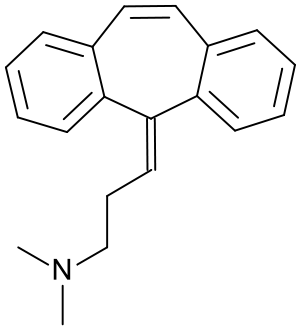
Cyclobenzaprine
 | |
 | |
| Names | |
|---|---|
| Trade names | Flexeril, Amrix, others |
IUPAC name
| |
| Clinical data | |
| Main uses | Muscle spasms[1] |
| Side effects | Headache, feeling tired, dizziness, dry mouth[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth |
| Defined daily dose | Not defined[3] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682514 |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | 33–55%[4][5] |
| Protein binding | 93% |
| Metabolism | Major: CYP3A4, CYP1A2; Minor: CYP2D6, N-demethylation[6] |
| Metabolites | Norcyclobenzaprine |
| Elimination half-life | 32 hours (range 8–37 hours)[7] |
| Excretion | Kidney |
| Chemical and physical data | |
| Formula | C20H21N |
| Molar mass | 275.395 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Cyclobenzaprine, sold under the brand name Flexeril among others, is a medication used for muscle spasms from musculoskeletal conditions of sudden onset.[1] It is not useful in cerebral palsy.[1] It is taken by mouth.[1] Use is not recommended for more than a few weeks.[1]
Common side effects include headache, feeling tired, dizziness, and dry mouth.[1] Serious side effects may include an irregular heart beat.[1] There is no evidence of harm in pregnancy, but it has not been well studied in this population.[1] It should not be used with an MAO inhibitor.[1] How it works is unclear.[1]
Cyclobenzaprine was approved for medical use in the United States in 1977.[1] It is available as a generic medication.[1] In the United States, the wholesale cost per dose is less than US$0.05 as of 2018.[8] In 2017, it was the 43rd most commonly prescribed medication in the United States, with more than 17 million prescriptions.[9][10] It was not available in the United Kingdom as of 2012.[11]
Medical use
Cyclobenzaprine is used to treat muscle spasms, in conjunction with physical therapy, that occur because of acute musculoskeletal conditions .[12] After sustaining an injury, painful muscle spasms may occur to stabilize the affected body part and prevent further damage. Cyclobenzaprine is used to treat such muscle spasms associated with acute, painful musculoskeletal conditions.[13] It decreases pain in the first two weeks,[14][15] peaking in the first few days, but has no proven benefit after two weeks.[14][16] Since no benefit is proven beyond that, therapy should not be continued long-term.[17] It is the best-studied muscle relaxer.[14] It is not useful for spasticity due to neurologic conditions such as cerebral palsy.[17][18]
A 2004 review found benefit for fibromyalgia symptoms, with a reported number needed to treat of 4.8 (meaning that 1 person out of every 4.8 benefits from treatment) for pain reduction, but no change in fatigue or tender points.[19] A 2009 Cochrane review found insufficient evidence to justify its use in myofascial pain syndrome.[20] It may also be used along with other treatments for tetanus.[21]
Dosage
The defined daily dose is not defined.[3]
Comparison to other medications
Cyclobenzaprine has been found to be not inferior to tizanidine, orphenadrine, and carisoprodol in the treatment of acute lower back pain, although none have been proven to be effective for long-term use (beyond two weeks of treatment). No differences in pain or spasm scores were noted among these agents, nor when compared to benzodiazepines.[22] However, nonbenzodiazepine (including cyclobenzaprine) treatment was found to have a lower risk of medication abuse and continuation of use against medical advice. Side effects such as sedation and ataxia are also less pronounced with nonbenzodiazepine antispasmodics.
