Hantavirus infection
| Hantavirus infection | |
|---|---|
| Other names: Hantavirus, hantavirus disease, hantavirus syndrome | |
 | |
| The cotton rat, Sigmodon hispidus, is a hantavirus carrier that becomes a threat when it enters human habitation in rural and suburban areas. | |
| Specialty | Infectious disease |
| Symptoms | HFRS: Headache, abdominal pain, fever, nausea, bleeding, kidney failure[1] HPS: Tiredness, fever, muscle pain, cough, shortness of breath[2] |
| Usual onset | 1 to 8 weeks following exposure[1][2] |
| Types | Hemorrhagic fever with renal syndrome (HFRS) Hantavirus pulmonary syndrome (HPS)[3] |
| Causes | Orthohantavirus spread by rodents[4] |
| Diagnostic method | Blood tests[4] |
| Prevention | Rodent control[4] |
| Treatment | Supportive care[4] |
| Frequency | HFRS 100,000 cases per year, HPS < 50 cases per year[4] |
| Deaths | HFRS 12%, HPS 40%[4] |
Hantavirus infection can result in a number of forms of disease including hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS).[3] Symptoms of HFRS generally include headache, abdominal pain, fever, nausea, bleeding, and kidney failure.[1] Symptoms of HPS include tiredness, fever, muscle pain, cough, and shortness of breath.[2] Onset of initial symptoms is generally 1 to 8 weeks following exposure.[1][2]
HFPS is due to Old World hantaviruses while HPS is due to New World hantaviruses.[3] More than 28 specific hantaviruses cause disease in humans.[4] The disease is typically spread when people breath in air contaminated by rodent droppings.[4] The underlying mechanism of both forms of the disease involves low platelets and leaky blood vessels.[4] Diagnosis is based on blood tests, typically serology.[4]
Treatment is primarily supportive care.[4] This may include oxygen therapy, mechanical ventilation, dialysis, or platelet transfusions.[4] Ribavirin may be useful if given early in HFRS.[4] The risk of death is around 12% with HFRS and around 40% with HPS.[4]
About 100,000 cases of HFRS occur a year, while about 1,000 cases of HPS have been identified since it was first detected in 1993.[4] Descriptions of what is believed to be hantavirus infections date back to around 1000 AD.[4] The virus that causes the disease; however, was only discovered in 1976 in the Hantan River area of South Korea.[4][5]
Signs and symptoms
Hemorrhagic fever with renal syndrome
Hemorrhagic fever with renal syndrome (HFRS) is caused chiefly by hantaviruses in Asia and Europe. Clinical presentation varies from subclinical to fatal, depending on the virus. After an incubation period of 2–4 weeks, the typical illness starts with non-specific symptoms such as high fever, chills, headache, backache, abdominal pains, nausea, and vomiting. After the initial period, bleeding under the skin begins, often paired with low blood pressure, followed by further internal bleeding throughout the body. Renal dysfunction leading to further health issues begins thereafter, which may cause death.[4] A more mild form of HFRS that occurs in Europe is called "nephropathia epidemica" (NE).[6] Trench nephritis during World War I is now thought to have been Hemorrhagic fever with renal syndrome.
