Nitazoxanide
 | |
 | |
| Names | |
|---|---|
| Pronunciation | nye" ta zox' a nide[1] |
| Trade names | Alinia, Nizonide, others |
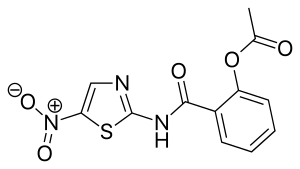
IUPAC name
| |
| Clinical data | |
| Drug class | Antiprotozoal[2] |
| Main uses | Cryptosporidiosis, giardiasis, amebiasis, isosporiasis, tapeworms, flukes, roundworms[2] |
| Side effects | Abdominal pain, nausea, headache, abnormally colored urine[2] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Routes of use | By mouth |
| Typical dose | 500 mg BID[2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603017 |
| Legal | |
| License data |
|
| Legal status | |
| Pharmacokinetics | |
| Protein binding | Nitazoxanide: ? Tizoxanide: over 99%[3][4] |
| Metabolism | Rapidly hydrolyzed to tizoxanide[3] |
| Metabolites | tizoxanide[3][4] tizoxanide glucuronide[3][4] |
| Elimination half-life | 3.5 hours[5] |
| Excretion | Kidney, bile duct, and fecal[3] |
| Chemical and physical data | |
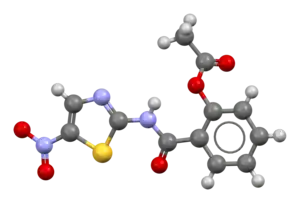
| Formula | C12H9N3O5S |
| Molar mass | 307.28 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Nitazoxanide, sold under the brand name Alinia among others, is a medication that is used to treat various protozoa and parasitic worms.[3][1] This includes cryptosporidiosis, giardiasis, amebiasis, isosporiasis, and certain tapeworms, flukes, and roundworms.[2] It is taken by mouth.[2]
Common side effects include abdominal pain, nausea, headache, and abnormally colored urine.[2] Safety in pregnancy is unclear.[2] It is a thiazolide and is believed to work by blocking pyruvate ferredoxin oxidoreductase.[1]
Nitazoxanide was approved for medical use in the United States in 2002.[2] It was approved as a generic medication in 2020.[6] In the United States 6 tablets of 500 mg costs about 240 USD as of 2021.[7] Research is ongoing as of 2021 with respect to its use for influenza.[8]
Medical uses
Nitazoxanide is an effective first-line treatment for infection by Blastocystis species[9][10] and is indicated for the treatment of infection by Cryptosporidium parvum or Giardia lamblia in immunocompetent adults and children.[3] It is also an effective treatment option for infections caused by other protozoa and helminths (e.g., Entamoeba histolytica,[11] Hymenolepis nana,[12] Ascaris lumbricoides,[13] and Cyclospora cayetanensis[14]).[15]
Nitazoxanide has also been shown to have in vitro antiparasitic activity and clinical treatment efficacy for infections caused by other protozoa and helminths;[15] evidence as of 2014 suggested that it possesses efficacy in treating a number of viral infections as well.[16]
Dosage
In adults it is often used at 500 mg twice per day.[2]
Contraindications
Nitazoxanide is contraindicated only in individuals who have experienced a hypersensitivity reaction to nitazoxanide or the inactive ingredients of a nitazoxanide formulation.[3]
Side effects
The side effects of nitazoxanide do not significantly differ from a placebo treatment for giardiasis;[3] these symptoms include stomach pain, headache, upset stomach, vomiting, discolored urine, excessive urinating, skin rash, itching, fever, flu syndrome, and others.[3][17] Nitazoxanide does not appear to cause any significant adverse effects when taken by healthy adults.[3][4]
Overdose
Information on nitazoxanide overdose is limited. Oral doses of 4 grams in healthy adults do not appear to cause any significant adverse effects.[3][4] In various animals, the oral LD50 is higher than 10 g/kg.[3]
Interactions
Due to the exceptionally high plasma protein binding (>99.9%) of nitazoxanide's metabolite, tizoxanide, the concurrent use of nitazoxanide with other highly plasma protein-bound drugs with narrow therapeutic indices (e.g., warfarin) increases the risk of drug toxicity.[3] In vitro evidence suggests that nitazoxanide does not affect the CYP450 system.[3]
Pharmacology
Pharmacodynamics
The anti-protozoal activity of nitazoxanide is believed to be due to interference with the pyruvate:ferredoxin oxidoreductase (PFOR) enzyme-dependent electron transfer reaction which is essential to anaerobic energy metabolism.[3][18] PFOR inhibition may also contribute to its activity against anaerobic bacteria.[19]
It has also been shown to have activity against influenza A virus in vitro.[20] The mechanism appears to be by selectively blocking the maturation of the viral hemagglutinin at a stage preceding resistance to endoglycosidase H digestion. This impairs hemagglutinin intracellular trafficking and insertion of the protein into the host plasma membrane.
