Neuroleptic malignant syndrome
| Neuroleptic malignant syndrome | |
|---|---|
.jpg.webp) | |
| Haloperidol, a known cause | |
| Specialty | Critical care medicine, neurology, psychiatry |
| Symptoms | High fever, confusion, rigid muscles, variable blood pressure, sweating[1] |
| Complications | Rhabdomyolysis, high blood potassium, kidney failure, seizures[1][2] |
| Usual onset | Within a few weeks[3] |
| Causes | Neuroleptic or antipsychotic medication[1] |
| Risk factors | Dehydration, agitation, catatonia[4] |
| Diagnostic method | Based on symptoms in someone who has started neuroleptics within the last month[2] |
| Differential diagnosis | Heat stroke, malignant hyperthermia, serotonin syndrome, lethal catatonia[2] |
| Treatment | Stopping the offending medication, rapid cooling, starting other medications[2] |
| Medication | Dantrolene, bromocriptine, diazepam[2] |
| Prognosis | 10% risk of death[4] |
| Frequency | 15 per 100,000 per year (on neuroleptics)[1] |
Neuroleptic malignant syndrome (NMS) is a life-threatening reaction that can occur in response to neuroleptic or antipsychotic medication.[1] Symptoms include high fever, confusion, rigid muscles, variable blood pressure, sweating, and fast heart rate.[1] Complications may include rhabdomyolysis, high blood potassium, kidney failure, or seizures.[1][2]
Any medications within the family of neuroleptics can cause the condition, though typical antipsychotics appear to have a higher risk than atypicals.[1] Onset is often within a few weeks of starting the medication but can occur at any time.[1][3] Risk factors include dehydration, agitation, and catatonia.[4] Rapidly decreasing the use of levodopa may also trigger the condition.[1] The underlying mechanism involves blockage of dopamine receptors.[1] Diagnosis is based on symptoms.[2]
Management includes stopping the offending medication, rapid cooling, and starting other medications.[2] Medications used include dantrolene, bromocriptine, and diazepam.[2] The risk of death among those affected is about 10%.[4] Rapid diagnosis and treatment is required to improve outcomes.[1] Many people can eventually be restarted on a lower dose of antipsychotic.[2][3]
As of 2011, among those in psychiatric hospitals on neuroleptics about 15 per 100,000 are affected per year (0.015%).[1] In the second half of the 20th century rates were over 100 times higher at about 2% (2,000 per 100,000).[1] Males appear to be more often affected than females.[1] The condition was first described in 1956.[1]
Signs and symptoms
The first symptoms of neuroleptic malignant syndrome are usually muscle cramps and tremors, fever, symptoms of autonomic nervous system instability such as unstable blood pressure, and sudden changes in mental status (agitation, delirium, or coma). Once symptoms appear, they may progress rapidly and reach peak intensity in as little as three days. These symptoms can last anywhere from eight hours to forty days.[4]
Symptoms are sometimes misinterpreted by doctors as symptoms of mental illness which can result in delayed treatment.[5] NMS is less likely if a person has previously been stable for a period of time on antipsychotics, especially in situations where the dose has not been changed and there are no issues of noncompliance or consumption of psychoactive substances known to worsen psychosis.
- Increased body temperature >38 °C (>100.4 °F), or
- Confused or altered consciousness
- sweating
- Rigid muscles
- Autonomic imbalance
Causes
NMS is usually caused by antipsychotic drug use, and a wide range of drugs can result in NMS.[6] Individuals using butyrophenones (such as haloperidol and droperidol) or phenothiazines (such as promethazine and chlorpromazine) are reported to be at greatest risk. However, various atypical antipsychotics such as clozapine, olanzapine, risperidone, quetiapine, and ziprasidone have also been implicated in cases.[7]
NMS may also occur in people taking dopaminergic drugs (such as levodopa) for Parkinson's disease, most often when the drug dosage is abruptly reduced.[8] In addition, other drugs with anti-dopaminergic activity, such as the antiemetic metoclopramide, can induce NMS.[9] Tetracyclics with anti-dopaminergic activity have been linked to NMS in case reports, such as the amoxapines. Additionally, desipramine, dothiepin, phenelzine, tetrabenazine, and reserpine have been known to trigger NMS.[10] Whether lithium can cause NMS is unclear.[11]
At the molecular level, NMS is caused by a sudden, marked reduction in dopamine activity, either from withdrawal of dopaminergic agents or from blockade of dopamine receptors.
