Neostigmine
 | |
 | |
| Names | |
|---|---|
| Trade names | Bloxiverz, Prostigmin, Vagostigmin, others |
IUPAC name
| |
| Clinical data | |
| Drug class | Acetylcholinesterase inhibitor[1] |
| Main uses | Myasthenia gravis, Ogilvie syndrome, urinary retention without blockage[1][2] |
| Side effects | Nausea, increased saliva, crampy abdominal pain, slow heart rate[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category | |
| Routes of use | IM, IV, subcutaneous, by mouth |
| Onset of action | Within 30 min (injection), with 4 hrs (by mouth)[1] |
| Duration of action | up to 4 hrs[1] |
| Defined daily dose | 0.4 ml (eye drop) 40 mg (eye ointment)[4] 60 milligrams (by mouth) 2 mg (by injection)[5] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data |
|
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | Unclear, probably less than 5% |
| Metabolism | Slow hydrolysis by acetylcholinesterase and also by plasma esterases |
| Elimination half-life | 50–90 minutes |
| Excretion | Unchanged drug (up to 70%) and alcoholic metabolite (30%) are excreted in the urine |
| Chemical and physical data | |
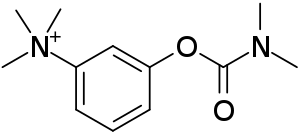
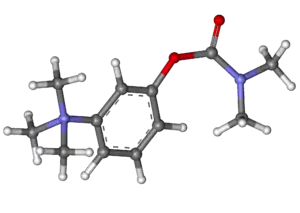
| Formula | C12H19N2O2+ |
| Molar mass | 223.296 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Neostigmine, sold under the brand name Prostigmin among others, is a medication used to treat myasthenia gravis, Ogilvie syndrome, and urinary retention without the presence of a blockage.[1][2] It is also used together with atropine to end the effects of neuromuscular blocking medication of the non-depolarizing type.[1] It is given by injection either into a vein, muscle, or under the skin.[1] After injection effects are generally greatest within 30 minutes and last up to 4 hours.[1][6]
Common side effects include nausea, increased saliva, crampy abdominal pain, and slow heart rate.[1] More severe side effects include low blood pressure, weakness, and allergic reactions.[1] It is unclear if use in pregnancy is safe for the baby.[1] Neostigmine is in the cholinergic family of medications.[1] It works by blocking the action of acetylcholinesterase and therefore increases the levels of acetylcholine.[1]
Neostigmine was patented in 1931.[7] It is on the World Health Organization's List of Essential Medicines.[8] The wholesale cost in the developing world is about US$0.18–2.6 per dose.[9] The term is from Greek neos, meaning "new", and "-stigmine", in reference to its parent molecule, physostigmine, on which it is based.[10]
Medical uses
It is used to improve muscle tone in people with myasthenia gravis, and also to reverse the effects of non-depolarizing muscle relaxants such as rocuronium and vecuronium at the end of an operation, usually in a dose of 25 to 50 μg per kilogram.
Another indication for use is the conservative management of acute colonic pseudo-obstruction, or Ogilvie's syndrome, in which patients get massive colonic dilatation in the absence of a true mechanical obstruction.[11]
Hospitals sometimes administer a solution containing neostigmine intravenously to delay the effects of envenomation through snakebite.[12] Some promising research results have also been reported for administering the drug nasally as a snakebite treatment.[13]
Neostigmine was approved in the United States in 2013 to reverse the effects of muscle relaxants.[14] It was initially approved in 1939.[15]
Dosage
0.4 ml (eye drop) or 40 mg (ointment) for lamella/eye treatment,[4] 60 milligrams (by mouth), or 2 milligrams (by injection).[5]
Side effects
Neostigmine can induce generic ocular side effects including: headache, brow pain, blurred vision, phacodonesis, pericorneal injection, congestive iritis, various allergic reactions, and rarely, retinal detachment.[16]
Neostigmine will cause slowing of the heart rate (bradycardia); for this reason it is usually given along with a parasympatholytic drug such as atropine or glycopyrrolate.
Gastrointestinal symptoms occur earliest after ingestion and include anorexia, nausea, vomiting, abdominal cramps, and diarrhea.[17]
Pharmacology
By interfering with the breakdown of acetylcholine, neostigmine indirectly stimulates both nicotinic and muscarinic receptors. Unlike physostigmine, neostigmine has a quaternary nitrogen; hence, it is more polar and does not cross the blood–brain barrier and enter the CNS, but it does cross the placenta. Its effect on skeletal muscle is greater than that of physostigmine. Neostigmine has moderate duration of action – usually two to four hours.[18] Neostigmine binds to the anionic and ester site of cholinesterase. The drug blocks the active site of acetylcholinesterase so the enzyme can no longer break down the acetylcholine molecules before they reach the postsynaptic membrane receptors. This allows for the threshold to be reached so a new impulse can be triggered in the next neuron. In myasthenia gravis there are too few acetylcholine receptors so with the acetylcholinesterase blocked, acetylcholine can bind to the few receptors and trigger a muscular contraction.
