Tension headache
| Tension headache | |
|---|---|
| Other names: Tension-type headache (TTH), stress headache, muscle contraction headache, psychomyogenic headache | |
 | |
| A woman experiencing a tension headache | |
| Specialty | Neurology |
| Symptoms | Mild to moderate head pain[1] |
| Complications | Mood disorders[1] |
| Duration | 30 min to 7 hours[1] |
| Types | Episodic, chronic[1] |
| Causes | Unclear[1] |
| Diagnostic method | Based on symptoms[1] |
| Differential diagnosis | Migraine, cluster headache, secondary headaches[1] |
| Prognosis | Usually good[1] |
| Frequency | 20%[1] |
Tension headache, also known as stress headache, is a common type of recurrent headache.[1] The pain is often band like, occurs on both sides, and is mild to moderate in intensity.[1] Generally the severity of the pain does not change with activity such as walking.[1] Often the pain is better in the morning and worse at night.[1] There may be associated neck or shoulder stiffness.[1] They can last from 30 minutes to 7 days.[1]
The cause is unclear though may involve environmental, genetic, and nutritional factors.[1] Psychological stress and posture appear to be related.[1] Diagnosis is based on the description of the symptoms, after ruling out other potential causes.[1] At least 10 episodes are required for an official diagnosis.[1]
Pain medication, specifically NSAIDs such as ibuprofen together with paracetamol (acetaminophine), are effective for the treatment of tension headache.[2][3][1] Frequent use of pain medications; however, can lead to medication overuse headaches.[1] Tricyclic antidepressants, such as amitriptyline, appear to be useful for prevention requiring about 4 weeks for a benefit.[4][1] Physical therapy and cognitive-behavioral therapy may also be useful.[1] Evidence is poor for SSRIs, propranolol and muscle relaxants.[5][6]
About 20% of people are affected in a given year and about 80% affected at some point in their life.[1] As of 2016, tension headaches affect about 1.89 billion people[7] and are more common in women than men (23% to 18% respectively).[8]
Signs and symptoms
For an official diagnosis the attacks must meet the following criteria:[9]
- A duration of between 30 minutes and 7 days.
- At least two of the following four characteristics:
- bilateral location
- pressing or tightening (non-pulsating) quality
- mild or moderate intensity
- not aggravated by routine physical activity such as walking or climbing stairs
- Both of the following:
- no nausea or vomiting
- no more than one of photophobia (sensitivity to bright light) or phonophobia (sensitivity to loud sounds)
Tension-type headaches may be accompanied by tenderness of the scalp on manual pressure during an attack.
Risk factors
Various precipitating factors may cause tension-type headaches in susceptible individuals:[10]
- Anxiety
- Stress
- Sleep problems
- Young age
- Poor health
Mechanism
Although the musculature of the head and neck and psychological factors such as stress may play a role in the overall pathophysiology of TTH, neither is currently believed to be the sole cause of the development of TTH.[11] The pathologic basis of TTH is most likely derived from a combination of personal factors, environmental factors, and alteration of both peripheral and central pain pathways.[12] Peripheral pain pathways receive pain signals from pericranial (around the head) myofascial tissue (protective tissue of muscles) and alteration of this pathway likely underlies episodic tension-type headache (ETTH).[12] In addition to these myofascial tissue pain signals, pericranial muscle tenderness, inflammation, and muscle ischemia have been postulated in headache literature to be causal factors in the peripheral pathophysiology of TTH.[10] However, multiple studies have failed to illustrate evidence for a pathologic role of either ischemia or inflammation within the muscles.[10] Pericranial tenderness is also not likely a peripheral causal factor for TTH, but may instead act to trigger a chronic pain cycle in which the peripheral pain response is transformed over time into a centralized pain response.[10] It is then these prolonged alterations in the peripheral pain pathways that lead to increased excitability of the central nervous system pain pathways, resulting in the transition of episodic tension-type headache into chronic tension type headache (CTTH).[12] Specifically, the hyperexcitability occurs in central nociceptive neurons (the trigeminal spinal nucleus, thalamus, and cerebral cortex) resulting in central sensitization, which manifests clinically as allodynia and hyperalgesia of CTTH.[10][13] Additionally, CTTH patients exhibit decreased thermal and pain thresholds which further bolsters support for central sensitization occurring in CTTH.[10]