Hantavirus pulmonary syndrome
Hantavirus pulmonary syndrome (HPS), also called hantavirus cardiopulmonary syndrome (HCPS), is usually caused by hantaviruses in the Americas. Its incubation period ranges from 16 to 24 days. Illness initially shows similar symptoms as HFRS. After a few days of non-specific symptoms, sudden onset of progressive, or productive, coughing, shortness of breath, and elevated heart rate occur due to fluid buildup in the lungs. These symptoms are accompanied by impairment of lymphoid organs. Death from cardiovascular shock may occur rapidly after the appearance of severe symptoms.[4][7] While HCPS is typically associated with New World hantaviruses, the Puumala orthohantavirus in Europe has also caused the syndrome on rare occasions.[6]
Cause
.jpg.webp)
The cause is Orthohantavirus, a genus of single-stranded, enveloped, negative-sense RNA viruses in the family Hantaviridae of the order Bunyavirales.[8] They normally cause infection in rodents, but do not cause disease in them.[8] Humans may become infected with hantaviruses through contact with rodent urine, saliva, or feces. While many hantaviruses cause either of the two diseases, some are not known to cause illness, such as the Prospect Hill orthohantavirus.[7]
Transmission
Hantaviruses are transmitted by contact with the bodily fluids of rodents, particularly from saliva from bites and especially from inhalation of viral particles from urine and feces in aerosols. The manner of transmission is the same for both diseases caused by hantaviruses. Among the HCPS-causing hantaviruses is the Andes orthohantavirus, which is the only hantavirus confirmed to be capable of spreading from person to person, though this is rare.[4][7]
Infections have almost entirely been linked to contact with rodent excrement; however, in 2005 and 2019, human-to-human transmission of the Andes virus was reported in South America.[9]
Diagnosis
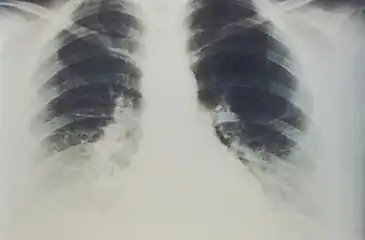
In terms of the evaluation of this infection the following is done:[10]
- Chest X-ray (pulmonary edema)
- Blood workup (thrombocytopenia)
- Immunofluorescent or immunoblot assay (ELISA utilizing IgM)
Prevention
The best prevention against contracting hantavirus is to eliminate or minimize contact with rodents in the home, workplace, or campsite.[11] As the virus can be transmitted by rodent saliva, excretions, and bites, control of rats and mice in areas frequented by humans is key for disease prevention. General prevention can be accomplished by disposing of rodent nests, sealing any cracks and holes in homes where mice or rats could enter, setting traps, or laying down poisons or using natural predators such as cats in the home.[12]
The duration that hantaviruses remain infectious in the environment varies based on factors such as the rodent's diet, temperature, humidity, and whether indoors or outdoors. The viruses have been demonstrated to remain active for two to three days at normal room temperature, while ultraviolet rays in direct sunlight kills them within a few hours. However, rodent droppings or urine of indeterminate age should always be treated as infectious.[13][14][15]
Vaccine
As of 2021, there are no US FDA-approved vaccines against hantaviruses. However, whole virus inactivated bivalent vaccines against Hantaan virus and Seoul virus are available in China and South Korea. In both countries, the use of the vaccine, combined with other preventive measures, has significantly reduced the incidence of hantavirus infections. Apart from these vaccines, four types of vaccines have been researched: DNA vaccines targeting the M genome segment and the S genome segment, subunit vaccines that use recombinant Gn, Gc, and N proteins of the virus, virus vector vaccines that have recombinant hantavirus proteins inserted in them, and virus-like particle vaccines that contain viral proteins but lack genetic material. Of these, only DNA vaccines have entered into clinical trials.[16][17]
Treatment
Ribavirin may be a drug for HPS and HFRS but its effectiveness remains unknown, still, spontaneous recovery is possible with supportive treatment. People with suspected hantavirus infection may be admitted to the hospital, given oxygen and mechanical ventilation support to help them breathe during the acute pulmonary stage with severe respiratory distress.[12][18] Immunotherapy, administration of human neutralizing antibodies during acute phases of Hantavirus, has only been studied in mice, hamsters, and rats. There are no reports of controlled clinical trials.[19]
Epidemiology
Hantavirus infections have been reported from all continents except Australia. Regions especially affected by hemorrhagic fever with renal syndrome include China, the Korean Peninsula, Russia (Hantaan, Puumala and Seoul viruses), and northern and western Europe (Puumala and Dobrava virus). Regions with the highest incidences of hantavirus pulmonary syndrome include Argentina, Chile, Brazil, the United States, Canada, and Panama.
Africa
In 2010, a novel hantavirus, Sangassou virus was isolated in Africa which causes hemorrhagic fever with renal syndrome.[20]
Asia
In China, Hong Kong, the Korean Peninsula and Russia, hemorrhagic fever with renal syndrome is caused by Hantaan, Puumala and Seoul viruses.[21]
China
In March 2020, a man from Yunnan tested positive for Hantavirus. He died while travelling to Shandong for work on a chartered bus. According to the Global Times reports, around 32 other people have been tested for the virus.[22][23][24]
Australia
As of 2005, there were no human infections reported in Australia, though rodents were found to carry antibodies.[25]
Europe
In Europe two hantaviruses – Puumala and Dobrava-Belgrade viruses – are known to cause hemorrhagic fever with renal syndrome.[26] Puumala usually causes a generally mild disease, nephropathia epidemica, which typically presents with fever, headache, gastrointestinal symptoms, impaired renal function and blurred vision. Dobrava infections are similar, except that they often also have hemorrhagic complications.
