Zuclopenthixol
 | |
| Names | |
|---|---|
| Trade names | Clopixol, Cisordinol, others |
| Other names | Zuclopentixol |
IUPAC name
| |
| Clinical data | |
| Drug class | Typical antipsychotic[1] |
| Main uses | Schizophrenia and other psychoses.[1] |
| Side effects | Anxiety, depression, high blood sugar, liver problems, sexual dysfunction, trouble sleeping[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth, IM[1] |
| External links | |
| AHFS/Drugs.com | International Drug Names |
| Legal | |
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | 49% (by mouth) |
| Protein binding | 98% |
| Metabolism | Liver (CYP2D6 and CYP3A4-mediated) |
| Elimination half-life | 20 hours (by mouth), 19 days (IM) |
| Excretion | Feces |
| Chemical and physical data | |
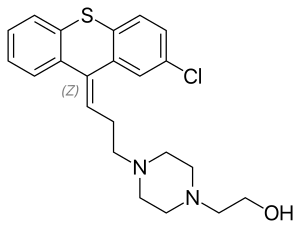
| Formula | C22H25ClN2OS |
| Molar mass | 400.97 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Zuclopenthixol , sold under the brand names Clopixol among others, is a medication used to treat schizophrenia and other psychoses.[1] Depending on the formulation it may be taken by mouth or by injection into a muscle.[1]
Side effects may include anxiety, depression, high blood sugar, liver problems, sexual dysfunction, and trouble sleeping.[1] Lower doses should be used in those with liver or kidney problems.[1] It is a typical antipsychotic.[1] It may be possible to use the medication while breastfeeding.[4]
Zuclopenthixol was isolated in 1962 and came into medical use in 1978.[5][6] It is approved for use in Australia, Canada, New Zealand, and the UK; though not the United States.[5][7][8] Some forms are available as a generic medication.[1] The long acting decanoate formulation is on the World Health Organization's List of Essential Medicines as an alternative to fluphenazine.[9] In the United Kingdom it is relatively inexpensive as of 2022.[1]
Medical uses
It is primarily used to treat schizophrenia and other psychoses.[1] It is also used in the treatment of acute bipolar mania.
Available forms
Zuclopenthixol is available in three major preparations:
- As zuclopenthixol decanoate (Clopixol Depot, Cisordinol Depot), it is a long-acting intramuscular injection. Its main use is as a long-acting injection given every two or three weeks to people with schizophrenia who have a poor compliance with medication and suffer frequent relapses of illness.[10] There is some evidence it may be more helpful in managing aggressive behaviour.[11]
- As zuclopenthixol acetate (Clopixol-Acuphase, Cisordinol-Acutard), it is a shorter-acting intramuscular injection used in the acute sedation of psychotic inpatients. The effect peaks at 48–72 hours providing 2–3 days of sedation.[12]
- As zuclopenthixol dihydrochloride (Clopixol, Cisordinol), it is a tablet used in the treatment of schizophrenia in those who are compliant with oral medication.[13]
Dosing
As a long-acting injection, zuclopenthixol decanoate comes in a 200 mg and 500 mg ampoule. Doses can vary from 50 mg weekly to the maximum licensed dose of 600 mg weekly. In general, the lowest effective dose to prevent relapse is preferred. The interval may be shorter as a patient starts on the medication before extending to 3 weekly intervals subsequently. The dose should be reviewed and reduced if side effects occur, though in the short-term an anticholinergic medication benztropine may be helpful for tremor and stiffness, while diazepam may be helpful for akathisia. 100 mg of zuclopenthixol decanoate is roughly equivalent to 20 mg of flupentixol decanoate or 12.5 mg of fluphenazine decanoate.
In acutely psychotic and agitated inpatients, 50 – 200 mg of zuclopenthixol acetate may be given for a calming effect over the subsequent three days, with a maximum dose of 400 mg in total to be given. As it is a long-acting medication, care must be taken not to give an excessive dose.