The alterations in physiology that lead to overall process of central sensitization involve changes at the level of neural tracts, neurotransmitters and their receptors, the neural synapse, and the post-synaptic membrane. Evidence suggests dysfunction in supraspinal descending inhibitory pain pathways may contribute to the pathogenesis of central sensitization in CTTH.[10]
Neurotransmitters
Specific neuronal receptors and neurotransmitters thought to be most involved include NMDA and AMPA receptors, glutamate, serotonin (5-HT), β-endorphin, and nitric oxide (NO).[10] Of the neurotransmitters, NO plays a major role in central pain pathways and likely contributes to the process of central sensitization.[10] Briefly, the enzyme nitric oxide synthase (NOS) forms NO which ultimately results in vasodilatation and activation of central nervous system pain pathways.[10] Serotonin may also be of significant importance and involved in malfunctioning pain filter located in the brain stem. The view is that the brain misinterprets information—for example from the temporal muscle or other muscles—and interprets this signal as pain. Evidence for this theory comes from the fact that chronic tension-type headaches may be successfully treated with certain antidepressants such as nortriptyline. However, the analgesic effect of nortriptyline, as well as amitriptyline in chronic tension-type headache, is not solely due to serotonin reuptake inhibition, and likely other mechanisms are involved.[14][10]
Synapses
Regarding synaptic level changes, homosynaptic facilitation and heterosynaptic facilitation are both likely to be involved in central sensitization.[10] Homosynaptic facilitation occurs when synapses normally involved in pain pathways undergo changes involving receptors on the post-synaptic membrane as well as the molecular pathways activated upon synaptic transmission. Lower pain thresholds of CTTH result from this homosynaptic facilitation. In contrast, heterosynaptic facilitation occurs when synapses not normally involved in pain pathways become involved. Once this occurs innocuous signals are interpreted as painful signals. Allodynia and hyperalgesia of CTTH represent this heterosynaptic facilitation clinically.[10]
Stress
In the literature, stress is mentioned as a factor and may be implicated via the adrenal axis. This ultimately results in downstream activation of NMDA receptor activation, NFκB activation, and upregulation of iNOS with subsequent production of NO leading to pain as described above.[10]
Diagnosis
With tension headaches the physical exam is expected to be normal with perhaps the exception of either pericranial tenderness upon palpation of the cranial muscles, or presence of either photophobia or phonophobia.[15]
Classification
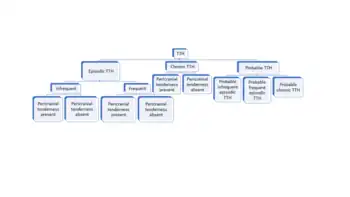
The International Headache Society's most current classification system for headache disorders is the International Classification of Headache Disorders 3rd edition (ICHD-3) as of 2018. This classification system separates tension-type headache (TTH) into two main groups: episodic (ETTH) and chronic (CTTH). CTTH is defined as fifteen days or more per month with headache for greater than three months, or one-hundred eighty days or more, with headache per year.[16] ETTH is less than fifteen days per month with headache or less than one-hundred eighty days with headache per year.[17][18] However, ETTH is further sub-divided into frequent and infrequent TTH.[19] Frequent TTH is defined as ten or more episodes of headache over the course of one to fourteen days per month for greater than three months, or at least twelve days per year, but less than one-hundred eighty days per year.[18] Infrequent TTH is defined as ten or more episodes of headache for less than one day per month or less than twelve days per year.[17] Furthermore, all sub-classes of TTH can be classified as having presence or absence of pericranial tenderness, which is tenderness of the muscles of the head.[19] Probable TTH is utilized for patients with some characteristics, but not all characteristics of a given sub-type of TTH.[20]