Nitazoxanide modulates a variety of other pathways in vitro, including glutathione-S-transferase and glutamate-gated chloride ion channels in nematodes, respiration and other pathways in bacteria and cancer cells, and viral and host transcriptional factors.[19]
Pharmacokinetics
Following oral administration, nitazoxanide is rapidly hydrolyzed to the pharmacologically active metabolite, tizoxanide, which is 99% protein bound.[3][21] Tizoxanide is then glucuronide conjugated into the active metabolite, tizoxanide glucuronide.[3] Peak plasma concentrations of the metabolites tizoxanide and tizoxanide glucuronide are observed 1–4 hours after oral administration of nitazoxanide, whereas nitazoxanide itself is not detected in blood plasma.[3]
Roughly 2⁄3 of an oral dose of nitazoxanide is excreted as its metabolites in feces, while the remainder of the dose excreted in urine.[3] Tizoxanide is excreted in the urine, bile and feces.[3] Tizoxanide glucuronide is excreted in urine and bile.[3]
Chemistry
Nitazoxanide is the prototype member of the thiazolides, which is a drug class of structurally-related broad-spectrum antiparasitic compounds.[22] Nitazoxanide is a light yellow crystalline powder. It is poorly soluble in ethanol and practically insoluble in water.
History
Nitazoxanide was originally discovered in the 1980s by Jean-François Rossignol at the Pasteur Institute. Initial studies demonstrated activity versus tapeworms. In vitro studies demonstrated much broader activity. Dr. Rossignol co-founded Romark Laboratories, with the goal of bringing nitazoxanide to market as an anti-parasitic drug. Initial studies in the USA were conducted in collaboration with Unimed Pharmaceuticals, Inc. (Marietta, GA) and focused on development of the drug for treatment of cryptosporidiosis in AIDS. Controlled trials began shortly after the advent of effective anti-retroviral therapies. The trials were abandoned due to poor enrollment and the FDA rejected an application based on uncontrolled studies.
Subsequently, Romark launched a series of controlled trials. A placebo-controlled study of nitazoxanide in cryptosporidiosis demonstrated significant clinical improvement in adults and children with mild illness. Among malnourished children in Zambia with chronic cryptosporidiosis, a three-day course of therapy led to clinical and parasitologic improvement and improved survival. In Zambia and in a study conducted in Mexico, nitazoxanide was not successful in the treatment of cryptosporidiosis in advanced infection with human immunodeficiency virus at the doses used. However, it was effective in patients with higher CD4 counts. In treatment of giardiasis, nitazoxanide was superior to placebo and comparable to metronidazole. Nitazoxanide was successful in the treatment of metronidazole-resistant giardiasis. Studies have suggested efficacy in the treatment of cyclosporiasis, isosporiasis, and amebiasis.[23] Recent studies have also found it to be effective against beef tapeworm(Taenia saginata).[24]
Society and culture
Dosage forms
Nitazoxanide is currently available in two oral dosage forms: a tablet (500 mg) and an oral suspension (100 mg per 5 ml when reconstituted).[3]
An extended release tablet (675 mg) has been used in clinical trials for chronic hepatitis C; however, this form is not currently marketed and available for prescription.[25]
Brand names
Nitazoxanide is sold under the brand names Adonid, Alinia, Allpar, Annita, Celectan, Colufase, Daxon, Dexidex, Diatazox, Kidonax, Mitafar, Nanazoxid, Parazoxanide, Netazox, Niazid, Nitamax, Nitax, Nitaxide, Nitaz, Nizonide, NT-TOX, Pacovanton, Paramix, Toza, and Zox.
Research
As of September 2015, nitazoxanide was in phase 3 clinical trials for the treatment influenza due to its inhibitory effect on a broad range of influenza virus subtypes and efficacy against influenza viruses that are resistant to neuraminidase inhibitors like oseltamivir.[16][26] Nitazoxanide is also being researched as a potential treatment for COVID-19,[27] chronic hepatitis B, chronic hepatitis C, rotavirus and norovirus gastroenteritis.[16]
Hepatitis C
Romark initially decided to focus on the possibility of treating chronic hepatitis C with nitazoxanide.[25] The drug garnered interest from the hepatology community after three phase II clinical trials involving the treatment of hepatitis C with nitazoxanide produced positive results for treatment efficacy and similar tolerability to placebo without any signs of toxicity.[25] A meta-analysis from 2014 concluded that the previous held trials were of low-quality and with held with a risk of bias. The authors concluded that more randomized trials with low risk of bias are needed to determine if Nitazoxanide can be used as an effective treatment for chronic hepatitis C patients.[28]
References
- 1 2 3 "Nitazoxanide". LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases. 2012. Archived from the original on 13 November 2021. Retrieved 13 November 2021.
