Tetrabenazine
 | |
 | |
| Names | |
|---|---|
| Trade names | Xenazine, Xentra, Nitoman, others |
| Other names | Ro-1-9569 |
IUPAC name
| |
| Clinical data | |
| Drug class | Vesicular monoamine transporter 2 inhibitor[1] |
| Main uses | Certain movement disorders[1][2] |
| Side effects | Sleepiness, depression, irritability, poor balance, nausea, falls[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth (tablets) |
| External links | |
| AHFS/Drugs.com | Consumer Drug Information |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | Low, extensive first pass effect |
| Protein binding | 82–85% |
| Metabolism | Liver (CYP2D6-mediated) |
| Elimination half-life | 10 hours parent compound (2 to 8 hours active metabolites)[3] |
| Excretion | Kidney (~75%) and fecal (7–16%)[4] |
| Chemical and physical data | |
| Formula | C19H27NO3 |
| Molar mass | 317.429 g·mol−1 |
| 3D model (JSmol) | |
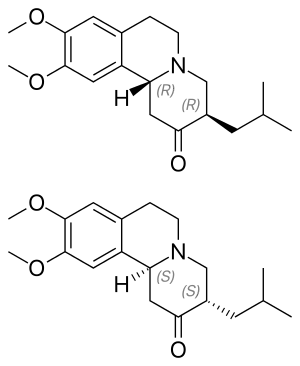
| Chirality | Racemic mixture |
SMILES
| |
InChI
| |
Tetrabenazine, sold under the brand name Xenazine among other, is a medication used to treat certain movement disorders, including Huntington chorea and tardive dyskinesia.[1][2] It is taken by mouth.[2]
Common side effects include sleepiness, depression, irritability, poor balance, nausea, and falls.[1] Other side effects may include high prolactin, low blood pressure, QT prolongation, neuroleptic malignant syndrome, and trouble swallowing.[1] It is a vesicular monoamine transporter 2 inhibitor.[1]
Tetrabenazine was approved for medical use in the United States in 2008.[1] It is available as a generic medication.[2] In the United Kingdom 112 tablets of 25 mg costs the NHS about 100 pounds as of 2021.[2] This amount in the United States costs about 1,500 USD.[5]
Medical uses
Tetrabenazine is used as a treatment, but not as a cure, for hyperkinetic disorders such as:[6][7]
- Huntington's disease – specifically, the chorea associated with it
- Tourette syndrome and other tic disorders
- Tardive dyskinesia,[8] a serious and sometimes irreversible side effect of long-term use of many antipsychotics, mainly typical antipsychotics
- Hemiballismus, spontaneous flinging limb movements due to contra-lateral subthalamic nucleus damage
Dosage
It is started at a dose of 12.5 to 25 mg once to three times per day and may be increased to a maximum of 200 mg per day.[2]
Side effects
The most common adverse reactions, which have occurred in at least 10% of subjects in studies and at least 5% greater than in subjects who received placebo, have been: sedation or somnolence, fatigue, insomnia, depression, suicidal thoughts, akathisia, anxiety and nausea.[4]
Warnings
There is a boxed warning associated with the use of tetrabenazine:[4]
- Increases the risk of depression and suicidal thoughts and behavior in patients with Huntington's disease
- Balance risks of depression and suicidality with the clinical need for control of chorea when considering the use of tetrabenazine
- Monitor patients for emergence or worsening of depression, suicidality or unusual changes in behavior
- Inform patients, caregivers and families of the risk of depression and suicidality and instruct to report behaviours of concern promptly to the treating physician
- Exercise caution when treating patients with a history of depression or prior suicide attempts or ideation
- Tetrabenazine is contraindicated in patients who are actively suicidal and in patients with untreated or inadequately treated depression
Pharmacology
The precise mechanism of action of tetrabenazine is unknown. Its anti-chorea effect is believed to be due to a reversible depletion of monoamines such as dopamine, serotonin, norepinephrine, and histamine from nerve terminals. Tetrabenazine reversibly inhibits vesicular monoamine transporter 2, resulting in decreased uptake of monoamines into synaptic vesicles, as well as depletion of monoamine storage.[4]
See also
References
- 1 2 3 4 5 6 7 8 "Tetrabenazine". drugs.com. American Society of Health-System Pharmacists. Archived from the original on 6 March 2021. Retrieved 1 October 2021.
- 1 2 3 4 5 6 BNF (80 ed.). BMJ Group and the Pharmaceutical Press. September 2020 – March 2021. p. 425. ISBN 978-0-85711-369-6.
{{cite book}}: CS1 maint: date format (link) - ↑ Yero, T.; Rey, J. A. (2008). "Tetrabenazine (Xenazine), An FDA-Approved Treatment Option For Huntington's Disease". P & T: A Peer-Reviewed Journal for Formulary Management. 33 (12): 690–694. PMC 2730806. PMID 19750050.
- 1 2 3 4 "Xenazine (tetrabenazine) Tablets, for Oral Use. Full Prescribing Information. Revised: 6/2015" (PDF). H. Lundbeck A/S. Archived (PDF) from the original on 31 July 2018. Retrieved 9 December 2015.
- ↑ "Tetrabenazine Generic Xenazine". Retrieved 1 October 2021.
- ↑ Jankovic J, Beach J (1997). "Long-term effects of tetrabenazine in hyperkinetic movement disorders". Neurology. 48 (2): 358–62. doi:10.1212/wnl.48.2.358. PMID 9040721. S2CID 33577525.
- ↑ Kenney C, Hunter C, Jankovic J (January 2007). "Long-term tolerability of tetrabenazine in the treatment of hyperkinetic movement disorders". Movement Disorders. 22 (2): 193–7. doi:10.1002/mds.21222. PMID 17133512. S2CID 22001960.
- ↑ Ondo WG, Hanna PA, Jankovic J (August 1999). "Tetrabenazine treatment for tardive dyskinesia: assessment by randomized videotape protocol". American Journal of Psychiatry. 156 (8): 1279–81. doi:10.1176/ajp.156.8.1279 (inactive 31 May 2021). PMID 10450276. Archived from the original on 15 December 2019. Retrieved 2 June 2021.
{{cite journal}}: CS1 maint: DOI inactive as of May 2021 (link)
External links
| Identifiers: |
|---|
- Xenazine prescribing information FDA Archived 2017-02-16 at the Wayback Machine
- NIMH Repository data sheet
- "Tetrabenazine" from HOPES: Huntington's Disease Outreach Project for Education at Stanford
- Detailed monograph on tetrabenazine on rxmed.com Archived 2016-01-11 at the Wayback Machine
- Information on tetrabenazine from netdoctor.co.uk Archived 2012-01-04 at the Wayback Machine