Haematopoietic system
| Haematopoietic system | |
|---|---|
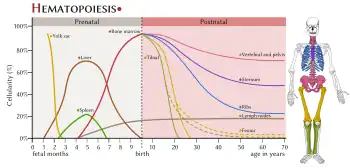 Sites of haematopoiesis periods before and after birth. | |
| Details | |
| Function | Creation of the cells of blood. |
| Identifiers | |
| MeSH | D006413 |
| FMA | 9667 |
| Anatomical terminology | |
The haematopoietic system is the system in the body involved in the creation of the cells of blood.[1]
Structure
Stem cells
Haematopoietic stem cells (HSCs) reside in the medulla of the bone (bone marrow) and have the unique ability to give rise to all of the different mature blood cell types and tissues.[2] HSCs are self-renewing cells: when they differentiate, at least some of their daughter cells remain as HSCs, so the pool of stem cells is not depleted. This phenomenon is called asymmetric division.[3] The other daughters of HSCs (myeloid and lymphoid progenitor cells) can follow any of the other differentiation pathways that lead to the production of one or more specific types of blood cell, but cannot renew themselves. The pool of progenitors is heterogeneous and can be divided into two groups; long-term self-renewing HSC and only transiently self-renewing HSC, also called short-terms.[4] This is one of the main vital processes in the body.
Development
In developing embryos, blood formation occurs in aggregates of blood cells in the yolk sac, called blood islands. As development progresses, blood formation occurs in the spleen, liver and lymph nodes. When bone marrow develops, it eventually assumes the task of forming most of the blood cells for the entire organism.[2] However, maturation, activation, and some proliferation of lymphoid cells occurs in the spleen, thymus, and lymph nodes. In children, haematopoiesis occurs in the marrow of the long bones such as the femur and tibia. In adults, it occurs mainly in the pelvis, cranium, vertebrae, and sternum.[5]
Function
Haematopoiesis (from Greek αἷμα, "blood" and ποιεῖν "to make"; also hematopoiesis in American English; sometimes also haemopoiesis or hemopoiesis) is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells.[2] In a healthy adult person, approximately 1011–1012 new blood cells are produced daily in order to maintain steady state levels in the peripheral circulation.[6][7]
All blood cells are divided into three lineages.[8]
- Red blood cells, also called erythrocytes, are the oxygen-carrying cells. Erythrocytes are functional and are released into the blood. The number of reticulocytes, immature red blood cells, gives an estimate of the rate of erythropoiesis.
- Lymphocytes are the cornerstone of the adaptive immune system. They are derived from common lymphoid progenitors. The lymphoid lineage is composed of T-cells, B-cells and natural killer cells. This is lymphopoiesis.
- Cells of the myeloid lineage, which include granulocytes, megakaryocytes and macrophages, are derived from common myeloid progenitors, and are involved in such diverse roles as innate immunity and blood clotting. This is myelopoiesis.
Clinical significance
Stem cell transplant
A stem cell transplant is a transplant intended to replace the progenitor hematopoietic stem cells
Hematopoietic stem cell transplantation (HSCT) is the transplantation of multipotent hematopoietic stem cells, usually derived from bone marrow, peripheral blood, or umbilical cord blood.[9][10][11] It may be autologous (the patient's own stem cells are used), allogeneic (the stem cells come from a donor) or syngeneic (from an identical twin).[9][10]
It is most often performed for patients with certain cancers of the blood or bone marrow, such as multiple myeloma or leukemia.[10] In these cases, the recipient's immune system is usually destroyed with radiation or chemotherapy before the transplantation. Infection and graft-versus-host disease are major complications of allogeneic HSCT.[10]
Hematopoietic stem cell transplantation remains a dangerous procedure with many possible complications; it is reserved for patients with life-threatening diseases. As survival following the procedure has increased, its use has expanded beyond cancer to autoimmune diseases[12][13] and hereditary skeletal dysplasias; notably malignant infantile osteopetrosis[14][15] and mucopolysaccharidosis.[16]
References
- ↑ "hematopoietic system". Merriam-Webster. Retrieved 8 July 2019.
- 1 2 3 Birbrair, Alexander; Frenette, Paul S. (2016-03-01). "Niche heterogeneity in the bone marrow". Annals of the New York Academy of Sciences. 1370 (1): 82–96. Bibcode:2016NYASA1370...82B. doi:10.1111/nyas.13016. ISSN 1749-6632. PMC 4938003. PMID 27015419.
