Pramlintide
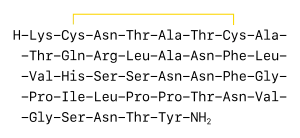 Golden line indicates disulfide bond | |
| Names | |
|---|---|
| Trade names | Symlin |
| Clinical data | |
| Drug class | Amylin analogue[1] |
| Main uses | Type 1 and 2 diabetes with mealtime insulin[1] |
| Side effects | Nausea, loss of appetite, headache, low blood sugar[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | Subcutaneous |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605031 |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | 30 to 40% |
| Protein binding | ~60% |
| Metabolism | Kidney |
| Elimination half-life | ~48 minutes |
| Chemical and physical data | |
| Formula | C171H267N51O53S2 |
| Molar mass | 3949.44 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Pramlintide, sold under the brand name Symlin, is a medication used to treat type 1 and 2 diabetes in people who use insulin at mealtime.[1] It is given by injection under the skin.[1]
Common side effects include nausea, loss of appetite, and headache.[1] Other side effects may include low blood sugar and allergic reactions.[1][2] Use is not recommended in people with gastroparesis.[1] Safety in pregnancy is unclear.[3] It is a amylin analogue.[1]
Pramlintide was approved for medical use in the United States in 2005.[1] In the United States 50 doses of 60 mcg costs about 1,000 USD as of 2021.[4]
Medical uses
Dosage
In type 1 DM it is started at a dose of 15 mcg before eating and may be increased up to 60 mcg.[1]
In type 2 DM it is started at 60 mcg and may be increased to 120 mcg.[1]
Pharmacology
Pramlintide is an analogue of amylin, a small peptide hormone that is released into the bloodstream by the β cells of the pancreas along with insulin after a meal.[5] Like insulin, amylin is completely absent in individuals with Type I diabetes.[6]
In synergy with endogenous amylin, pramlintide aids in the regulation of blood glucose by slowing gastric emptying, promoting satiety via hypothalamic receptors (different receptors than for GLP-1), and inhibiting inappropriate secretion of glucagon, a catabolic hormone that opposes the effects of insulin and amylin. Pramlintide also has effects in raising the acute first-phase insulin response threshold following a meal.
Both a reduction in glycated hemoglobin and weight loss have been shown in insulin-treated patients with type 2 diabetes taking pramlintide as an adjunctive therapy.[7]
Chemistry
Since native human amylin is highly amyloidogenic and potentially toxic, the strategy for designing pramlintide was to substitute residues from rat amylin, which is less amyloidogenic although not completely [8][9] (but would presumably retain clinical activity). Proline residues are known to be structure-breaking residues, so these were directly grafted into the human sequence. Despite its enhanced stability compared to human amylin, pramlintide is still able to organize into amyloid material.[10]
Amino acid sequences:
| Pramlintide | KCNTATCATQRLANFLVHSSNNFGPILPPTNVGSNTY-(NH2) |
| Amylin | KCNTATCATQRLANFLVHSSNNFGAILSSTNVGSNTY-(NH2) |
| Rat amylin | KCNTATCATQRLANFLVRSSNNLGPVLPPTNVGSNTY-(NH2) |
Pramlintide as protein is (positively charged).
History
Pramlintide has been approved by the FDA, for use by type 1 and type 2 diabetics who use insulin.[11] Pramlintide allows patients to use less insulin, lowers average blood sugar levels, and substantially reduces what otherwise would be a large unhealthy rise in blood sugar that occurs in diabetics right after eating.
Apart from insulin analogs, pramlintide is the only drug approved by the FDA to lower blood sugar in type 1 diabetics since insulin in the early 1920s.[12]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "DailyMed - SYMLINPEN- pramlintide acetate injection". dailymed.nlm.nih.gov. Archived from the original on 19 March 2021. Retrieved 29 October 2021.
- ↑ "Pramlintide Monograph for Professionals". Drugs.com. Archived from the original on 4 March 2021. Retrieved 29 October 2021.
- ↑ "Pramlintide Use During Pregnancy". Drugs.com. Archived from the original on 25 January 2021. Retrieved 29 October 2021.
- ↑ "SymlinPen 60 Prices, Coupons & Patient Assistance Programs". Drugs.com. Archived from the original on 22 January 2021. Retrieved 29 October 2021.
- ↑ Jones MC (2007). "Therapies for diabetes: pramlintide and exenatide" (PDF). American Family Physician. 75 (12): 1831–5. PMID 17619527. Archived (PDF) from the original on 2017-08-09. Retrieved 2021-05-05.
- ↑ Edelman, Steve; Maier, Holly; Wilhelm, Ken (2008). "Pramlintide in the Treatment of Diabetes Mellitus". BioDrugs. 22 (6): 375–386. doi:10.2165/0063030-200822060-00004. ISSN 1173-8804. PMID 18998755.
- ↑ Hollander, Priscilla; Maggs, David G.; Ruggles, James A.; Fineman, Mark; Shen, Larry; Kolterman, Orville G.; Weyer, Christian (2004). "Effect of Pramlintide on Weight in Overweight and Obese Insulin-Treated Type 2 Diabetes Patients" (PDF). Obesity. 12 (4): 661–668. doi:10.1038/oby.2004.76. ISSN 1930-7381. PMID 15090634.
- ↑ Palmieri, Leonardo C; Melo-Ferreira, Bruno; Braga, Carolina A; Fontes, Giselle N; Mattos, Luana J; Lima, Luis Mauricio (2013). "Stepwise oligomerization of murine amylin and assembly of amyloid fibrils". Biophys Chem. 181: 135–144. doi:10.1016/j.bpc.2013.07.013. PMID 23974296.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Erthal, Luiza C; Marques, Adriana F; Almeida, Fábio C; Melo, Gustavo L; Carvalho, Camila M; Palmieri, Leonardo C; Cabral, Kátia M; Fontes, Giselle N; Lima, Luis Mauricio (2016). "Regulation of the assembly and amyloid aggregation of murine amylin by zinc". Biophys. Chem. 218: 58–70. doi:10.1016/j.bpc.2016.09.008. PMID 27693831.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ da Silva, Dayana C; Fontes, Giselle N; Erthal, Luiza C; Lima, Luis Mauricio. (2016). "Amyloidogenesis of the amylin analogue pramlintide". Biophys. Chem. 219: 1–8. doi:10.1016/j.bpc.2016.09.007. PMID 27665170.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Ryan GJ, Jobe LJ, Martin R (2005). "Pramlintide in the treatment of type 1 and type 2 diabetes mellitus". Clinical Therapeutics. 27 (10): 1500–12. doi:10.1016/j.clinthera.2005.10.009. PMID 16330288.
- ↑ "Dual-Hormone, Artificial Pancreas with Insulin and Pramlintide Significantly Improves Glucose Levels, Compared to Insulin-Only Artificial Pancreas". American Diabetes Association. Archived from the original on 2018-08-29. Retrieved 2018-08-28.
External links
| Identifiers: |
|---|
Template:Neuropeptidergics