Side effects
Cyclobenzaprine results in increased rates of drowsiness (38%), dry mouth (24%), and dizziness (10%).[16] Drowsiness and dry mouth appear to intensify with increasing dose.[23] Dysphagia, a life-threatening side-effect, may rarely occur.[24]
The sedative effects of cyclobenzaprine are likely due to its antagonistic effect on histamine, serotonin, and muscarinic receptors. Agitation is a common side effect observed especially in the elderly. In general, the National Committee for Quality Assurance recommends avoiding the use of cyclobenzaprine in the elderly because of the potential for more severe side effects.[25] Treatment protocols and support should follow the same as for any structurally related tricyclic, such as tricyclic antidepressants.[26]
Some experts believe that cyclobenzaprine should be avoided in elderly patients because it can cause confusion, delirium, and cognitive impairment.[27][28]
Overdose
The most common effects of overdose are drowsiness and tachycardia.[13] Rare but potentially critical complications are cardiac arrest, abnormal heart rhythms, severe low blood pressure, seizures, and neuroleptic malignant syndrome.[13] Life-threatening overdose is rare,[13] however, as the median lethal dose is about 338 milligrams/kilogram in mice and 425 mg/kg in rats.[13] The potential harm is increased when central nervous system depressants and antidepressants are also used; deliberate overdose often includes alcohol among other drugs.[13]
Interactions
Cyclobenzaprine has major contraindications with monoamine oxidase inhibitors (MAOIs). At least one study also found increased risk of serotonin syndrome when cyclobenzaprine was taken with the serotonergic drugs duloxetine or phenelzine.[29]
These substances may interact with cyclobenzaprine:
- Central nervous system depressants (e.g. alcohol, opioids, benzodiazepines, nonbenzodiazepines, phenothiazines, carbamates, barbiturates, major tranquilizers)
- Monoamine oxidase inhibitors taken within two weeks of cyclobenzaprine may result in serious, life-threatening side effects.[17]
Cyclobenzaprine may affect the medications used in surgical sedation and some surgeons request that patients temporarily discontinue its use prior to surgery.[30]
Pharmacology
Cyclobenzaprine is a centrally acting muscle relaxant.[31] Cyclobenzaprine is a 5HT2 receptor antagonist; it relieves muscle spasm through action on the central nervous system at the brain stem, rather than targeting the peripheral nervous system or muscles themselves.[32]
Pharmacokinetics
Cyclobenzaprine has an oral bioavailability of about 55% and approximately 93% is bound to proteins in plasma. The half-life of the drug is 18 hours and it has a plasma clearance of 0.7 litres per minute.[31][33][34]
Society and culture
Cost
In the United States, the wholesale cost per dose is less than US$0.05 as of 2018.[8] In 2017, it was the 43rd most commonly prescribed medication in the United States, with more than 17 million prescriptions.[9][10]
.svg.png.webp) Cyclobenzaprine costs (US)
Cyclobenzaprine costs (US).svg.png.webp) Cyclobenzaprine prescriptions (US)
Cyclobenzaprine prescriptions (US)
Formulations

By mouth, cyclobenzaprine is marketed as Apo-Cyclobenzaprin, Fexmid, Flexeril and Novo-Cycloprine. It is available in generic form. A once-a-day, extended-release formulation, Amrix, is available.[35] Cyclobenzaprine is also used by compounding pharmacies in topical creams.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Cyclobenzaprine Monograph for Professionals". Drugs.com. AHFS. Archived from the original on 23 December 2018. Retrieved 22 December 2018.
- ↑ "Cyclobenzaprine Use During Pregnancy". Drugs.com. Archived from the original on 2 June 2019. Retrieved 8 January 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 26 September 2020. Retrieved 9 September 2020.
- ↑ Micromedex® 2010 – DRUGDEX Evaluations (Cyclobenzaprine Hydrochloride)
- ↑ "Cyclobenzaprine Hydrochloride Tablets USP Revised: April 2005 Rx only". nih.gov. Archived from the original on 21 April 2016. Retrieved 1 October 2016.
- ↑ Teva Pharmaceuticals USA, Inc (May 2016). "AMR40470 (Amrix) Prescribing Information" (PDF). Archived (PDF) from the original on 22 December 2016. Retrieved 2 February 2017.
- ↑ Teva Pharmaceuticals USA, Inc (May 2016). "AMR40470 (Amrix) Prescribing Information" (PDF). Archived (PDF) from the original on 22 December 2016. Retrieved 2 February 2017.
- 1 2 "NADAC as of 2018-12-19". Centers for Medicare and Medicaid Services. Archived from the original on 19 December 2018. Retrieved 22 December 2018.
- 1 2 "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- 1 2 "Cyclobenzaprine - Drug Usage Statistics". ClinCalc. Archived from the original on 12 April 2020. Retrieved 11 April 2020.
- ↑ "Fibromyalgia, psychiatric comorbidity, and the somatosensory cortex". British Journal of Medical Practitioners. 5 (2): a522. 2012. Archived from the original on 23 December 2018. Retrieved 22 December 2018.
- ↑ Yang YW, Macdonald JB, Nelson SA, Sekulic A (December 2017). "Treatment of vismodegib-associated muscle cramps with cyclobenzaprine: A retrospective review". Journal of the American Academy of Dermatology. 77 (6): 1170–1172. doi:10.1016/j.jaad.2016.12.017. PMID 29132849.
- 1 2 3 4 5 6 "Flexeril (Cyclobenzaprine HCl) Tablets" (PDF). Food and Drug Administration. 2003. Archived (PDF) from the original on 16 October 2012. Retrieved 26 July 2009.
- 1 2 3 Chou R, Peterson K, Helfand M (August 2004). "Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review". Journal of Pain and Symptom Management. 28 (2): 140–75. doi:10.1016/j.jpainsymman.2004.05.002. PMID 15276195.
- ↑ van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM (2003). Van Tulder MW (ed.). "Muscle relaxants for non-specific low back pain". The Cochrane Database of Systematic Reviews. 2 (2): CD004252. doi:10.1002/14651858.CD004252. PMC 6464310. PMID 12804507.