Differential diagnosis
Extensive testing is not needed as TTH is diagnosed by history and physical. However, if symptoms indicative of a more serious diagnosis are present, a contrast enhanced MRI may be utilized. Furthermore, giant cell arteritis should be considered in those 50 years of age and beyond. Screening for giant cell arteritis involves the blood tests of erythrocyte sedimentation rate (ESR) and c-reactive protein.[15]
- Migraine
- Oromandibular dysfunction
- Sinus disease
- Eye disease
- Cervical spine disease
- Infection
- Brain tumor
- Idiopathic intracranial hypertension
- Medication overuse headache
- Giant cell arteritis ( ≥50 years of age)
- Dermatochalasis
Prevention
Lifestyle
Drinking water and avoiding dehydration helps in preventing tension headache.[21] Using stress management and relaxing often makes headaches less likely.[21] Drinking alcohol can make headaches more likely or severe.[21] Good posture might prevent headaches if there is neck pain.[21] People who have jaw clenching might develop headaches, and getting treatment from a dentist might prevent those headaches.[21] Biofeedback techniques may also help.[22]
Medications
People who have 15 or more headaches in a month may be treated with certain types of daily antidepressants which act to prevent continued tension headaches from occurring.[21] In those who are predisposed to tension type headaches the first-line preventative treatment is amitriptyline, whereas mirtazapine and venlafaxine are second-line treatment options.[23] Tricyclic antidepressants appear to be useful for prevention.[4] Tricyclic antidepressants have been found to be more effective than SSRIs but have greater side effects.[4] Evidence is poor for the use of SSRIs, propranolol, and muscle relaxants for prevention of tension headaches.[5][6]
Treatment
Treatment for a current tension headache is to drink water and confirm that there is no dehydration.[21] If symptoms do not resolve within an hour for a person who has had water, then stress reduction might resolve the issue.[21]
Exercise
Evidence supports simple neck and shoulder exercises in managing ETTH and CTTH for headaches associated with neck pain. Exercises include stretching, strengthening and range of motion exercises. CTTH can also benefit from combined therapy from stress therapy, exercises and postural correction.[24]
Medications
Episodic
Over-the-counter drugs, like paracetamol, aspirin, or NSAIDs (ibuprofen, naproxen, ketoprofen), can be effective but tend to only be helpful as a treatment for a few times in a week at most.[2][21][25][12] For those with gastrointestinal problems (ulcers and bleeding), acetaminophen is the better choice over aspirin, though both provide roughly equivalent pain relief.[12] It is important to note that large daily doses of paracetamol should be avoided as it may cause liver damage especially in those that consume 3 or more drinks/day and those with pre-existing liver disease.[12] Ibuprofen, one of the NSAIDs listed above, is a common choice for pain relief but may also lead to gastrointestinal discomfort.[12]
Analgesic/sedative combinations are widely used (e.g., analgesic/antihistamine combinations, analgesic/barbiturate combinations such as Fiorinal).[3][23] In addition analgesic/caffeine combinations are popular such as the aspirin-caffeine combination or the aspirin, acetaminophen and caffeine combinations.[12] Frequent use (daily or skipping just one day in between use for 7–10 days) of any of the above analgesics may, however, lead to medication overuse headache.[3][23][12]
Muscle relaxants are typically used for and are helpful with acute post-traumatic TTH rather than ETTH.[12] Opioid medications are not utilized to treat ETTH.[12] Botulinum toxin does not appear to be helpful.[26]
Chronic
Classes of medications involved in treatment of CTTH include tricyclic antidepressants (TCAs), SSRIs, benzodiazepine (Clonazepam in small evening dose), and muscle relaxants. The most commonly utilized TCA is amitriptyline due to the postulated role in decreasing central sensitization and analgesic relief. Another popular TCA used is Doxepine. SSRIs may also be utilized for management of CTTH. For patients with concurrent muscle spasm and CTTH, the muscle relaxant Tizanidine can be a helpful option.[12]