- 1 2 3 4 5 6 7 8 9 10 "Nitazoxanide Monograph for Professionals". Drugs.com. Archived from the original on 5 August 2020. Retrieved 13 November 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 "Alinia- nitazoxanide tablet Alinia- nitazoxanide powder, for suspension". DailyMed. Archived from the original on 20 March 2021. Retrieved 13 February 2021.
- 1 2 3 4 5 Stockis A, Allemon AM, De Bruyn S, Gengler C (May 2002). "Nitazoxanide pharmacokinetics and tolerability in man using single ascending oral doses". Int J Clin Pharmacol Ther. 40 (5): 213–220. doi:10.5414/cpp40213. PMID 12051573.
- ↑ "Nitazoxanide". PubChem Compound. National Center for Biotechnology Information. Archived from the original on 6 March 2016. Retrieved 3 January 2016.
- ↑ "First Generic Drug Approvals". U.S. Food and Drug Administration (FDA). Archived from the original on 26 January 2021. Retrieved 13 February 2021.
- ↑ "Nitazoxanide Prices and Nitazoxanide Coupons - GoodRx". GoodRx. Archived from the original on 1 November 2016. Retrieved 13 November 2021.
- ↑ "Nitazoxanide". SPS - Specialist Pharmacy Service. 14 January 2016. Archived from the original on 13 November 2021. Retrieved 13 November 2021.
- ↑ "Blastocystis: Resources for Health Professionals". United States Centers for Disease Control and Prevention. 2017-05-02. Archived from the original on 2015-11-08. Retrieved 4 January 2016.
- ↑ Roberts T, Stark D, Harkness J, Ellis J (May 2014). "Update on the pathogenic potential and treatment options for Blastocystis sp". Gut Pathog. 6: 17. doi:10.1186/1757-4749-6-17. PMC 4039988. PMID 24883113.
Blastocystis is one of the most common intestinal protists of humans. ... A recent study showed that 100% of people from low socio-economic villages in Senegal were infected with Blastocystis sp. suggesting that transmission was increased due to poor hygiene sanitation, close contact with domestic animals and livestock, and water supply directly from well and river [10]. ...
Table 2: Summary of treatments and efficacy for Blastocystis infection{{cite journal}}: External link in|quote= - ↑ Muñoz P, Valerio M, Eworo A, Bouza E (2011). "Parasitic infections in solid-organ transplant recipients". Curr Opin Organ Transplant. 16 (6): 565–575. doi:10.1097/MOT.0b013e32834cdbb0. PMID 22027588. S2CID 23861504. Archived from the original on 30 June 2016. Retrieved 7 January 2016.
Nitazoxanide: intestinal amoebiasis: 500 mg po bid x 3 days
- ↑ "Hymenolepiasis: Resources for Health Professionals". United States Centers for Disease Control and Prevention. 2017-05-02. Archived from the original on 2016-01-20. Retrieved 4 January 2016.
- ↑ Hagel I, Giusti T (October 2010). "Ascaris lumbricoides: an overview of therapeutic targets". Infectious Disorders Drug Targets. 10 (5): 349–67. doi:10.2174/187152610793180876. PMID 20701574. S2CID 15403331. Archived from the original on 2021-10-28. Retrieved 2021-10-04.
new anthelmintic alternatives such as tribendimidine and Nitazoxanide have proved to be safe and effective against A. lumbricoides and other soil-transmitted helminthiases in human trials.
- ↑ Shoff WH (5 October 2015). Chandrasekar PH, Talavera F, King JW (eds.). "Cyclospora Medication". Medscape. WebMD. Archived from the original on 6 September 2015. Retrieved 11 January 2016.
Nitazoxanide, a 5-nitrothiazole derivative with broad-spectrum activity against helminths and protozoans, has been shown to be effective against C cayetanensis, with an efficacy 87% by the third dose (first, 71%; second 75%). Three percent of patients had minor side effects.
- 1 2 Anderson, V. R.; Curran, M. P. (2007). "Nitazoxanide: A review of its use in the treatment of gastrointestinal infections". Drugs. 67 (13): 1947–1967. doi:10.2165/00003495-200767130-00015. PMID 17722965.