It is available in 2, 10, 25 and 40 mg tablets, with a dose range of 20–60 mg daily.[14]
Side effects
Long term zuclopenthixol (30 mg/kg/day for two years) in rats results in a small increases in thyroid parafollicular carcinomas and, in females, of mammary adenocarcinomas and of pancreatic islet cell adenomas and carcinomas. An increase in the incidence of mammary adenocarcinomas is a common finding for D2 antagonists which increase prolactin secretion when administered to rats. An increase in the incidence of pancreatic islet cell tumours has been observed for some other D2 antagonists. The physiological differences between rats and humans with regard to prolactin make the clinical significance of these findings unclear.
Withdrawal syndrome: Abrupt cessation of therapy may cause acute withdrawal symptoms (eg, nausea, vomiting, or insomnia). Symptoms usually begin in 1 to 4 days of withdrawal and subside within 1 to 2 weeks. Archived 2023-08-26 at the Wayback Machine Archived 2023-08-26 at the Wayback Machine
Other permanent side effects are similar to many other typical antipsychotics, namely extrapyramidal symptoms as a result of dopamine blockade in subcortical areas of the brain. This may result in symptoms similar to those seen in Parkinson's disease and include a restlessness and inability to sit still known as akathisia, a slow tremor and stiffness of the limbs.[13] Zuclopenthixol is thought to be more sedating than the related flupentixol, though possibly less likely to induce extrapyramidal symptoms than other typical depots.[10] As with other dopamine antagonists, zuclopenthixol may sometimes elevate prolactin levels; this may occasionally result in amenorrhoea or galactorrhoea in severe cases. Neuroleptic malignant syndrome is a rare but potentially fatal side effect. Any unexpected deterioration in mental state with confusion and muscle stiffness should be seen by a physician.
Zuclopenthixol decanoate induces a transient dose-dependent sedation. However, if the patient is switched to maintenance treatment with zuclopenthixol decanoate from oral zuclopenthixol or from i.m. zuclopenthixol acetate the sedation will be no problem. Tolerance to the unspecific sedative effect develops rapidly.[15]
- Very common (≥10% incidence) [16]
- Dry Mouth
- Somnolence
- Akathisia
- Hyperkinesia
- Hypokinesia
- Common (1%≤incidence≤10%) [16]
- Tachycardia
- Heart palpitations
- Vertigo
- Accommodation disorder
- Abnormal vision
- Salivary hypersecretion
- Constipation
- Vomiting
- Dyspepsia
- Diarrhoea
- Asthenia
- Fatigue
- Malaise
- Pain (at the injection site)
- Increased appetite
- Weight gain
- Myalgia
- Tremor
- Dystonia
- Hypertonia
- Dizziness
- Headache
- Paraesthesia
- Disturbance in attention
- Amnesia
- Abnormal gait
- Insomnia
- Depression
- Anxiety
- Abnormal dreams
- Agitation
- Decreased libido
- Nasal congestion
- Dyspnoea
- Hyperhidrosis
- Pruritus
- Uncommon (0.1%≤incidence≤1%)[16]
- Hyperacusis
- Tinnitus
- Mydriasis
- Abdominal pain
- Nausea
- Flatulence
- Thirst
- Injection site reaction
- Hypothermia
- Pyrexia
- Liver function test abnormal
- Decreased appetite
- Weight loss
- Muscle rigidity
- Trismus
- Torticollis
- Tardive dyskinesia
- Hyperreflexia
- Dyskinesia
- Parkinsonism
- Syncope
- Ataxia
- Speech disorder
- Hypotonia
- Convulsion
- Migraine
- Apathy
- Nightmares
- Libido increased
- Confused state
- Ejaculation failure
- Erectile dysfunction
- Female orgasmic disorder
- Vulvovaginal
- Dryness
- Rash
- Photosensitivity
- Pigmentation disorder
- Seborrhoea
- Dermatitis
- Purpura
- Hypotension
- Hot flush
- Rare (0.01%≤incidence≤0.1%)[16]
- Thrombocytopenia
- Neutropenia
- Leukopenia
- Agranulocytosis
- QT prolongation
- Hyperprolactinaemia
- Hypersensitivity
- Anaphylactic reaction
- Hyperglycaemia
- Glucose tolerance impaired
- Hyperlipidaemia
- Gynaecomastia
- Galactorrhoea
- Amenorrhoea
- Priapism
- Withdrawal symptoms
- Very rare (incidence<0.01%)[16]
Pharmacology
Pharmacodynamics

It is a D1 and D2 antagonist, α1-adrenergic and 5-HT2 antagonist.[17]
It has no affinity for muscarinic acetylcholine receptors. It weakly antagonises the histamine (H1) receptor but has no α2-adrenoceptor blocking activity .