Puumala virus is carried by its rodent host, the bank vole (Clethrionomys glareolus), and is present throughout most of Europe, except for the Mediterranean region. There are four known Dobrava virus genotypes, each carried by a different rodent species. Genotype Dobrava is found in the yellow-necked mouse (Apodemus flavicollis); genotypes Saaremaa and Kurkino in the striped field mouse (Apodemus agrarius), and genotype Sochi in the Black Sea field mouse (Apodemus ponticus).
In 2017 alone, the Robert Koch Institute (RKI) in Germany received 1,713 notifications of hantavirus infections.[27]
North America
Canada
The primary cause of the disease in Canada is Sin Nombre virus-infected deer mice. Between 1989 and 2014, there were a total of 109 confirmed cases, with the death rate estimated at 29%.[28] The virus exists in deer mice nationwide, but cases were concentrated in western Canada (British Columbia, Alberta, Saskatchewan and Manitoba) with only one case in eastern Canada. In Canada "[a]ll cases occurred in rural settings and approximately 70% of the cases have been associated with domestic and farming activities."[28]
United States
In the United States, minor cases of HPS include Sin Nombre orthohantavirus, New York orthohantavirus, Bayou orthohantavirus, and possibly Black Creek Canal orthohantavirus.
As of January 2017, 728 cases of hantavirus had been reported in the United States cumulatively since 1995, across 36 states, not including cases with presumed exposure outside the United States. More than 96% of cases have occurred in states west of the Mississippi River. The top 10 states by number of cases reported (which differs slightly from a count ordered by the state of original exposure) were New Mexico (109), Colorado (104), Arizona (78), California (61), Washington (50), Texas (45), Montana (43), Utah (38), Idaho (21), and Oregon (21); 36% of the total reported cases have resulted in death.[29]
Mexico
In Mexico, rodents have been found to carry hantaviruses include Thomas's giant deer mouse (Megadontomys thomasi), the pack rat Neotoma picta, Orizaba deer mouse (Peromyscus beatae), Western harvest mouse (Reithrodontomys megalotis) and Sumichrast's harvest mouse (Reithrodontomys sumichrasti).[30]
South America
Agents of HPS found in South America include the Andes virus (also called Oran, Castelo de Sonhos – Portuguese for "Castle of Dreams", Lechiguanas, Juquitiba, Araraquara, and Bermejo virus, among many other synonyms), which is the only hantavirus that has shown an interpersonal form of transmission, and the Laguna Negra virus, an extremely close relative of the previously known Rio Mamore virus.
Rodents that have been shown to carry hantaviruses include Abrothrix longipilis and Oligoryzomys longicaudatus.[31]
History
Hantavirus HFRS was likely first referenced in China in the 12th century. The first clinical recognition was in 1931 in northeast China. Around the same time in the 1930s, NE was identified in Sweden. HFRS came to the recognition of western physicians during the Korean War between 1951 and 1954 when more than 3,000 United Nations soldiers fell ill in an outbreak. In 1976, the first pathogenic hantavirus, the Hantaan orthohantavirus, was isolated from rodents near the Hantan River in South Korea. Other prominent hantaviruses that cause HFRS, including the Dobrava-Belgrade orthohantavirus, Puumala orthohantavirus, and Seoul orthohantavirus, were identified in the years after then and are collectively referred to as the Old World hantaviruses.[6]
In 1993, an outbreak of HCPS, then unrecognized, occurred in the Four Corners region of the United States and led to the discovery of the Sin Nombre orthohantavirus. Since then, approximately 43 hantavirus strains, of which 20 are pathogenic, have been found in the Americas and are referred to as the New World hantaviruses. This includes the Andes orthohantavirus, one of the primary causes of HCPS in South America and the only hantavirus known to be capable of person-to-person transmission.[6]
In late medieval England a mysterious sweating sickness swept through the country in 1485 just before the Battle of Bosworth Field. Noting that the symptoms overlap with hantavirus pulmonary syndrome, several scientists have theorized that the virus may have been the cause of the disease.[32][33] The hypothesis was criticized because sweating sickness was recorded as being transmitted from human to human, whereas hantaviruses were not known to spread in this way.[34]
References
- 1 2 3 4 "CDC - Hemorrhagic Fever with Renal Syndrome (HFRS) - Hantavirus". www.cdc.gov. 22 February 2019. Archived from the original on 16 November 2019. Retrieved 29 March 2021.