These medications however, are not effective if concurrent overuse of over the counter medications or other analgesics is occurring.[12] Stopping overuse must occur prior to proceeding with other forms of treatment.[12]
Alternative medicine
Current evidence for acupuncture is slight. A 2016 systematic review suggests better evidence among those with frequent tension headaches, but concludes that further trials comparing acupuncture with other treatment options are needed.[27]
People with tension-type headache often use spinal manipulation, soft tissue therapy, and myofascial trigger point treatment. Studies of effectiveness are mixed. A 2006 systematic review found no rigorous evidence supporting manual therapies for tension headache.[28] A 2005 structured review found only weak evidence for the effectiveness of chiropractic manipulation for tension headache, and that it was probably more effective for tension headache than for migraine.[29] A 2004 Cochrane review found that spinal manipulation may be effective for tension headache.[30] Two other systematic reviews published between 2000 and May 2005 did not find conclusive evidence in favor of spinal manipulation.[31] A 2012 systematic review of manual therapy found that hands-on work may reduce both the frequency and the intensity of chronic tension-type headaches.[32] More current literature also appears to be mixed however, CTTH patients may benefit from massage and physiotherapy as suggested by a systemic review examining these modalities via RCTs specifically for this patient population[33] Despite being helpful, the review also makes a point to note that there is no difference in effectiveness long term (6 months) between those CTTH patients utilizing TCAs and physiotherapy.[33] Another systemic review comparing manual therapy to pharmacologic therapy also supports little long term difference in outcome regarding TTH frequency, duration, and intensity.[34]
Epidemiology
As of 2016 tension headaches affect about 1.89 billion people [35] and are more common in women than men (23% to 18% respectively).[8] Despite its benign character, tension-type headache, especially in its chronic form, can impart significant disability on patients as well as burden on society at large.[7]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Shah, N; Hameed, S (January 2020). "Muscle Contraction Tension Headache". PMID 32965945.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Derry S, Wiffen PJ, Moore RA, Bendtsen L (July 2015). "Ibuprofen for acute treatment of episodic tension-type headache in adults". The Cochrane Database of Systematic Reviews. 7 (7): CD011474. doi:10.1002/14651858.CD011474.pub2. PMC 6457940. PMID 26230487.
- 1 2 3 Loder E, Rizzoli P (January 2008). "Tension-type headache". BMJ. 336 (7635): 88–92. doi:10.1136/bmj.39412.705868.AD. PMC 2190284. PMID 18187725.
- 1 2 3 Jackson JL, Shimeall W, Sessums L, Dezee KJ, Becher D, Diemer M, Berbano E, O'Malley PG (October 2010). "Tricyclic antidepressants and headaches: systematic review and meta-analysis". BMJ. 341: c5222. doi:10.1136/bmj.c5222. PMC 2958257. PMID 20961988.
- 1 2 Verhagen AP, Damen L, Berger MY, Passchier J, Koes BW (April 2010). "Lack of benefit for prophylactic drugs of tension-type headache in adults: a systematic review". Family Practice. 27 (2): 151–65. doi:10.1093/fampra/cmp089. PMID 20028727.
- 1 2 Banzi R, Cusi C, Randazzo C, Sterzi R, Tedesco D, Moja L (May 2015). "Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) for the prevention of tension-type headache in adults". The Cochrane Database of Systematic Reviews. 5 (5): CD011681. doi:10.1002/14651858.CD011681. PMC 6864942. PMID 25931277.
- 1 2 Lenaerts ME (December 2006). "Burden of tension-type headache". Current Pain and Headache Reports. 10 (6): 459–62. doi:10.1007/s11916-006-0078-z. PMID 17087872.
- 1 2 Vos T, Flaxman AD (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMC 6350784. PMID 23245607.
- ↑ Headache Classification Committee of the International Headache Society (IHS): The International Classification of Headache Disorders,3rd edition. Cephalalgia 33(9) 629–808
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Chen, Yaniv (2009). "Advances in the pathophysiology of tension-type headache: From stress to central sensitization". Current Pain and Headache Reports. 13 (6): 484–494. doi:10.1007/s11916-009-0078-x. ISSN 1531-3433. PMID 19889292.