Evidence from in vitro work and clinical sources (i.e. therapeutic drug monitoring databases) suggests that both CYP2D6 and CYP3A4 play important roles in zuclopenthixol metabolism.[18]
Pharmacokinetics
| Medication | Brand name | Class | Vehicle | Dosage | Tmax | t1/2 single | t1/2 multiple | logPc | Ref |
|---|---|---|---|---|---|---|---|---|---|
| Aripiprazole lauroxil | Aristada | Atypical | Watera | 441–1064 mg/4–8 weeks | 24–35 days | ? | 54–57 days | 7.9–10.0 | |
| Aripiprazole monohydrate | Abilify Maintena | Atypical | Watera | 300–400 mg/4 weeks | 7 days | ? | 30–47 days | 4.9–5.2 | |
| Bromperidol decanoate | Impromen Decanoas | Typical | Sesame oil | 40–300 mg/4 weeks | 3–9 days | ? | 21–25 days | 7.9 | [19] |
| Clopentixol decanoate | Sordinol Depot | Typical | Viscoleob | 50–600 mg/1–4 weeks | 4–7 days | ? | 19 days | 9.0 | [20] |
| Flupentixol decanoate | Depixol | Typical | Viscoleob | 10–200 mg/2–4 weeks | 4–10 days | 8 days | 17 days | 7.2–9.2 | [20][21] |
| Fluphenazine decanoate | Prolixin Decanoate | Typical | Sesame oil | 12.5–100 mg/2–5 weeks | 1–2 days | 1–10 days | 14–100 days | 7.2–9.0 | [22][23][24] |
| Fluphenazine enanthate | Prolixin Enanthate | Typical | Sesame oil | 12.5–100 mg/1–4 weeks | 2–3 days | 4 days | ? | 6.4–7.4 | [23] |
| Fluspirilene | Imap, Redeptin | Typical | Watera | 2–12 mg/1 week | 1–8 days | 7 days | ? | 5.2–5.8 | [25] |
| Haloperidol decanoate | Haldol Decanoate | Typical | Sesame oil | 20–400 mg/2–4 weeks | 3–9 days | 18–21 days | 7.2–7.9 | [26][27] | |
| Olanzapine pamoate | Zyprexa Relprevv | Atypical | Watera | 150–405 mg/2–4 weeks | 7 days | ? | 30 days | – | |
| Oxyprothepin decanoate | Meclopin | Typical | ? | ? | ? | ? | ? | 8.5–8.7 | |
| Paliperidone palmitate | Invega Sustenna | Atypical | Watera | 39–819 mg/4–12 weeks | 13–33 days | 25–139 days | ? | 8.1–10.1 | |
| Perphenazine decanoate | Trilafon Dekanoat | Typical | Sesame oil | 50–200 mg/2–4 weeks | ? | ? | 27 days | 8.9 | |
| Perphenazine enanthate | Trilafon Enanthate | Typical | Sesame oil | 25–200 mg/2 weeks | 2–3 days | ? | 4–7 days | 6.4–7.2 | [28] |
| Pipotiazine palmitate | Piportil Longum | Typical | Viscoleob | 25–400 mg/4 weeks | 9–10 days | ? | 14–21 days | 8.5–11.6 | [21] |
| Pipotiazine undecylenate | Piportil Medium | Typical | Sesame oil | 100–200 mg/2 weeks | ? | ? | ? | 8.4 | |
| Risperidone | Risperdal Consta | Atypical | Microspheres | 12.5–75 mg/2 weeks | 21 days | ? | 3–6 days | – | |
| Zuclopentixol acetate | Clopixol Acuphase | Typical | Viscoleob | 50–200 mg/1–3 days | 1–2 days | 1–2 days | 4.7–4.9 | ||
| Zuclopentixol decanoate | Clopixol Depot | Typical | Viscoleob | 50–800 mg/2–4 weeks | 4–9 days | ? | 11–21 days | 7.5–9.0 | |
| Note: All by intramuscular injection. Footnotes: a = Microcrystalline or nanocrystalline aqueous suspension. b = Low-viscosity vegetable oil (specifically fractionated coconut oil with medium-chain triglycerides). c = Predicted, from PubChem and DrugBank. Sources: Main: See template. | |||||||||
Chemistry
Chemically it is a thioxanthene. It is the cis-isomer of clopenthixol.[29]
History
Zuclopenthixol was introduced by Lundbeck in 1978.[30]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 BNF 83 (British National Formulary) March 2022 (83 ed.). Pharmaceutical Press. Aug 13 2022. p. 421. ISBN 9780857114341.
