Nifurtimox
 | |
 | |
| Names | |
|---|---|
| Trade names | Lampit[1] |
| Other names | Bayer 2502[1] |
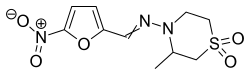
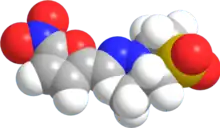
IUPAC name
| |
| Clinical data | |
| Drug class | Nitrofuran[2] |
| Main uses | Chagas disease, sleeping sickness[1][3] |
| Side effects | Abdominal pain, headache, nausea, weight loss[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Routes of use | By mouth |
| Defined daily dose | 0.7 g[4] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Bioavailability | Low |
| Metabolism | Liver (Cytochrome P450 oxidase (CYP) involved) |
| Elimination half-life | 2.95 ± 1.19 hours |
| Excretion | Kidney, very low |
| Chemical and physical data | |
| Formula | C10H13N3O5S |
| Molar mass | 287.29 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Melting point | 180 to 182 °C (356 to 360 °F) |
SMILES
| |
InChI
| |
Nifurtimox, sold under the brand name Lampit, is a medication used to treat Chagas disease and sleeping sickness.[1][3] For sleeping sickness it is used together with eflornithine in nifurtimox-eflornithine combination treatment.[3] In Chagas disease it is a second-line option to benznidazole.[2] It is given by mouth.[1]
Common side effects include abdominal pain, headache, nausea, and weight loss.[1] There are concerns from animal studies that it may increase the risk of cancer but these concerns have not be found in human trials.[2] Nifurtimox is not recommended in pregnancy or in those with significant kidney or liver problems.[2] It is a type of nitrofuran.[2]
Nifurtimox came into medication use in 1965.[2] It is on the World Health Organization's List of Essential Medicines.[3] It was approved for medical use in the United States in 2020.[6] It is not available commercially in Canada.[1] It cost about 20 USD for a course of treatment as of 2013.[7] In regions of the world where the disease is common nifurtimox is provided for free by the World Health Organization.[8]
Medical uses
Nifurtimox has been used to treat Chagas disease, when it is given for 30 to 60 days.[9][10] However, long-term use of nifurtimox does increase chances of adverse events like gastrointestinal and neurological side effects.[10][11] Due to the low tolerance and completion rate of nifurtimox, benznidazole is now being more considered for those who have Chagas disease and require long-term treatment.[2][11]
In the United States nifurtimox is indicated in children and adolescents (birth to less than 18 years of age and weighing at least 2.5 kilograms (5.5 lb) for the treatment of Chagas disease (American Trypanosomiasis), caused by Trypanosoma cruzi.[5]
Nifurtimox has also been used to treat African trypanosomiasis (sleeping sickness), and is active in the second stage of the disease (central nervous system involvement). When nifurtimox is given on its own, about half of all patients will relapse,[12] but the combination of melarsoprol with nifurtimox appears to be efficacious.[13] Trials are awaited comparing melarsoprol/nifurtimox against melarsoprol alone for African sleeping sickness.[14]
Combination therapy with eflornithine and nifurtimox is safer and easier than treatment with eflornithine alone, and appears to be equally or more effective. It has been recommended as first-line treatment for second-stage African trypanosomiasis.[15]
Pregnancy and breastfeeding
Use of nifurtimox should be avoided in pregnant women due to limited use.[2][10][16] There is limited data shown that nifurtimox doses up to 15 mg/kg daily can cause adverse effects in breastfed infants.[17] Other authors do not consider breastfeeding a contraindication during nifurtimox use.[17]
Dosage
The defined daily dose is 0.7 g (by mouth).[4]
Side effects
Side effects occur following chronic administration, particularly in elderly people. Major toxicities include immediate hypersensitivity such as anaphylaxis and delayed hypersensitivity reaction involving icterus and dermatitis. Central nervous system disturbances and peripheral neuropathy may also occur.[10]
Most common side effects[18][10][19][20][21]
- anorexia
- weight loss
- nausea
- vomiting
- headache
- dizziness
- amnesia
Less common effects[18][10][19][21]
- rash
- depression
- anxiety
- confusion
- fever
- sore throat
- chills
- seizures
- impotence
- tremors
- muscle weakness
- numbness of hands or feet
Contraindications
Nifurtimox is contraindicated in people with severe liver or kidney disease, as well as people with a background of neurological or psychiatric disorders.[2][18][22]
Mechanism of action
Nifurtimox forms a nitro-anion radical metabolite that reacts with nucleic acids of the parasite causing significant breakdown of DNA.[10] Its mechanism is similar to that proposed for the antibacterial action of nitrofuran agents. Nifurtimox undergoes reduction and creates oxygen radicals such as superoxide. These radicals are toxic to T. cruzi. Mammalian cells are protected by presence of catalase, glutathione, peroxidases, and superoxide dismutase. Accumulation of hydrogen peroxide to cytotoxic levels results in parasite death.[10]
Society and culture
.jpg.webp)
Nifurtimox is sold under the brand name Lampit by Bayer.[6] It was previously known as Bayer 2502.
Nifurtimox was only licensed for use in Argentina and Germany, where it is sold as 120-mg tablets. It was approved for medical use in the United States in August 2020.[6]
Research
Nifurtimox is in a phase-II clinical trial for the treatment of pediatric neuroblastoma and medulloblastoma.[23]
References
- 1 2 3 4 5 6 7 8 "Nifurtimox (Systemic)". Drugs.com. 1995. Archived from the original on 20 December 2016. Retrieved 3 December 2016.