- 1 2 Walls, Ron; Hockberger, Robert; Gausche-Hill, Marianne (2017-03-09). Rosen's emergency medicine : concepts and clinical practice. Walls, Ron M.; Hockberger, Robert S.; Gausche-Hill, Marianne (Ninth ed.). Philadelphia, PA. p. 1269. ISBN 9780323390163. OCLC 989157341.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Jay GW, Barkin RL (December 2017). "Primary Headache Disorders- Part 2: Tension-type headache and medication overuse headache". Disease-A-Month. 63 (12): 342–367. doi:10.1016/j.disamonth.2017.05.001. PMID 28886861.
- ↑ Ashina S, Bendtsen L, Ashina M (December 2005). "Pathophysiology of tension-type headache". Current Pain and Headache Reports. 9 (6): 415–22. doi:10.1007/s11916-005-0021-8. PMID 16282042.
- ↑ Ashina M, Lassen LH, Bendtsen L, Jensen R, Olesen J (January 1999). "Effect of inhibition of nitric oxide synthase on chronic tension-type headache: a randomised crossover trial". Lancet. 353 (9149): 287–9. doi:10.1016/S0140-6736(98)01079-4. PMID 9929022.
- 1 2 3 Smith, Jonathan (2019). Ferri's Clinical Advisor. Philadelphia: Elsevier. p. 1348. ISBN 978-0-323-53042-2.
- ↑ Ihsclassification. "2.3 Chronic tension-type headache". ICHD-3 The International Classification of Headache Disorders 3rd edition. Archived from the original on 2019-01-13. Retrieved 2019-01-12.
- 1 2 Ihsclassification. "2.1 Infrequent episodic tension-type headache". ICHD-3 The International Classification of Headache Disorders 3rd edition. Archived from the original on 2019-01-13. Retrieved 2019-01-12.
- 1 2 Ihsclassification. "2.2 Frequent episodic tension-type headache". ICHD-3 The International Classification of Headache Disorders 3rd edition. Archived from the original on 2019-08-06. Retrieved 2019-01-12.
- 1 2 Ihsclassification. "2. Tension-type headache (TTH)". ICHD-3 The International Classification of Headache Disorders 3rd edition. Archived from the original on 2019-08-06. Retrieved 2019-01-12.
- ↑ Ihsclassification. "2.4 Probable tension-type headache". ICHD-3 The International Classification of Headache Disorders 3rd edition. Archived from the original on 2019-01-13. Retrieved 2019-01-12.
- 1 2 3 4 5 6 7 8 9 Consumer Reports (28 April 2016). "Tension Headache Treatment and Prevention". Consumer Reports. Archived from the original on 6 August 2019. Retrieved 25 May 2016.
- ↑ Nestoriuc Y, Rief W, Martin A (June 2008). "Meta-analysis of biofeedback for tension-type headache: efficacy, specificity, and treatment moderators". Journal of Consulting and Clinical Psychology. 76 (3): 379–96. doi:10.1037/0022-006X.76.3.379. PMID 18540732.
- 1 2 3 Bendtsen L, Jensen R (May 2011). "Treating tension-type headache -- an expert opinion". Expert Opinion on Pharmacotherapy. 12 (7): 1099–109. doi:10.1517/14656566.2011.548806. PMID 21247362.
- ↑ Varatharajan, Sharanya; Ferguson, Brad; Chrobak, Karen; Shergill, Yaadwinder; Côté, Pierre; Wong, Jessica J.; Yu, Hainan; Shearer, Heather M.; Southerst, Danielle; Sutton, Deborah; Randhawa, Kristi (July 2016). "Are non-invasive interventions effective for the management of headaches associated with neck pain? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration". European Spine Journal. 25 (7): 1971–1999. doi:10.1007/s00586-016-4376-9. ISSN 0940-6719. PMID 26851953.
- ↑ Derry S, Wiffen PJ, Moore RA (January 2017). "Aspirin for acute treatment of episodic tension-type headache in adults". The Cochrane Database of Systematic Reviews. 1: CD011888. doi:10.1002/14651858.CD011888.pub2. PMC 6464783. PMID 28084009.
