Galloway Mowat syndrome
| Galloway Mowat syndrome | |
|---|---|
| Other names: Galloway Syndrome, Hiatal Hernia-Microcephaly-Nephrosis, Galloway Type, Microcephaly-Hiatal Hernia-Nephrosis, Galloway Type, Nephrosis-Microcephaly Syndrome, Nephrosis-Neuronal Dysmigration Syndrome, Microcephaly-Hiatal Hernia-Nephrotic Syndrome | |
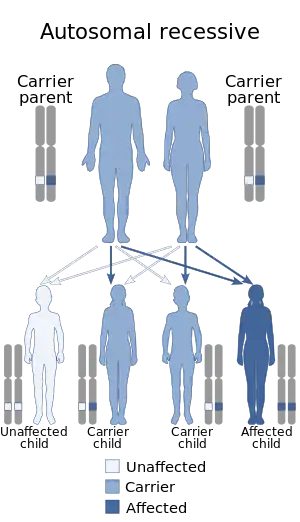 | |
| Galloway Mowat syndrome has an autosomal recessive pattern of inheritance. | |
Galloway Mowat syndrome is a very rare autosomal recessive[1] genetic disorder, consisting of a variety of features including hiatal hernia, microcephaly and nephrotic syndrome.[2]
Signs and symptoms

The clinical presentation of this condition is as follows:[3]
- Underdeveloped ear cartilage
- Cognitive impairment
- Nephropathy
- Proteinuria
- Intellectual impairment
- Ataxia
Cause
The exact genetic defect in Galloway Mowat syndrome is yet to be discovered. However, mutations in podocyte proteins, such as nephrin, alpha-actinin 4, and podocin, are associated with proteinuria and nephrotic syndrome. There is reduced expression of synaptopodin, GLEPP1, and nephrin in Galloway-Mowat syndrome, but these are likely secondary to the proteinuria, likely not the proteins mutated in Galloway-Mowat syndrome.[4]
The biochemical lesion appears to be in the Kinase, Endopeptidase and Other Proteins of small Size (KEOPS)/Endopeptidase-like and Kinase associated to transcribed Chromatin (EKC) (KEOPS/EKC) complex.[5] Sequencing of genes in 37 cases of this condition revealed mutations in the OSGEP, TP53RK, TPRKB and LAGE3 genes all of which encode subunits in the KEOPS complex. Members of this complex are found in bacteria, archaea and eukaryotes and are highly conserved. The function of this complex is still under investigation.
The biochemical lesion in this condition appears to be in the N6-threonyl-carbamoylation of adenosine 37 of ANN-type tRNA pathway. This pathway uses two sequentially acting enzymes - YRDC and OSGEP. Mutations in these genes leads to this syndrome.[6]
Genetics
Galloway Mowat syndrome is usually an autosomal recessive disorder,[1] which means the defective gene responsible for the disorder is located on an autosome, and two copies of the defective gene (one inherited from each parent) are required in order to be born with the disorder. The parents of an individual with an autosomal recessive disorder both carry one copy of the defective gene, but usually do not experience any signs or symptoms of the disorder. Multiple genes (10 genes as of October 2020) are causal for the clinical symptoms of Galloway Mowat syndrome. There is one gene, LAGE3, associated with X-linked inheritance of Galloway Mowat syndrome.
Diagnosis
The diagnosis of Galloway Mowat syndrome is done via the following manner in those individuals suspected of having the condition:[7]
- Clinical evaluation
- Characteristic physical findings
- Laboratory tests
- Imaging techniques
- Genetic testing
Treatment
The management of this condition entails addressing the specific symptom(s) each individual displays , as well as:[7]
- Special education
- Physical therapy
- Speech therapy
- Social or vocational services
References
- 1 2 Cooperstone BG, Friedman A, Kaplan BS (Aug 1993). "Galloway-Mowat syndrome of abnormal gyral patterns and glomerulopathy" (Free full text). American Journal of Medical Genetics. 47 (2): 250–254. doi:10.1002/ajmg.1320470221. PMID 8213914. Archived from the original on 2020-09-12. Retrieved 2021-11-21.