- 1 2 3 4 5 6 7 8 9 Bern, Caryn; Montgomery, Susan P.; Herwaldt, Barbara L.; Rassi, Anis; Marin-Neto, Jose Antonio; Dantas, Roberto O.; Maguire, James H.; Acquatella, Harry; Morillo, Carlos (2007-11-14). "Evaluation and Treatment of Chagas Disease in the United States". JAMA. 298 (18): 2171–81. doi:10.1001/jama.298.18.2171. ISSN 0098-7484. PMID 18000201.
- 1 2 3 4 World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 29 October 2020. Retrieved 21 September 2020.
- 1 2 "Lampit (nifurtimox) tablets, for oral use" (PDF). U.S. Food and Drug Administration (FDA). Bayer HealthCare Pharmaceuticals Inc. Archived (PDF) from the original on 18 September 2020. Retrieved 6 August 2020.
- 1 2 3 4 "Lampit: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 20 October 2020. Retrieved 6 August 2020.
- ↑ Dumas, Michel; Bouteille, Bernard; Buguet, Alain (2013). Progress in Human African Trypanosomiasis, Sleeping Sickness. Springer Science & Business Media. p. 268. ISBN 9782817808574. Archived from the original on 2016-12-20.
- ↑ "Trypanosomiasis, human African (sleeping sickness)". World Health Organization. February 2016. Archived from the original on 4 December 2016. Retrieved 7 December 2016.
- ↑ Coura JR, de Castro SL (2002). "A critical review of Chagas disease chemotherapy". Mem Inst Oswaldo Cruz. 97 (1): 3–24. doi:10.1590/S0074-02762002000100001. PMID 11992141.
- 1 2 3 4 5 6 7 8 "Nifurtimox Drug Information, Professional". www.drugs.com. Archived from the original on 2016-11-08. Retrieved 2016-11-09.
- 1 2 Jackson, Yves; Alirol, Emilie; Getaz, Laurent; Wolff, Hans; Combescure, Christophe; Chappuis, François (2010-11-15). "Tolerance and Safety of Nifurtimox in Patients with Chronic Chagas Disease". Clinical Infectious Diseases. 51 (10): e69–e75. doi:10.1086/656917. ISSN 1058-4838. PMID 20932171. Archived from the original on 2021-08-29. Retrieved 2016-11-09.
- ↑ Pepin J, Milord F, Mpia B, et al. (1989). "An open clinical trial of nifurtimox for arseno-resistant T. b. gambiense sleeping sickness in central Zaire". Trans R Soc Trop Med Hyg. 83 (4): 514–7. doi:10.1016/0035-9203(89)90270-8. PMID 2694491.
- ↑ Bisser S, N'Siesi FX, Lejon V, et al. (2007). "Equivalence Trial of Melarsoprol and Nifurtimox Monotherapy and Combination Therapy for the Treatment of Second-Stage Trypanosoma brucei gambiense Sleeping Sickness". J Infect Dis. 195 (3): 322–329. doi:10.1086/510534. PMID 17205469.
- ↑ Pepin J (2007). "Combination Therapy for Sleeping Sickness: A Wake-Up Call". J Infect Dis. 195 (3): 311–13. doi:10.1086/510540. PMID 17205466.
- ↑ Priotto G, Kasparian S, Mutombo W, et al. (July 2009). "Nifurtimox-eflornithine combination therapy for second-stage African Trypanosoma brucei gambiense trypanosomiasis: a multicentre, randomised, phase III, non-inferiority trial". Lancet. 374 (9683): 56–64. doi:10.1016/S0140-6736(09)61117-X. hdl:10144/72797. PMID 19559476.
- ↑ Schaefer, Christof; Peters, Paul W. J.; Miller, Richard K. (2014-09-17). Drugs During Pregnancy and Lactation: Treatment Options and Risk Assessment. Academic Press. ISBN 9780124079014. Archived from the original on 2017-09-08.
- 1 2 "Nifurtimox use while Breastfeeding | Drugs.com". www.drugs.com. Archived from the original on 2016-11-08. Retrieved 2016-11-07.
- 1 2 3 "Parasites - American Trypanosomiasis (also known as Chagas Disease)". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 2016-11-06. Retrieved 2016-11-09.
- 1 2 Forsyth, Colin J.; Hernandez, Salvador; Olmedo, Wilman; Abuhamidah, Adieb; Traina, Mahmoud I.; Sanchez, Daniel R.; Soverow, Jonathan; Meymandi, Sheba K. (2016-10-15). "Safety Profile of Nifurtimox for Treatment of Chagas Disease in the United States". Clinical Infectious Diseases. 63 (8): 1056–1062. doi:10.1093/cid/ciw477. ISSN 1537-6591. PMC 5036918. PMID 27432838.
- ↑ Castro, José A.; de Mecca, Maria Montalto; Bartel, Laura C. (2006-08-01). "Toxic side effects of drugs used to treat Chagas' disease (American trypanosomiasis)". Human & Experimental Toxicology. 25 (8): 471–479. doi:10.1191/0960327106het653oa. ISSN 0960-3271. PMID 16937919.
- 1 2 Estani, Sergio Sosa; Segura, Elsa Leonor (1999-09-01). "Treatment of Trypanosoma cruzi infection in the undetermined phase. Experience and current guidelines of treatment in Argentina". Memórias do Instituto Oswaldo Cruz. 94: 363–365. doi:10.1590/S0074-02761999000700070. ISSN 0074-0276. PMID 10677756.
- ↑ "Chagas disease". World Health Organization. Archived from the original on 2014-02-27. Retrieved 2016-11-08.
- ↑ Clinical trial number NCT00601003 for "Study of Nifurtimox to Treat Refractory or Relapsed Neuroblastoma or Medulloblastoma" at ClinicalTrials.gov. Retrieved on July 10, 2009.
External links
| External sites: |
|
|---|---|
| Identifiers: |