Risk factors
One of the clearest risk factors in the development of NMS is the course of drug therapy chosen to treat a condition. Use of high-potency neuroleptics, a rapid increase in the dosage of neuroleptics, and use of long-acting forms of neuroleptics are all known to increase the risk of developing NMS.[12]
It has been purported that there is a genetic risk factor for NMS, since identical twins have both presented with NMS in one case, and a mother and two of her daughters have presented with NMS in another case.[13]
Demographically, it appears that males, especially those under forty, are at greatest risk for developing NMS, although it is unclear if the increased incidence is a result of greater neuroleptic use in men under forty.[6] It has also been suggested that postpartum women may be at a greater risk for NMS.[14]
An important risk factor for this condition is Lewy body dementia. These patients are extremely sensitive to neuroleptics. As a result, neuroleptics should be used cautiously in all cases of dementia.[15]
Pathophysiology
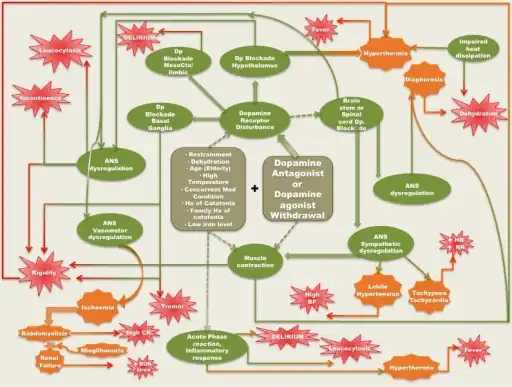
The mechanism is commonly thought to depend on decreased levels of dopamine activity due to:
- Dopamine receptor blockade
- Genetically reduced function of dopamine receptor D2[17]
It has been proposed that blockade of D2-like (D2, D3 and D4) receptors induce massive glutamate release, generating catatonia, neurotoxicity and myotoxicity.[18][19] Additionally, the blockade of diverse serotonin receptors by atypical antipsychotics and activation of 5HT1 receptors by certain of them reduces GABA release and indirectly induces glutamate release, worsening this syndrome.[20]
The muscular symptoms are most likely caused by blockade of the dopamine receptor D2, leading to abnormal function of the basal ganglia similar to that seen in Parkinson's disease.[21]
However, the failure of D2 dopamine receptor antagonism, or dopamine receptor dysfunction, do not fully explain the presenting symptoms and signs of NMS, as well as the occurrence of NMS with atypical antipsychotic drugs with lower D2 dopamine activity.[22] This has led to the hypothesis of sympathoadrenal hyperactivity (results from removing tonic inhibition from the sympathetic nervous system) as a mechanism for NMS.[23] Release of calcium is increased from the sarcoplasmic reticulum with antipsychotic usage. This can result in increased muscle contractility, which can play a role in the breakdown of muscle, muscle rigidity, and hyperthermia. Some antipsychotic drugs, such as typical neuroleptics, are known to block dopamine receptors; other studies have shown that when drugs supplying dopamine are withdrawn, symptoms similar to NMS present themselves.[4]
There is also thought to be considerable overlap between malignant catatonia and NMS in their pathophysiology, the former being idiopathic and the latter being the drug-induced form of the same syndrome.[24]
The raised white blood cell count and creatine phosphokinase (CPK) plasma concentration seen in those with NMS is due to increased muscular activity and rhabdomyolysis (destruction of muscle tissue).[25] The patient may suffer hypertensive crisis and metabolic acidosis. A non-generalized slowing on an EEG is reported in around 50% of cases.