- ↑ Morrison, J.; Judith Kimble (2006). "Asymmetric and symmetric stem-cell divisions in development and cancer" (PDF). Nature. 441 (7097): 1068–74. Bibcode:2006Natur.441.1068M. doi:10.1038/nature04956. hdl:2027.42/62868. PMID 16810241. S2CID 715049.
- ↑ Morrison, SJ; Weissman, IL (Nov 1994). "The long-term repopulating subset of hematopoietic stem cells is deterministic and isolable by phenotype". Immunity. 1 (8): 661–73. doi:10.1016/1074-7613(94)90037-x. PMID 7541305.
- ↑ Fernández, KS; de Alarcón, PA (Dec 2013). "Development of the hematopoietic system and disorders of hematopoiesis that present during infancy and early childhood". Pediatric Clinics of North America. 60 (6): 1273–89. doi:10.1016/j.pcl.2013.08.002. PMID 24237971.
- ↑ Semester 4 medical lectures at Uppsala University 2008 by Leif Jansson
- ↑ Parslow, T G.; Stites, DP.; Terr, AI.; Imboden JB. (1997). Medical Immunology (1 ed.). ISBN 978-0-8385-6278-9.
- ↑ "Hematopoiesis from Pluripotent Stem Cells". ThermoFisher Scientific. Retrieved 3 February 2014.
- 1 2 Felfly, H; Haddad, GG (2014). "Hematopoietic stem cells: potential new applications for translational medicine". Journal of Stem Cells. 9 (3): 163–97. PMID 25157450.
- 1 2 3 4 Park, B; Yoo, KH; Kim, C (December 2015). "Hematopoietic stem cell expansion and generation: the ways to make a breakthrough". Blood Research. 50 (4): 194–203. doi:10.5045/br.2015.50.4.194. PMC 4705045. PMID 26770947.
- ↑ Mahla RS (2016). "Stem cells application in regenerative medicine and disease threpeutics". International Journal of Cell Biology. 2016 (7): 1–24. doi:10.1155/2016/6940283. PMC 4969512. PMID 27516776.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Tyndall A, Fassas A, Passweg J, et al. (1999). "Autologous haematopoietic stem cell transplants for autoimmune disease–feasibility and transplant-related mortality. Autoimmune Disease and Lymphoma Working Parties of the European Group for Blood and Marrow Transplantation, the European League Against Rheumatism and the International Stem Cell Project for Autoimmune Disease". Bone Marrow Transplant. 24 (7): 729–34. doi:10.1038/sj.bmt.1701987. PMID 10516675.
- ↑ Burt RK, Loh Y, Pearce W, et al. (2008). "Clinical applications of blood-derived and marrow-derived stem cells for nonmalignant diseases". JAMA. 299 (8): 925–36. doi:10.1001/jama.299.8.925. PMID 18314435.
- ↑ EL-Sobky TA, El-Haddad A, Elsobky E, Elsayed SM, Sakr HM (March 2017). "Reversal of skeletal radiographic pathology in a case of malignant infantile osteopetrosis following hematopoietic stem cell transplantation". The Egyptian Journal of Radiology and Nuclear Medicine. 48 (1): 237–43. doi:10.1016/j.ejrnm.2016.12.013.
- ↑ Hashemi Taheri AP, Radmard AR, Kooraki S, Behfar M, Pak N, Hamidieh AA, Ghavamzadeh A (September 2015). "Radiologic resolution of malignant infantile osteopetrosis skeletal changes following hematopoietic stem cell transplantation". Pediatric Blood & Cancer. 62 (9): 1645–49. doi:10.1002/pbc.25524. PMID 25820806. S2CID 11287381.
- ↑ Langereis EJ, den Os MM, Breen C, Jones SA, Knaven OC, Mercer J, Miller WP, Kelly PM, Kennedy J, Ketterl TG, O'Meara A, Orchard PJ, Lund TC, van Rijn RR, Sakkers RJ, White KK, Wijburg FA (March 2016). "Progression of Hip Dysplasia in Mucopolysaccharidosis Type I Hurler After Successful Hematopoietic Stem Cell Transplantation". The Journal of Bone and Joint Surgery. 98 (5): 386–95. doi:10.2106/JBJS.O.00601. PMID 26935461.