183–188. PMID 9175386.
- ↑ Agís-Balboa RC, Pinna G, Zhubi A, Maloku E, Veldic M, Costa E, et al. (September 2006). "Characterization of brain neurons that express enzymes mediating neurosteroid biosynthesis". Proceedings of the National Academy of Sciences of the United States of America. 103 (39): 14602–7. Bibcode:2006PNAS..10314602A. doi:10.1073/pnas.0606544103. PMC 1600006. PMID 16984997.
- ↑ "Drug Approval Package: Zulresso". U.S. Food and Drug Administration (FDA). 7 February 2019. Archived from the original on 25 July 2020. Retrieved 6 August 2020.
- ↑ "Drug Trials Snapshots: Zulresso". U.S. Food and Drug Administration (FDA). 2 April 2019. Archived from the original on 28 September 2019. Retrieved 24 November 2019.
- ↑ "New Drug Therapy Approvals 2019". U.S. Food and Drug Administration. 31 December 2019. Archived from the original on 16 September 2020. Retrieved 15 September 2020.
- ↑ "INN Brexanolone". Archived from the original on 4 November 2021. Retrieved 3 September 2019.
- ↑ "KEGG DRUG: Brexanolone". Archived from the original on 25 July 2020. Retrieved 16 September 2021.
- ↑ "Brexanolone - Sage Therapeutics". AdisInsight. Archived from the original on 19 October 2021. Retrieved 16 September 2021.
- 1 2 Andréen L, Spigset O, Andersson A, Nyberg S, Bäckström T (June 2006). "Pharmacokinetics of progesterone and its metabolites allopregnanolone and pregnanolone after oral administration of low-dose progesterone". Maturitas. 54 (3): 238–44. doi:10.1016/j.maturitas.2005.11.005. PMID 16406399.
- ↑ Devinsky O, Schachter S, Pacia S (1 January 2005). Complementary and Alternative Therapies for Epilepsy. Demos Medical Publishing. pp. 378–. ISBN 978-1-934559-08-6. Archived from the original on 29 April 2016. Retrieved 16 September 2021.
- ↑ Saudan C, Desmarchelier A, Sottas PE, Mangin P, Saugy M (March 2005). "Urinary marker of oral pregnenolone administration". Steroids. 70 (3): 179–83. doi:10.1016/j.steroids.2004.12.007. PMID 15763596. S2CID 25490229.
- ↑ Piper T, Schlug C, Mareck U, Schänzer W (May 2011). "Investigations on changes in 13C/12C ratios of endogenous urinary steroids after pregnenolone administration". Drug Testing and Analysis. 3 (5): 283–90. doi:10.1002/dta.281. PMID 21538944.
- ↑ Sripada RK, Marx CE, King AP, Rampton JC, Ho SS, Liberzon I (June 2013). "Allopregnanolone elevations following pregnenolone administration are associated with enhanced activation of emotion regulation neurocircuits". Biological Psychiatry. 73 (11): 1045–53. doi:10.1016/j.biopsych.2012.12.008. PMC 3648625. PMID 23348009.
- ↑ Ducharme N, Banks WA, Morley JE, Robinson SM, Niehoff ML, Mattern C, et al. (September 2010). "Brain distribution and behavioral effects of progesterone and pregnenolone after intranasal or intravenous administration". European Journal of Pharmacology. 641 (2–3): 128–34. doi:10.1016/j.ejphar.2010.05.033. PMC 3008321. PMID 20570588.
Further reading
- Herd MB, Belelli D, Lambert JJ (October 2007). "Neurosteroid modulation of synaptic and extrasynaptic GABA(A) receptors". Pharmacology & Therapeutics. 116 (1): 20–34. arXiv:1607.02870. doi:10.1016/j.pharmthera.2007.03.007. PMID 17531325. Archived from the original on 9 March 2021. Retrieved 16 September 2021.
- Zorumski CF, Paul SM, Covey DF, Mennerick S (November 2019). "Neurosteroids as novel antidepressants and anxiolytics: GABA-A receptors and beyond". Neurobiology of Stress. 11: 100196. doi:10.1016/j.ynstr.2019.100196. PMC 6804800. PMID 31649968.
External links
| Identifiers: |
|---|
- "Brexanolone". Drug Information Portal. U.S. National Library of Medicine.