Insulin degludec
 | |
| Names | |
|---|---|
IUPAC name
| |
| Clinical data | |
| Drug class | Insulin (long-acting)[1] |
| Main uses | Type I and type II diabetes[1] |
| Side effects | Low blood sugar, allergic reactions, pain at the site of injection, itchiness, rash, weight gain, lipodystrophy[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Subcutaneous |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data | |
| Legal status | |
| Chemical and physical data | |
| Formula | C274H411N65O81S6 |
| Molar mass | 6104.04 g·mol−1 |
Insulin degludec, under the brand name Tresiba is an long-acting insulin used to treat type I and type II diabetes.[1] It once daily by injection under the skin.[1] Onset of effects occur within 90 minutes and last for more than 42 hours.[1] After a few days it has a steady effects at all hours.[3]
Common side effects include low blood sugar, allergic reactions, pain at the site of injection, itchiness, rash, weight gain, and lipodystrophy.[1] It has a lower risk of low blood sugar compared to long acting detemir and glargine.[4] Other side effects may include low potassium.[1] In pregnancy NPH insulin is preferred.[5] It is a form of insulin made by recombinant DNA technology and than further modified.[5][1]
Insulin degludec was approved for medical use in Europe in 2013 and the United States in 2015.[6][1] It is on the World Health Organization's List of Essential Medicines.[7] In the United Kingdom a 300 unit pen costs the NHS about £9 as of 2021.[5] In the United States this amount costs about 100 USD.[8] In 2019, it was the 168th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[9][10] It is also available in combination with liraglutide.[1]
Medical uses
It is used for type I and type II diabetes.[1] In type I diabetes it is used together with a rapid acting insulin.[6]
Dosage
The dose is adjusted based on blood sugar control.[5]
People taking insulin degludec needed to take smaller doses of basal insulin than those taking insulin glargine U100, while achieving similar blood glucose levels. Insulin degludec also has the ability to be mixed with other insulins, thereby improving glycemic control. This cannot be done with some other long-acting insulins.[11][12]
Side effects
A side effect of insulin therapy is low blood sugar. A 2012 review found 39 to 47.9 events of hypoglycemia (defined as blood glucose <56 mg/dL) per patient year, with higher rates in the more concentrated degludec formulation. Rates of nighttime hypoglycemia ranged from 3.7 to 5.1 events per patient year.[13]
Pharmacology
Mechanism of action
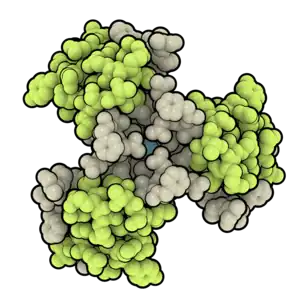
Insulin degludec is an ultra-long acting insulin that, unlike insulin glargine, is active at a physiologic pH. The addition of hexadecanedioic acid via an amide linkage to lysine at the B29 position allows for the formation of multi-hexamers in subcutaneous tissues.[14] This allows for the formation of a subcutaneous depot that results in slow insulin release into the systemic circulation.[15]
Pharmacokinetics
Insulin degludec has an onset of action of 30–90 minutes (similar to insulin glargine and insulin detemir). There is no peak in activity, due to the slow release into systemic circulation. The duration of action of insulin degludec is longer than 24 hours.[14][13]
When taken at the same time of day, this long (but under 48 hour) duration can result in an overlap from one dose to the next, resulting in greater insulin action then. if the overlap should be during sleep, there is a risk of lower blood sugar, so it is important to dose in the morning so that the overlap will be when users are eating and otherwise checking their blood sugar. The dose should be titrated during this overlap period as well.
Chemistry
It is a modified insulin that has one single amino acid deleted in comparison to human insulin, and is conjugated to hexadecanedioic acid via gamma-L-glutamyl spacer at the amino acid lysine at position B29.
History
Insulin degludec has been filed for registration in the United States.[16] Novo Nordisk hopes to begin marketing the insulin analog in 2015 or 2016 after the completion of additional cardiac safety studies requested by the U.S. Food and Drug Administration (FDA) in February 2013.[17] Insulin degludec received FDA approval 25 September 2015[18] and marketing began on 26 January 2016.[19]
Society and culture
Cost
The cost of this medication in the U.S. is $363 (USD) for 10 ml subcutaneous solution 100 units/mL [20]
.svg.png.webp) InsulinDegludec costs (US)
InsulinDegludec costs (US).svg.png.webp) InsulinDegludec prescriptions (US)
InsulinDegludec prescriptions (US)
Given the treat-to-target nature of the BEGIN trial program, much of the health economic analysis of insulin degludec has focussed on short-term cost-effectiveness based on differences in insulin dosing and hypoglycemic event incidence rather than differences in glycemic control.[21] The first cost-effectiveness analysis of this nature was conducted from a societal perspective in the Swedish setting in 2013, finding that insulin degludec would be cost-effective relative to insulin glargine in the treatment of type 1 diabetes, and type 2 diabetes as part of either a basal or basal-insulin regimen.[21]
Research
Type 1 diabetes
Insulin degludec was studied as an alternative to insulin glargine as part of a basal-bolus regimen in the BEGIN Basal-Bolus Type 1 trial. 629 patients with type 1 diabetes were randomized in a 3:1 ratio to either insulin degludec (n=472) or insulin glargine (n=157) in addition to mealtime insulin aspart. Patients in the degludec treatment arm were switched from their basal insulin to insulin degludec in a 1:1 ratio, with a 20-30% dose reduction in patients receiving multiple basal doses per day. After 52 weeks, patients treated with insulin degludec produced a similar reduction in HbA1c (0.40% vs. 0.39%) meeting the criteria for noninferiority. Adverse events were similar in the two treatment arms; however, rates of nocturnal hypoglycemia (between midnight and 6am) were 27% lower in patients treated with insulin degludec (3.91 vs. 5.22%,p=0.024). The reduction in the incidence of hypoglycemia was seen as a therapeutic benefit, as hypoglycemia is often a dose limiting toxicity in insulin therapy.[22]
Type 2 diabetes
In the BEGIN Basal-Bolus Type 2 trial, insulin degludec was studied as an alternative to insulin glargine in patients with type 2 diabetes mellitus. 995 patients were randomized to receive either insulin degludec (n=755) or insulin glargine (n=251), in addition to either mealtime insulin aspart, metformin, and/or pioglitazone. Patients in this trial had an average HbA1c of 8.3–8.4%, and 49–50% were on a regimen consisting of basal-bolus insulin plus oral antidiabetic medications. After 52 weeks, insulin degludec was found to be noninferior to insulin glargine, providing a similar HbA1c lowering effect (−1.10 vs. −1.18%). Overall rates of hypoglycemia were significantly lower with insulin degludec (11.09 vs. 13.63%/yr, p=0.0359), including cases of nocturnal hypoglycemia (1.39 vs. 1.84%/yr, p=0.0399).[23]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Insulin Degludec Monograph for Professionals". Drugs.com. Archived from the original on 21 October 2020. Retrieved 26 November 2021.