The fever seen with NMS is believed to be caused by hypothalamic dopamine receptor blockade. The peripheral problems (the high white blood cell and CPK count) are caused by the antipsychotic drugs. They cause an increased calcium release from the sarcoplasmic reticulum of muscle cells which can result in rigidity and eventual cell breakdown. No major studies have reported an explanation for the abnormal EEG, but it is likely also attributable to dopamine blockage leading to changes in neuronal pathways.[6]
Diagnosis
Differential diagnosis
Differentiating NMS from other neurological disorders can be very difficult. It requires expert judgement to separate symptoms of NMS from other diseases. Some of the most commonly mistaken diseases are encephalitis, toxic encephalopathy, status epilepticus, heat stroke, and malignant hyperthermia. Due to the comparative rarity of NMS, it is often overlooked and immediate treatment for the syndrome is delayed. Drugs such as cocaine and amphetamine may also produce similar symptoms.[4][26]
The differential diagnosis is similar to that of hyperthermia, and includes serotonin syndrome.[27] Features which distinguish NMS from serotonin syndrome include bradykinesia, muscle rigidity, and a high white blood cell count.[28]
Treatment
NMS is a medical emergency and can lead to death if untreated. The first step is to stop the antipsychotic medication and treat the hyperthermia aggressively, such as with cooling blankets or ice packs to the axillae and groin. Supportive care in an intensive care unit capable of circulatory and ventilatory support is crucial. The best pharmacological treatment is still unclear. Dantrolene has been used when needed to reduce muscle rigidity, and more recently dopamine pathway medications such as bromocriptine have shown benefit.[29] Amantadine is another treatment option due to its dopaminergic and anticholinergic effects. Apomorphine may be used however its use is supported by little evidence.[21] Benzodiazepines may be used to control agitation. Highly elevated blood myoglobin levels can result in kidney damage, therefore aggressive intravenous hydration with diuresis may be required. When recognized early NMS can be successfully managed; however, up to 10% of cases can be fatal.[4]
Should the affected person subsequently require an antipsychotic, trialing a low dose of a low-potency atypical antipsychotic is recommended.[4]
Prognosis
The prognosis is best when identified early and treated aggressively. In these cases NMS is not usually fatal. In earlier studies the mortality rates from NMS ranged from 20%–38%, but by 2009 mortality rates were reported to have fallen below 10% over the previous two decades due to early recognition and improved management.[30] Re-introduction to the drug that originally caused NMS to develop may also trigger a recurrence, although in most cases it does not.
Memory impairment is a consistent feature of recovery from NMS, and is usually temporary though in some cases may become persistent.[31]
Epidemiology
Pooled data suggest the incidence of NMS is between 0.2%–3.23%.[32] However, greater physician awareness coupled with increased use of atypical anti-psychotics have likely reduced the prevalence of NMS.[6] Additionally, young males are particularly susceptible and the male:female ratio has been reported to be as high as 2:1.[6][32][33]
History
NMS was known about as early as 1956, shortly after the introduction of the first phenothiazines.[34] NMS was first described in 1960 by French clinicians who had been working on a study involving haloperidol. They characterized the condition that was associated with the side effects of haloperidol "syndrome malin des neuroleptiques", which was translated to neuroleptic malignant syndrome.[10]
Research
While the pathophysiology of NMS remains unclear, the two most prevalent theories are:
- Reduced dopamine activity due to receptor blockade
- Sympathoadrenal hyperactivity and autonomic dysfunction
In the past, research and clinical studies seemed to corroborate the D2 receptor blockade theory in which antipsychotic drugs were thought to significantly reduce dopamine activity by blocking the D2 receptors associated with this neurotransmitter. However, recent studies indicate a genetic component to the condition.[35] In support of the sympathoadrenal hyperactivity model proposed, it has been hypothesized that a defect in calcium regulatory proteins within the sympathetic neurons may bring about the onset of NMS.[36] This model of NMS strengthens its suspected association with malignant hyperthermia in which NMS may be regarded as a neurogenic form of this condition which itself is linked to defective calcium-related proteins.
The introduction of atypical antipsychotic drugs, with lower affinity to the D2 dopamine receptors, was thought to have reduced the incidence of NMS. However, recent studies suggest that the decrease in mortality may be the result of increased physician awareness and earlier initiation of treatment rather than the action of the drugs themselves.[22] NMS induced by atypical drugs also resembles "classical" NMS (induced by "typical" antipsychotic drugs), further casting doubt on the overall superiority of these drugs.[37]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Berman, BD (January 2011). "Neuroleptic malignant syndrome: a review for neurohospitalists". The Neurohospitalist. 1 (1): 41–7. doi:10.1177/1941875210386491. PMC 3726098. PMID 23983836.
- 1 2 3 4 5 6 7 8 9 10 "Neuroleptic Malignant Syndrome - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). 2004. Archived from the original on 19 February 2017. Retrieved 1 July 2017.
- 1 2 3 "Neuroleptic Malignant Syndrome Information Page | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 4 July 2017. Retrieved 1 July 2017.
- 1 2 3 4 5 6 7 8 9 Strawn JR, Keck PE, Caroff SN (2007). "Neuroleptic malignant syndrome". The American Journal of Psychiatry. 164 (6): 870–6. doi:10.1176/ajp.2007.164.6.870. PMID 17541044.