- ↑ Galloway WH, Mowat AP (Dec 1968). "Congenital microcephaly with hiatus hernia and nephrotic syndrome in two sibs". Journal of Medical Genetics. 5 (4): 319–321. doi:10.1136/jmg.5.4.319. ISSN 0022-2593. PMC 1468664. PMID 5713646.
- ↑ "Galloway-Mowat syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 22 April 2021. Retrieved 13 December 2021.
- ↑ Srivastava T, Whiting JM, Garola RE, Dasouki MJ, Ruotsalainen V, Tryggvason K, Hamed R, Alon US (Dec 2001). "Podocyte proteins in Galloway-Mowat syndrome". Pediatric Nephrology (Berlin, Germany). 16 (12): 1022–1029. doi:10.1007/s004670100018. PMID 11793093. S2CID 23690258.
- ↑ Braun DA, Rao J, Mollet G, Schapiro D, Daugeron MC, Tan W, Gribouval O, Boyer O, Revy P, Jobst-Schwan T, Schmidt JM, Lawson JA, Schanze D, Ashraf S, Ullmann JFP, Hoogstraten CA, Boddaert N, Collinet B, Martin G, Liger D, Lovric S, Furlano M, Guerrera IC, Sanchez-Ferras O, Hu JF, Boschat AC, Sanquer S, Menten B, Vergult S, De Rocker N, Airik M, Hermle T, Shril S, Widmeier E, Gee HY, Choi WI, Sadowski CE, Pabst WL, Warejko JK, Daga A, Basta T, Matejas V, Scharmann K, Kienast SD, Behnam B, Beeson B, Begtrup A, Bruce M, Ch'ng GS, Lin SP, Chang JH, Chen CH, Cho MT, Gaffney PM, Gipson PE, Hsu CH, Kari JA, Ke YY, Kiraly-Borri C, Lai WM, Lemyre E, Littlejohn RO, Masri A, Moghtaderi M, Nakamura K, Ozaltin F, Praet M, Prasad C, Prytula A, Roeder ER, Rump P, Schnur RE, Shiihara T, Sinha MD, Soliman NA, Soulami K, Sweetser DA, Tsai WH, Tsai JD, Topaloglu R, Vester U, Viskochil DH, Vatanavicharn N, Waxler JL, Wierenga K, Wolf MTF, Wong SN, Leidel SA, Truglio G, Dedon PC, Poduri A, Mane S, Lifton RP, Bouchard M, Kannu P, Chitayat D, Magen D, Callewaert B, van Tilbeurgh H, Zenker M, Antignac C, Hildebrandt F (2017) Mutations in KEOPS-complex genes cause nephrotic syndrome with primary microcephaly. Nat Genet
- ↑ Arrondel C, Missoury S, Snoek R, Patat J, Menara G, Collinet B, Liger D, Durand D, Gribouval O, Boyer O, Buscara L, Martin G, Machuca E, Nevo F, Lescop E, Braun DA, Boschat AC, Sanquer S, Guerrera IC, Revy P, Parisot M, Masson C, Boddaert N, Charbit M, Decramer S, Novo R, Macher MA, Ranchin B, Bacchetta J, Laurent A, Collardeau-Frachon S, van Eerde AM, Hildebrandt F, Magen D, Antignac C, van Tilbeurgh H, Mollet G (2019) Defects in t6A tRNA modification due to GON7 and YRDC mutations lead to Galloway-Mowat syndrome. Nat Commun 10(1):3967
- 1 2 "Galloway-Mowat Syndrome". NORD (National Organization for Rare Disorders). Archived from the original on 11 March 2021. Retrieved 13 December 2021.
External links
| Classification | |
|---|---|
| External resources |
|
- Microcephaly, hiatal hernia and nephrotic syndrome at NIH's Office of Rare Diseases