- ↑ "Tresiba EPAR". European Medicines Agency (EMA). Archived from the original on 22 January 2021. Retrieved 15 January 2021.
- ↑ "Tresiba Summary of product characteristics" (PDF). European Medicines Agency. Archived (PDF) from the original on 2016-03-04. Retrieved 2021-01-16.
- ↑ Ton, Joey (21 March 2022). "#311 "Ultralong"-acting insulin for diabetes: How long is long enough?". CFPCLearn. Archived from the original on 1 February 2023. Retrieved 14 June 2023.
- 1 2 3 4 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 757. ISBN 978-0857114105.
- 1 2 "Tresiba". Archived from the original on 22 January 2021. Retrieved 26 November 2021.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ↑ "Tresiba Prices, Coupons & Savings Tips - GoodRx". GoodRx. Archived from the original on 8 October 2021. Retrieved 26 November 2021.
- ↑ "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- ↑ "Insulin Degludec - Drug Usage Statistics". ClinCalc. Archived from the original on 12 April 2020. Retrieved 11 April 2020.
- ↑ "Monograph - Insulin Glargine: Dosage & Administration". American Society of Health-System Pharmacists, Inc. Archived from the original on 2021-08-28. Retrieved 2010-11-07.
- ↑ Ringstrom A (2010-06-26). "Novo says degludec has potential to lower blood sugar". Reuters. Archived from the original on 2010-07-12. Retrieved 2010-11-07.
- 1 2 Wang F, Surh J, Kaur M (2012). "Insulin degludec as an ultralong-acting basal insulin once a day: a systematic review". Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 5: 191–204. doi:10.2147/DMSO.S21979. PMC 3402007. PMID 22826637.
- 1 2 Nasrallah SN, Reynolds LR (2012). "Insulin Degludec, The New Generation Basal Insulin or Just another Basal Insulin?". Clinical Medicine Insights. Endocrinology and Diabetes. 5: 31–7. doi:10.4137/CMED.S9494. PMC 3411522. PMID 22879797.
- ↑ Robinson JD, Neumiller JJ, Campbell RK (December 2012). "Can a new ultra-long-acting insulin analogue improve patient care? Investigating the potential role of insulin degludec". Drugs. 72 (18): 2319–25. doi:10.2165/11642240-000000000-00000. PMID 23145524. S2CID 21557012.
- ↑ "R&D Pipeline". Novo Nordisk. Archived from the original on 2014-12-25. Retrieved 2012-01-27.
- ↑ Hirschler B (2010-10-27). "New Novo insulin fails to knock out rival Sanofi". Reuters. Archived from the original on 2021-08-28. Retrieved 2010-11-07.
- ↑ "FDA approves two new drug treatments for diabetes mellitus". U.S. Food and Drug Administration. Archived from the original on 16 January 2016.
- ↑ "Novo Nordisk Launches Tresiba® (insulin degludec injection 200 Units/mL) in the United States". novonordisk-us.com. Archived from the original on 2018-05-22. Retrieved 2021-01-16.
- ↑ "Tresiba Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 7 December 2020. Retrieved 1 April 2021.
- 1 2 Ericsson, Å.; Pollock, R. F.; Hunt, B.; Valentine, W. J. (2013). "Evaluation of the cost-utility of insulin degludec vs insulin glargine in Sweden". Journal of Medical Economics. 16 (12): 1442–1452. doi:10.3111/13696998.2013.852099. ISSN 1369-6998. PMID 24147661. S2CID 826947.
- ↑ Heller S, Buse J, Fisher M, Garg S, Marre M, Merker L, et al. (April 2012). "Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN Basal-Bolus Type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial". Lancet. 379 (9825): 1489–97. doi:10.1016/S0140-6736(12)60204-9. PMID 22521071. S2CID 5868807.
- ↑ Garber AJ, King AB, Del Prato S, Sreenan S, Balci MK, Muñoz-Torres M, et al. (April 2012). "Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN Basal-Bolus Type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial". Lancet. 379 (9825): 1498–507. doi:10.1016/S0140-6736(12)60205-0. PMID 22521072. S2CID 205965206.
External links
| Identifiers: |
|---|
- "Insulin degludec". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2021-08-28. Retrieved 2021-01-16.