Chemistry
Neostigmine, which can be viewed as a simplified analog of physostigmine, is made by reacting 3-dimethylaminophenol with N-dimethylcarbamoyl chloride, which forms the dimethylcarbamate, and its subsequent alkylation using dimethyl sulfate forming the desired compound.
Spectral data
Neostigmine shows notable UV/VIS absorption at 261 nm, 267 nm, and 225 nm.[19]
Neostigmine's 1H NMR Spectroscopy reveals shifts at: 7.8, 7.7, 7.4, 7.4, 3.8, and 3.1 parts per million. The higher shifts are due to the aromatic hydrogens. The lower shifts at 3.8 ppm and 3.1 ppm are due to the electronic withdrawing nature of the tertiary and quaternary nitrogen, respectively.[20]
History
Neostigmine was first synthesized by Aeschlimann and Reinert in 1931[21] and was patented by Aeschlimann in 1933.[22]
Neostigmine is made by first reacting 3-dimethylaminophenol with N-dimethylcarbamoyl chloride, which forms a dimethylcarbamate. Next, that product is alkylated using dimethyl sulfate, which forms neostigmine.[23]
See also
- Miotine
- T-1123
- TL-1238
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Neostigmine Bromide". The American Society of Health-System Pharmacists. Archived from the original on 21 December 2016. Retrieved 8 December 2016.
- 1 2 World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 428. hdl:10665/44053. ISBN 9789241547659.
- 1 2 "Neostigmine Use During Pregnancy". Drugs.com. 3 January 2020. Archived from the original on 29 November 2020. Retrieved 21 January 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 4 August 2020. Retrieved 19 September 2020.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 4 August 2020. Retrieved 19 September 2020.
- ↑ "Neostigmine Methylsulfate Monograph for Professionals". Drugs.com. The American Society of Health-System Pharmacists. 19 September 2019. Archived from the original on 4 August 2020. Retrieved 20 January 2020.
- ↑ Fischer, Janos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 540. ISBN 9783527607495. Archived from the original on 20 December 2016.
- ↑ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "Neostigmine Methylsulfate". International Drug Price Indicator Guide. Archived from the original on 10 May 2017. Retrieved 8 December 2016.
- ↑ "neostigmine: definition of neostigmine in Oxford dictionary (American English) (US)". www.oxforddictionaries.com. Archived from the original on 22 December 2015. Retrieved 17 December 2015.
- ↑ Maloney N, Vargas HD (May 2005). "Acute intestinal pseudo-obstruction (Ogilvie's syndrome)". Clinics in Colon and Rectal Surgery. 18 (2): 96–101. doi:10.1055/s-2005-870890. PMC 2780141. PMID 20011348.
- ↑ Franklin, Deborah (31 July 2013). "Potential Treatment For Snakebites Leads To A Paralyzing Test". NPR. Archived from the original on 9 August 2014.
- ↑ Bulfone TC, Samuel SP, Bickler PE, Lewin MR (2018). "Developing Small Molecule Therapeutics for the Initial and Adjunctive Treatment of Snakebite". Journal of Tropical Medicine. 2018: 4320175. doi:10.1155/2018/4320175. PMC 6091453. PMID 30154870.
- ↑ "Drug Approval Package: Bloxiverz (Neostigmine Methylsulfate) Injection NDA #204078". U.S. Food and Drug Administration (FDA). 24 December 1999. Archived from the original on 5 August 2020. Retrieved 20 January 2020.
- ↑ "Bloxiverz- neostigmine methylsulfate injection". DailyMed. 19 September 2019. Archived from the original on 9 August 2020. Retrieved 21 January 2020.
- ↑ Gilman, Goodman & Gilman 1980, p. 114.
- ↑ Gilman, Goodman & Gilman 1980, p. 109.
- ↑ Howland RD, Mycek MJ, Harvey RA, Champe PC, Mycek MJ (2008). Pharmacology (3rd ed.). Lippincott's Illustrated Reviews. p. 51.
- ↑ Porst H, Kny L (May 1985). "[The structure of degradation products of neostigmine bromide]". Die Pharmazie (in German). 40 (5): 325–8. PMID 4034636.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Ferdous AJ, Waigh RD (June 1993). "Application of the WATR technique for water suppression in 1H NMR spectroscopy in determination of the kinetics of hydrolysis of neostigmine bromide in aqueous solution". The Journal of Pharmacy and Pharmacology. 45 (6): 559–62. doi:10.1111/j.2042-7158.1993.tb05598.x. PMID 8103105.
- ↑ Whitacre 2007, p. 57.
- ↑ Aeschliman, John A., U.S. Patent 1,905,990 (1933).
- ↑ Gilman, Goodman & Gilman 1980, p. 103.
Further reading
- Gilman, A.G.; Goodman, L.S.; Gilman, A. (1980). Goodman & Gilman's The Pharmacological Basis of Therapeutics (6th ed.). New York: Macmillan Publishing Co., Inc.
- Whitacre, David M. (2007). Reviews of Environmental Contamination and Toxicology. Springer Science+Business Media. p. 57. ISBN 978-0-387-73162-9. Archived from the original on 6 August 2020. Retrieved 23 October 2016.
External links
| Identifiers: |
|---|
- "Neostigmine". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 28 June 2019. Retrieved 6 January 2020.