- 1 2 Browning R, Jackson JL, O'Malley PG (July 2001). "Cyclobenzaprine and back pain: a meta-analysis". Archives of Internal Medicine. 161 (13): 1613–20. doi:10.1001/archinte.161.13.1613. PMID 11434793.
- 1 2 3 "Cyclobenzaprine official FDA information, side effects, and uses". Drugs.com. October 2009. Archived from the original on 6 March 2010. Retrieved 19 February 2010.
- ↑ Ashby P, Burke D, Rao S, Jones RF (October 1972). "Assessment of cyclobenzaprine in the treatment of spasticity". Journal of Neurology, Neurosurgery, and Psychiatry. 35 (5): 599–605. doi:10.1136/jnnp.35.5.599. PMC 494138. PMID 4563483.
- ↑ Tofferi JK, Jackson JL, O'Malley PG (February 2004). "Treatment of fibromyalgia with cyclobenzaprine: A meta-analysis". Arthritis and Rheumatism. 51 (1): 9–13. doi:10.1002/art.20076. PMID 14872449.
- ↑ Leite FM, Atallah AN, El Dib R, Grossmann E, Januzzi E, Andriolo RB, da Silva EM (July 2009). "Cyclobenzaprine for the treatment of myofascial pain in adults". The Cochrane Database of Systematic Reviews (3): CD006830. doi:10.1002/14651858.CD006830.pub3. PMC 6481902. PMID 19588406.
- ↑ Smith, Blaine T. (2014). Pharmacology for Nurses. Jones & Bartlett Publishers. p. 122. ISBN 9781449689407. Archived from the original on 3 October 2016. Retrieved 3 October 2016.
- ↑ "Medscape: Medscape Access". medscape.com. Archived from the original on 28 February 2015. Retrieved 1 October 2016.
- ↑ "Flexeril: Side effects". RxList.com. Archived from the original on 12 September 2008. Retrieved 22 February 2010.
- ↑ "MEDICATIONS AND DYSPHAGIA/ SWALLOWING RISKS" (PDF). Archived (PDF) from the original on 15 February 2017. Retrieved 2 February 2017.
- ↑ "High risk medications" (PDF). National Committee for Quality Assurance. Archived from the original (PDF) on 1 February 2010. Retrieved 22 February 2010.
- ↑ Chabria SB (July 2006). "Rhabdomyolysis: a manifestation of cyclobenzaprine toxicity". Journal of Occupational Medicine and Toxicology. 1 (1): 16. doi:10.1186/1745-6673-1-16. PMC 1540431. PMID 16846511.
- ↑ "Long-term Use of Cyclobenzaprine for Pain: A Review of the Clinical Effectiveness". CADTH Rapid Response Reports. Ottawa, Ontario: Canadian Agency for Drugs and Technologies in Health. 23 February 2015. PMID 25763449.
- ↑ Potentially inappropriate medications for the elderly according to the revised Beers criteria. 2012. Duke Clinical Research Institute website. Archived 12 August 2015 at the Wayback Machine http://www.americangeriatrics.org/files/documents/beers/2012AGSBeersCriteriaCitations.pdf%5B%5D
- ↑ Keegan MT, Brown DR, Rabinstein AA (December 2006). "Serotonin syndrome from the interaction of cyclobenzaprine with other serotoninergic drugs". Anesthesia and Analgesia. 103 (6): 1466–8. doi:10.1213/01.ane.0000247699.81580.eb. PMID 17122225.
- ↑ Medical Practice of William H. Gorman, M.D. (18 February 2014). "Medications to Avoid, Continue, or Stop - Before & After Surgery". Archived from the original on 1 December 2017. Retrieved 2 February 2017.
- 1 2 "Cyclobenzaprine". www.drugbank.ca. Archived from the original on 15 July 2020. Retrieved 22 January 2019.
- ↑ Kobayashi H, Hasegawa Y, Ono H (September 1996). "Cyclobenzaprine, a centrally acting muscle relaxant, acts on descending serotonergic systems". European Journal of Pharmacology. 311 (1): 29–35. doi:10.1016/0014-2999(96)00402-5. PMID 8884233.
- ↑ "Cyclobenzaprine". pubchem.ncbi.nlm.nih.gov. Archived from the original on 23 January 2019. Retrieved 22 January 2019.
- ↑ Winchell GA, King JD, Chavez-Eng CM, Constanzer ML, Korn SH (January 2002). "Cyclobenzaprine pharmacokinetics, including the effects of age, gender, and hepatic insufficiency". Journal of Clinical Pharmacology. 42 (1): 61–9. doi:10.1177/0091270002042001007. PMID 11808825.
- ↑ "Patient Web site for AMRIX® (Cyclobenzaprine Hydrochloride Extended‐Release Capsules)". amrix.com. Archived from the original on 4 October 2016. Retrieved 1 October 2016.
External links
| External sites: |
|
|---|---|
| Identifiers: |