Tiotixene
 | |
| Names | |
|---|---|
| Trade names | Navane, others |
| Other names | Thiothixene, Thiothixene (USAN US) |
IUPAC name
| |
| Clinical data | |
| Drug class | Typical antipsychotic |
| Main uses | Psychoses such as schizophrenia[1] |
| Side effects | Sleepiness, movement disorders, dry mouth, low blood pressure, blurry vision[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth |
| Onset of action | Within 4 weeks[1] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682867 |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Metabolism | Liver |
| Elimination half-life | 10–20 hours |
| Chemical and physical data | |
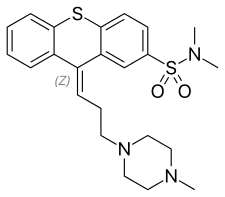
| Formula | C23H29N3O2S2 |
| Molar mass | 443.62 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Tiotixene, also known as thiothixene and sold under the brand name Navane among others, is a typical antipsychotic used to treat psychoses such as schizophrenia.[1] It is not useful for behavioral problems in intellectual disability.[1] It is taken by mouth.[1] Benefits generally begin within 4 weeks but maximal effect may take up to 6 months.[1]
Common side effects include sleepiness, movement disorders, dry mouth, low blood pressure, and blurry vision.[1] Other side effects include an increased risk of death in those with dementia, neuroleptic malignant syndrome, and allergic reactions.[1] It is in the thioxanthene family of chemicals and believed to work by inhibiting dopamine.[1]
Tiotixene was approved for medical use in the United States in 1967.[1] In the United States 30 pills of 10 mg costs about 30 USD.[2]
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Species | Ref |
|---|---|---|---|
| SERT | 3,162–3,878 | Human | [3][4] |
| NET | 30,200 | Human | [3][4] |
| DAT | 3,630 | Human | [3][4] |
| 5-HT1A | 410–912 | Human | [3][5][4] |
| 5-HT1B | 151 | Human | [3] |
| 5-HT1D | 659 | Human | [3] |
| 5-HT1E | >10,000 | Human | [3] |
| 5-HT2A | 50–89 | Human | [5][4] |
| 5-HT2C | 1,350–1,400 | Human | [5][4] |
| 5-HT3 | 1,860 | Human | [3][4] |
| 5-HT5A | 361 | Human | [3] |
| 5-HT6 | 208–320 | Human | [3][5][4] |
| 5-HT7 | 15.5 | Human | [3][5][4] |
| α1 | 19 | ND | [4] |
| α1A | 11–12 | Human | [3][5] |
| α1B | 35 | Human | [3] |
| α2 | 95 | ND | [4] |
| α2A | 80 | Human | [3][5] |
| α2B | 50 | Human | [3][5] |
| α2C | 52 | Human | [3][5] |
| β1 | >10,000 | Human | [3] |
| β2 | >10,000 | Human | [3] |
| D1 | 51–339 | Human | [3][4] |
| D2 | 0.03–1.4 | Human | [3][5][6] |
| D3 | 0.3–186 | Human | [6][4] |
| D4 | 203–363 | Human | [3][4] |
| D4.2 | 410–685 | Human | [6] |
| D5 | 261 | Human | [3] |
| H1 | 4.0–12 | Human | [3][5][7] |
| H2 | 411 | Human | [3] |
| H3 | 1,336 | Guinea pig | [3] |
| H4 | >10,000 | Human | [3] |
| mACh | 3,310 | ND | [4] |
| M1 | ≥2,820 | Human | [3][4] |
| M2 | ≥2,450 | Human | [3][4] |
| M3 | ≥5,750 | Human | [3][5][4] |
| M4 | >10,000 | Human | [3] |
| M5 | 5,376 | Human | [3] |
| σ | 1,780 | ND | [4] |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||
Tiotixene acts primarily as a highly potent antagonist of the dopamine D2 and D3 receptors (subnanomolar affinity).[3] It is also an antagonist of the histamine H1, α1-adrenergic, and serotonin 5-HT7 receptors (low nanomolar affinity), as well as of various other receptors to a much lesser extent (lower affinity).[3] It does not have any anticholinergic activity.[3] Antagonism of the D2 receptor is thought to be responsible for the antipsychotic effects of tiotixene.
Chemistry
Tiotixene is a member of the thioxanthene class of antipsychotics. Analogues include chlorprothixene, clopenthixol, flupentixol, and zuclopenthixol.
History
References
- 1 2 3 4 5 6 7 8 9 10 11 "Thiothixene Monograph for Professionals". Drugs.com. Archived from the original on 11 August 2020. Retrieved 3 October 2021.
- ↑ "Thiothixene Prices, Coupons & Savings Tips - GoodRx". GoodRx. Archived from the original on 8 May 2016. Retrieved 3 October 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 15 December 2019. Retrieved 14 August 2017.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Silvestre JS, Prous J (2005). "Research on adverse drug events. I. Muscarinic M3 receptor binding affinity could predict the risk of antipsychotics to induce type 2 diabetes". Methods Find Exp Clin Pharmacol. 27 (5): 289–304. doi:10.1358/mf.2005.27.5.908643. PMID 16082416.
- 1 2 3 4 5 6 7 8 9 10 11 12 Kroeze WK, Hufeisen SJ, Popadak BA, Renock SM, Steinberg S, Ernsberger P, Jayathilake K, Meltzer HY, Roth BL (2003). "H1-histamine receptor affinity predicts short-term weight gain for typical and atypical antipsychotic drugs". Neuropsychopharmacology. 28 (3): 519–26. doi:10.1038/sj.npp.1300027. PMID 12629531.
- 1 2 3 Burstein ES, Ma J, Wong S, Gao Y, Pham E, Knapp AE, Nash NR, Olsson R, Davis RE, Hacksell U, Weiner DM, Brann MR (2005). "Intrinsic efficacy of antipsychotics at human D2, D3, and D4 dopamine receptors: identification of the clozapine metabolite N-desmethylclozapine as a D2/D3 partial agonist". J. Pharmacol. Exp. Ther. 315 (3): 1278–87. doi:10.1124/jpet.105.092155. PMID 16135699. S2CID 2247093.
- ↑ Kanba S, Richelson E (1984). "Histamine H1 receptors in human brain labelled with [3H]doxepin". Brain Res. 304 (1): 1–7. doi:10.1016/0006-8993(84)90856-4. PMID 6146381. S2CID 45303586.
- ↑ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 3214–. ISBN 978-0-8155-1856-3. Archived from the original on 19 August 2020. Retrieved 17 July 2021.
- ↑ Edward Shorter (2009). Before Prozac: The Troubled History of Mood Disorders in Psychiatry. Oxford University Press, USA. pp. 51–. ISBN 978-0-19-536874-1. Archived from the original on 2020-08-19. Retrieved 2021-07-17.
External links
| Identifiers: |
|---|