{{cite book}}: Check date values in:|date=(help) - ↑ "Clopixol (Zuclopenthixol Hydrochloride) Film-coated tablets". Australian Product Information. Australia: The Therapeutics Goods Administration. Archived from the original on 2018-06-15. Retrieved 2013-08-08.
- ↑ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in português do Brasil). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ↑ "Zuclopenthixol use while Breastfeeding". Drugs.com. Archived from the original on 24 September 2022. Retrieved 8 September 2023.
- 1 2 Meyer, Jonathan M.; Stahl, Stephen M. (2 September 2021). The Clinical Use of Antipsychotic Plasma Levels: Stahl's Handbooks. Cambridge University Press. p. 201. ISBN 978-1-009-00989-8. Archived from the original on 10 September 2023. Retrieved 8 September 2023.
- ↑ Riederer, Peter; Laux, Gerd; Nagatsu, Toshiharu; Le, Weidong; Riederer, Christian (4 November 2022). NeuroPsychopharmacotherapy. Springer Nature. p. 636. ISBN 978-3-030-62059-2. Archived from the original on 10 September 2023. Retrieved 8 September 2023.
- ↑ Green AI, Noordsy DL, Brunette MF, O'Keefe C (January 2008). "Substance abuse and schizophrenia: pharmacotherapeutic intervention". Journal of Substance Abuse Treatment. 34 (1): 61–71. doi:10.1016/j.jsat.2007.01.008. PMC 2930488. PMID 17574793.
- ↑ Sweetman, Sean C., ed. (2009). "Anxiolytic Sedatives Hypnotics and Antipsychotics". Martindale: The complete drug reference (36th ed.). London: Pharmaceutical Press. pp. 1040–1. ISBN 978-0-85369-840-1.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- 1 2 da Silva Freire Coutinho E, Fenton M, Quraishi SN (1999). "Zuclopenthixol decanoate for schizophrenia". The Cochrane Database of Systematic Reviews. John Wiley and Sons, Ltd. 1999 (2): CD001164. doi:10.1002/14651858.CD001164. PMC 7032616. PMID 10796607. Archived from the original on 2007-06-13. Retrieved 2007-06-12.
- ↑ Haessler F, Glaser T, Beneke M, Pap AF, Bodenschatz R, Reis O (2007). "Zuclopenthixol in adults with intellectual disabilities and aggressive behaviours". British Journal of Psychiatry. 190 (5): 447–448. doi:10.1192/bjp.bp.105.016535. PMID 17470962.
- ↑ Lundbeck P/L (1991). "Clopixol Acuphase 50 mg/mL Injection Clopixol Acuphase 100 mg / 2 mL Injection". Lundbeck P/L. Archived from the original on 2007-06-09. Retrieved 2007-06-12.
- 1 2 Bryan EJ, Purcell MA, Kumar A (November 2017). "Zuclopenthixol dihydrochloride for schizophrenia". The Cochrane Database of Systematic Reviews. 2017 (11): CD005474. doi:10.1002/14651858.CD005474.pub2. PMC 6486001. PMID 29144549.
- ↑ "Clopixol 2 mg film-coated tablets - Summary of Product Characteristics (SmPC) - (emc)". www.medicines.org.uk. Archived from the original on 2023-03-28. Retrieved 2023-03-28.
- ↑ "Summary of Product Characteristics" (PDF). Archived (PDF) from the original on 2017-03-28. Retrieved 2017-03-28.