- ↑ Stacy Milbouer, "Quest for the truth", Nashua Telegraph http://www.nashuatelegraph.com/apps/pbcs.dll/article?AID=/20050424/NEWS01/104240081 Archived 2007-09-27 at the Wayback Machine
- 1 2 3 4 5 Neuroleptic Malignant Syndrome at eMedicine
- ↑ Khaldi S, Kornreich C, Choubani Z, Gourevitch R (2008). "Antipsychotiques atypiques et syndrome malin des neuroleptiques : brève revue de la littérature" [Neuroleptic malignant syndrome and atypical antipsychotics: A brief review] (PDF). L'Encéphale (in French). 34 (6): 618–24. doi:10.1016/j.encep.2007.11.007. PMID 19081460. Archived from the original on 2021-08-29. Retrieved 2019-12-11.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Keyser DL, Rodnitzky RL (1991). "Neuroleptic malignant syndrome in Parkinson's disease after withdrawal or alteration of dopaminergic therapy". Archives of Internal Medicine. 151 (4): 794–6. doi:10.1001/archinte.151.4.794. PMID 1672810.
- ↑ Friedman LS, Weinrauch LA, D'Elia JA (1987). "Metoclopramide-induced neuroleptic malignant syndrome". Archives of Internal Medicine. 147 (8): 1495–7. doi:10.1001/archinte.147.8.1495. PMID 3632154.
- 1 2 Buckley PF, Hutchinson M (1995). "Neuroleptic malignant syndrome". Journal of Neurology, Neurosurgery, and Psychiatry. 58 (3): 271–3. doi:10.1136/jnnp.58.3.271. PMC 1073359. PMID 7897404.
- ↑ Aronson, Jeffrey K. (2015). Meyler's Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. Elsevier. p. 607. ISBN 978-0-444-53716-4. Archived from the original on 2021-08-28. Retrieved 2020-01-13.
- ↑ Keck PE, Pope HG, Cohen BM, McElroy SL, Nierenberg AA (1989). "Risk factors for neuroleptic malignant syndrome. A case-control study". Archives of General Psychiatry. 46 (10): 914–8. doi:10.1001/archpsyc.1989.01810100056011. PMID 2572206.
- ↑ Otani K, Horiuchi M, Kondo T, Kaneko S, Fukushima Y (1991). "Is the predisposition to neuroleptic malignant syndrome genetically transmitted?". The British Journal of Psychiatry. 158 (6): 850–3. doi:10.1192/bjp.158.6.850. PMID 1678666.
- ↑ Alexander PJ, Thomas RM, Das A (1998). "Is risk of neuroleptic malignant syndrome increased in the postpartum period?". The Journal of Clinical Psychiatry. 59 (5): 254–5. doi:10.4088/JCP.v59n0509a. PMID 9632037.
- ↑ Steinberg, Martin; Lyketsos, Constantine G. (September 2012). "Atypical Antipsychotic Use in Patients With Dementia: Managing Safety Concerns". The American Journal of Psychiatry. 169 (9): 900–906. doi:10.1176/appi.ajp.2012.12030342. PMC 3516138. PMID 22952071.
- ↑ Tse, Lurdes; Barr, Alasdair M.; Scarapicchia, Vanessa; Vila-Rodriguez, Fidel (2015). "Neuroleptic Malignant Syndrome: A Review from a Clinically Oriented Perspective". Current Neuropharmacology. 13 (3): 395–406. doi:10.2174/1570159x13999150424113345. ISSN 1875-6190. Retrieved 4 December 2022.
- ↑ Mihara K, Kondo T, Suzuki A, Yasui-Furukori N, Ono S, Sano A, Koshiro K, Otani K, Kaneko S (2003). "Relationship between functional dopamine D2 and D3 receptors gene polymorphisms and neuroleptic malignant syndrome". American Journal of Medical Genetics Part B. 117B (1): 57–60. doi:10.1002/ajmg.b.10025. PMID 12555236.
- ↑ Kornhuber J, Weller M, Riederer P (1993). "Glutamate receptor antagonists for neuroleptic malignant syndrome and akinetic hyperthermic parkinsonian crisis". Journal of Neural Transmission. Parkinson's Disease and Dementia Section. 6 (1): 63–72. doi:10.1007/bf02252624. PMID 8105799.
- ↑ Chatterjee A (2014). "Glutamate-based magnetic resonance spectroscopy in neuroleptic malignant syndrome". Annals of Indian Academy of Neurology. 17 (1): 123–4. doi:10.4103/0972-2327.128579. PMC 3992752. PMID 24753679.
- ↑ Odagaki Y (2009). "Atypical neuroleptic malignant syndrome or serotonin toxicity associated with atypical antipsychotics?". Current Drug Safety. 4 (1): 84–93. CiteSeerX 10.1.1.334.241. doi:10.2174/157488609787354387. PMID 19149529.
- 1 2 "UpToDate". www.uptodate.com. Archived from the original on 2018-08-06. Retrieved 2019-08-17.