Nitazoxanide is effective in the treatment of protozoal and helminthic infections ... Nitazoxanide is a first-line choice for the treatment of illness caused by C. parvum or G. lamblia infection in immunocompetent adults and children, and is an option to be considered in the treatment of illnesses caused by other protozoa and/or helminths.
- ↑ "Nitazoxanide". MedlinePlus. Archived from the original on 10 April 2014. Retrieved 9 April 2014.
- ↑ Sisson G1, Goodwin A, Raudonikiene A, Hughes NJ, Mukhopadhyay AK, Berg DE, Hoffman PS. (July 2002). "Enzymes associated with reductive activation and action of nitazoxanide, nitrofurans, and metronidazole in Helicobacter pylori". Antimicrob. Agents Chemother. 46 (7): 2116–23. doi:10.1128/aac.46.7.2116-2123.2002. PMC 127316. PMID 12069963.
Nitazoxanide (NTZ) is a redox-active nitrothiazolyl-salicylamide
{{cite journal}}: CS1 maint: uses authors parameter (link) - 1 2 Shakya, A; Bhat, HR; Ghosh, SK (2018). "Update on Nitazoxanide: A Multifunctional Chemotherapeutic Agent". Current Drug Discovery Technologies. 15 (3): 201–213. doi:10.2174/1570163814666170727130003. PMID 28748751.
- ↑ Rossignol, J. F.; La Frazia, S.; Chiappa, L.; Ciucci, A.; Santoro, M. G. (2009). "Thiazolides, a New Class of Anti-influenza Molecules Targeting Viral Hemagglutinin at the Post-translational Level". Journal of Biological Chemistry. 284 (43): 29798–29808. doi:10.1074/jbc.M109.029470. PMC 2785610. PMID 19638339.
- ↑ Korba BE, Montero AB, Farrar K, et al. (January 2008). "Nitazoxanide, tizoxanide and other thiazolides are potent inhibitors of hepatitis B virus and hepatitis C virus replication". Antiviral Res. 77 (1): 56–63. doi:10.1016/j.antiviral.2007.08.005. PMID 17888524.
- ↑
- ↑ White Jr, AC (2003). "Nitazoxanide: An important advance in anti-parasitic therapy". Am. J. Trop. Med. Hyg. 68 (4): 382–383. doi:10.4269/ajtmh.2003.68.382. PMID 12875283.
- ↑ Lateef, M.; Zargar, S. A.; Khan, A. R.; Nazir, M.; Shoukat, A. (2008). "Successful treatment of niclosamide- and praziquantel-resistant beef tapeworm infection with nitazoxanide". International Journal of Infectious Diseases. 12 (1): 80–2. doi:10.1016/j.ijid.2007.04.017. PMID 17962058.
- 1 2 3 Keeffe, E. B.; Rossignol, J. F. (2009). "Treatment of chronic viral hepatitis with nitazoxanide and second generation thiazolides". World Journal of Gastroenterology. 15 (15): 1805–1808. doi:10.3748/wjg.15.1805. PMC 2670405. PMID 19370775.
- ↑ Li TC, Chan MC, Lee N (September 2015). "Clinical Implications of Antiviral Resistance in Influenza". Viruses. 7 (9): 4929–4944. doi:10.3390/v7092850. PMC 4584294. PMID 26389935.
Oral nitazoxanide is an available, approved antiparasitic agent (e.g., against cryptosporidium, giardia) with established safety profiles. Recently, it has been shown (together with its active metabolite tizoxanide) to possess anti-influenza activity by blocking haemagglutinin maturation/trafficking, and acting as an interferon-inducer [97]. ... A large, multicenter, Phase 3 randomized-controlled trial comparing nitazoxanide, oseltamivir, and their combination in uncomplicated influenza is currently underway (NCT01610245).
Figure 1: Molecular targets and potential antiviral treatments against influenza virus infection Archived 2021-10-28 at the Wayback Machine - ↑ Pepperrell, Toby (2020). "Review of safety and minimum pricing of nitazoxanide for potential treatment of COVID-19". Journal of Virus Eradication. 6 (2): 52–60. doi:10.1016/S2055-6640(20)30017-0. PMC 7332204. PMID 32405422.
- ↑ Nikolova, Kristiana; Gluud, Christian; Grevstad, Berit; Jakobsen, Janus C (2014). "Nitazoxanide for chronic hepatitis C". Cochrane Database of Systematic Reviews (4): CD009182. doi:10.1002/14651858.CD009182.pub2. ISSN 1465-1858. PMID 24706397.
External links
- "Parasitic infections". Am J Transplant. 4 (Suppl 10): 142–55. October 2004. doi:10.1111/j.1600-6135.2004.00677.x. PMID 15504227. S2CID 5742723.
| External sites: |
|
|---|---|
| Identifiers: |