- 1 2 3 4 5 "TGA eBS - Product and Consumer Medicine Information Licence". Archived from the original on 2018-06-15. Retrieved 2013-08-08.
- ↑ Christensen AV, Arnt J, Hyttel J, Larsen JJ, Svendsen O (April 1984). "Pharmacological effects of a specific dopamine D-1 antagonist SCH 23390 in comparison with neuroleptics". Life Sciences. 34 (16): 1529–1540. doi:10.1016/0024-3205(84)90607-6. PMID 6144029.
- ↑ Davies SJ, Westin AA, Castberg I, Lewis G, Lennard MS, Taylor S, Spigset O (2010). "Characterisation of zuclopenthixol metabolism by in vitro and therapeutic drug monitoring studies". Acta Psychiatrica Scandinavica. 122 (6): 445–453. doi:10.1111/j.1600-0447.2010.01619.x. PMID 20946203. S2CID 41869401.
- ↑ Parent M, Toussaint C, Gilson H (1983). "Long-term treatment of chronic psychotics with bromperidol decanoate: clinical and pharmacokinetic evaluation". Current Therapeutic Research. 34 (1): 1–6.
- 1 2 Jørgensen A, Overø KF (1980). "Clopenthixol and flupenthixol depot preparations in outpatient schizophrenics. III. Serum levels". Acta Psychiatrica Scandinavica. Supplementum. 279: 41–54. doi:10.1111/j.1600-0447.1980.tb07082.x. PMID 6931472.
- 1 2 Reynolds JE (1993). "Anxiolytic sedatives, hypnotics and neuroleptics.". Martindale: The Extra Pharmacopoeia (30th ed.). London: Pharmaceutical Press. pp. 364–623.
- ↑ Ereshefsky L, Saklad SR, Jann MW, Davis CM, Richards A, Seidel DR (May 1984). "Future of depot neuroleptic therapy: pharmacokinetic and pharmacodynamic approaches". The Journal of Clinical Psychiatry. 45 (5 Pt 2): 50–9. PMID 6143748.
- 1 2 Curry SH, Whelpton R, de Schepper PJ, Vranckx S, Schiff AA (April 1979). "Kinetics of fluphenazine after fluphenazine dihydrochloride, enanthate and decanoate administration to man". British Journal of Clinical Pharmacology. 7 (4): 325–31. doi:10.1111/j.1365-2125.1979.tb00941.x. PMC 1429660. PMID 444352.
- ↑ Young D, Ereshefsky L, Saklad SR, Jann MW, Garcia N (1984). Explaining the pharmacokinetics of fluphenazine through computer simulations. (Abstract.). 19th Annual Midyear Clinical Meeting of the American Society of Hospital Pharmacists. Dallas, Texas.
- ↑ Janssen PA, Niemegeers CJ, Schellekens KH, Lenaerts FM, Verbruggen FJ, van Nueten JM, et al. (November 1970). "The pharmacology of fluspirilene (R 6218), a potent, long-acting and injectable neuroleptic drug". Arzneimittel-Forschung. 20 (11): 1689–98. PMID 4992598.
- ↑ Beresford R, Ward A (January 1987). "Haloperidol decanoate. A preliminary review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in psychosis". Drugs. 33 (1): 31–49. doi:10.2165/00003495-198733010-00002. PMID 3545764.
- ↑ Reyntigens AJ, Heykants JJ, Woestenborghs RJ, Gelders YG, Aerts TJ (1982). "Pharmacokinetics of haloperidol decanoate. A 2-year follow-up". International Pharmacopsychiatry. 17 (4): 238–46. doi:10.1159/000468580. PMID 7185768.
- ↑ Larsson M, Axelsson R, Forsman A (1984). "On the pharmacokinetics of perphenazine: a clinical study of perphenazine enanthate and decanoate". Current Therapeutic Research. 36 (6): 1071–88.
- ↑ Sneader, Walter (2005). Drug discovery: a history. New York: Wiley. p. 410. ISBN 0-471-89980-1. Archived from the original on 2023-04-29. Retrieved 2020-10-07.
- ↑ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 1102–. ISBN 978-0-8155-1856-3. Archived from the original on 14 January 2023. Retrieved 27 September 2017.
External links
| Identifiers: |
|
|---|