- 1 2 Ananth J, Parameswaran S, Gunatilake S, Burgoyne K, Sidhom T (2004). "Neuroleptic malignant syndrome and atypical antipsychotic drugs". The Journal of Clinical Psychiatry. 65 (4): 464–70. doi:10.4088/JCP.v65n0403. PMID 15119907. Archived from the original on 2021-08-28. Retrieved 2019-12-11.
- ↑ Gurrera RJ (1999). "Sympathoadrenal hyperactivity and the etiology of neuroleptic malignant syndrome". The American Journal of Psychiatry. 156 (2): 169–180. doi:10.1176/ajp.156.2.169 (inactive 2020-05-21). PMID 9989551. Archived from the original on 2020-02-23. Retrieved 2020-02-23.
{{cite journal}}: CS1 maint: DOI inactive as of May 2020 (link) - ↑ Northoff G (2002). "Catatonia and neuroleptic malignant syndrome: psychopathology and pathophysiology". Journal of Neural Transmission. 109 (12): 1453–67. CiteSeerX 10.1.1.464.9266. doi:10.1007/s00702-002-0762-z. PMID 12486486.
- ↑ Latham J, Campbell D, Nichols W, Mott T (2008). "How much can exercise raise creatine kinase level—and does it matter?". The Journal of Family Practice. 57 (8): 545–7. PMID 18687233. Archived from the original on 2016-06-01.
- ↑ Sachdev PS (2005). "A rating scale for neuroleptic malignant syndrome". Psychiatry Research. 135 (3): 249–56. doi:10.1016/j.psychres.2005.05.003. PMID 15996751.
- ↑ Christensen V, Glenthøj B (2001). "[Malignant neuroleptic syndrome or serotonergic syndrome]". Ugeskrift for Lægerer. 163 (3): 301–2. PMID 11219110.
- ↑ Birmes P, Coppin D, Schmitt L, Lauque D (2003). "Serotonin syndrome: a brief review". CMAJ. 168 (11): 1439–42. PMC 155963. PMID 12771076. Archived from the original on 2020-07-02. Retrieved 2016-04-30.
- ↑ Dhib-Jalbut S, Hesselbrock R, Mouradian MM, Means ED (1987). "Bromocriptine treatment of neuroleptic malignant syndrome". The Journal of Clinical Psychiatry. 48 (2): 69–73. PMID 3804991.
- ↑ Ahuja, N.; Cole, A. J. (2009). "Hyperthermia syndromes in psychiatry". Advances in Psychiatric Treatment. 15 (3): 181–91. doi:10.1192/apt.bp.107.005090.
- ↑ Mendhekar DN, Duggal HS (2006). "Persistent amnesia as a sequel of olanzapine-induced neuroleptic malignant syndrome". The Journal of Neuropsychiatry and Clinical Neurosciences. 18 (4): 552–3. doi:10.1176/jnp.2006.18.4.552. PMID 17135384.
- 1 2 Pelonero AL, Levenson JL, Pandurangi AK (1998). "Neuroleptic malignant syndrome: a review". Psychiatric Services. 49 (9): 1163–72. doi:10.1176/ps.49.9.1163. PMID 9735957.
- ↑ Hernández JL, Palacios-Araus L, Echevarría S, Herrán A, Campo JF, Riancho JA (1997). "Neuroleptic malignant syndrome in the acquired immunodeficiency syndrome". Postgraduate Medical Journal. 73 (866): 779–84. doi:10.1136/pgmj.73.866.779. PMC 2431511. PMID 9497946.
- ↑ Friedberg JM. Neuroleptic malignant syndrome. URL: "Archived copy". Archived from the original on October 16, 2006. Retrieved 2006-07-03.
{{cite web}}: CS1 maint: archived copy as title (link). Accessed: July 3, 2006. - ↑ Velamoor VR (1998). "Neuroleptic malignant syndrome. Recognition, prevention and management". Drug Safety. 19 (1): 73–82. doi:10.2165/00002018-199819010-00006. PMID 9673859.
- ↑ Gurrera RJ (2002). "Is neuroleptic malignant syndrome a neurogenic form of malignant hyperthermia?". Clinical Neuropharmacology. 25 (4): 183–93. doi:10.1097/00002826-200207000-00001. PMID 12151905.
- ↑ Hasan S, Buckley P (1998). "Novel antipsychotics and the neuroleptic malignant syndrome: a review and critique". The American Journal of Psychiatry. 155 (8): 1113–6. doi:10.1176/ajp.155.8.1113. PMID 9699705.
External links
- NINDS Neuroleptic Malignant Syndrome Information Page Archived 2017-07-04 at the Wayback Machine—NIH.
| Classification | |
|---|---|
| External resources |