- ↑ Simpson DM, Hallett M, Ashman EJ, Comella CL, Green MW, Gronseth GS, Armstrong MJ, Gloss D, Potrebic S, Jankovic J, Karp BP, Naumann M, So YT, Yablon SA (May 2016). "Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology. 86 (19): 1818–26. doi:10.1212/WNL.0000000000002560. PMC 4862245. PMID 27164716.
- ↑ Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin BC, Vickers A, White AR (April 2016). "Acupuncture for the prevention of tension-type headache". The Cochrane Database of Systematic Reviews. 4 (4): CD007587. doi:10.1002/14651858.CD007587.pub2. PMC 4955729. PMID 27092807.
- ↑ Fernández-de-Las-Peñas C, Alonso-Blanco C, Cuadrado ML, Miangolarra JC, Barriga FJ, Pareja JA (2006). "Are manual therapies effective in reducing pain from tension-type headache?: a systematic review". The Clinical Journal of Pain. 22 (3): 278–85. doi:10.1097/01.ajp.0000173017.64741.86. PMID 16514329.
- ↑ Biondi DM (June 2005). "Physical treatments for headache: a structured review". Headache. 45 (6): 738–46. doi:10.1111/j.1526-4610.2005.05141.x. PMID 15953306.
- ↑ Bronfort G, et al. (2004). Brønfort G (ed.). "Non-invasive physical treatments for chronic/recurrent headache". The Cochrane Database of Systematic Reviews (3): CD001878. doi:10.1002/14651858.CD001878.pub2. PMID 15266458. Archived from the original on 2021-08-29. Retrieved 2019-12-13.
- ↑ Ernst E, Canter PH (April 2006). "A systematic review of systematic reviews of spinal manipulation". Journal of the Royal Society of Medicine. 99 (4): 192–6. doi:10.1258/jrsm.99.4.192. PMC 1420782. PMID 16574972. Archived from the original on 2008-02-08. Retrieved 2009-02-03.
- ↑ Chaibi A, Russell MB (July 2012). "Manual therapies for cervicogenic headache: a systematic review". The Journal of Headache and Pain. 13 (5): 351–9. doi:10.1007/s10194-012-0436-7. PMC 3381059. PMID 22460941.
- 1 2 Chaibi A, Russell MB (October 2014). "Manual therapies for primary chronic headaches: a systematic review of randomized controlled trials". The Journal of Headache and Pain. 15: 67. doi:10.1186/1129-2377-15-67. PMC 4194455. PMID 25278005.
- ↑ Mesa-Jiménez JA, Lozano-López C, Angulo-Díaz-Parreño S, Rodríguez-Fernández ÁL, De-la-Hoz-Aizpurua JL, Fernández-de-Las-Peñas C (December 2015). "Multimodal manual therapy vs. pharmacological care for management of tension type headache: A meta-analysis of randomized trials". Cephalalgia. 35 (14): 1323–32. doi:10.1177/0333102415576226. PMID 25748428.
- ↑ Stovner, Lars Jacob; Nichols, Emma; Steiner, Timothy J.; Abd-Allah, Foad; Abdelalim, Ahmed; Al-Raddadi, Rajaa M.; Ansha, Mustafa Geleto; Barac, Aleksandra; Bensenor, Isabela M.; Doan, Linh Phuong; Edessa, Dumessa; Endres, Matthias; Foreman, Kyle J.; Gankpe, Fortune Gbetoho; Gopalkrishna, Gururaj; Goulart, Alessandra C.; Gupta, Rahul; Hankey, Graeme J.; Hay, Simon I.; Hegazy, Mohamed I.; Hilawe, Esayas Haregot; Kasaeian, Amir; Kassa, Dessalegn H.; Khalil, Ibrahim; Khang, Young-Ho; Khubchandan, Jagdish; Kim, Yun Jin; Kokubo, Yoshihiro; Mohammed, Mohammed A.; et al. (November 2018). "Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016". The Lancet. Neurology. 17 (11): 954–976. doi:10.1016/S1474-4422(18)30322-3. PMC 6191530. PMID 30353868.
External links
| Classification | |
|---|---|
| External resources |