- 1 2 3 4 "Signs & Symptoms | Hantavirus | DHCPP | CDC". www.cdc.gov. 22 February 2019. Archived from the original on 20 March 2021. Retrieved 28 March 2021.
- 1 2 3 "CDC - Hantavirus". www.cdc.gov. 9 September 2020. Archived from the original on 8 February 2012. Retrieved 25 March 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Avšič-Županc T, Saksida A, Korva M (2019). "Hantavirus infections". Clin Microbiol Infect. 21S: e6–e16. doi:10.1111/1469-0691.12291. PMID 24750436. Archived from the original on 21 October 2020. Retrieved 21 April 2020.
- ↑ "ICTV 9th Report (2011) – Negative Sense RNA Viruses – Bunyaviridae". International Committee on Taxonomy of Viruses (ICTV). Archived from the original on 11 December 2018. Retrieved 31 January 2019.
Hanta: from Hantaan, river in South Korea near where type virus was isolated.
- 1 2 3 4 Jiang H, Zheng X, Wang L, Du H, Wang P, Bai X (2017). "Hantavirus infection: a global zoonotic challenge". Virol Sin. 32 (1): 32–43. doi:10.1007/s12250-016-3899-x. PMC 6598904. PMID 28120221.
- 1 2 3 Gravinatti ML, Barbosa CM, Soares RM, Gregori F (2020). "Synanthropic rodents as virus reservoirs and transmitters". Rev Soc Bras Med Trop. 53: e20190486. doi:10.1590/0037-8682-0486-2019. PMC 7083353. PMID 32049206.
- 1 2 "Rodent-borne diseases". European Centre for Disease Prevention and Control. Archived from the original on 2018-06-23. Retrieved 2018-06-04.
- ↑ Martinez VP, Bellomo C, San Juan J, Pinna D, Forlenza R, Elder M, Padula PJ (2005). "Person-to-person transmission of Andes virus". Emerging Infectious Diseases. 11 (12): 1848–1853. doi:10.3201/eid1112.050501. PMC 3367635. PMID 16485469.
- ↑ Moore, Ross A.; Griffen, David (2021). "Hantavirus Syndrome". StatPearls. StatPearls Publishing. Archived from the original on 20 March 2021. Retrieved 27 November 2021.
- ↑ "Hantavirus Prevention". CDC. USA.gov. 2019-02-22. Archived from the original on 2021-03-19. Retrieved 2021-03-25.
- 1 2 "Hantavirus: Canadian Lung Association". Canadian Lung Association. 26 November 2015. Archived from the original on 2 March 2011. Retrieved 23 April 2018.
- ↑ Washington State Department of Labor & Industries (April 2010). "Hantavirus Pulmonary Syndrome (HPS) and the workplace". wisha-training.lni.wa.gov. Archived from the original on 2017-02-19. Retrieved 2017-08-25.
- ↑ Canadian Centre for Occupational Health and Safety (2016-01-08). "Hantavirus : OSH Answers". www.ccohs.ca. Archived from the original on 2017-08-26. Retrieved 2017-08-25.
- ↑ Washington State Department of Health (2017). "Hantavirus". www.doh.wa.gov. Archived from the original on 2017-08-26. Retrieved 2017-08-25.
- ↑ Liu R, Ma H, Shu J, Zhang Q, Han M, Liu Z, Jin X, Zhang F, Wu X (2020). "Vaccines and Therapeutics Against Hantaviruses". Front Microbiol. 10: 2989. doi:10.3389/fmicb.2019.02989. PMC 7002362. PMID 32082263.
- ↑ Brocato RL, Hooper JW (2019). "Progress on the Prevention and Treatment of Hantavirus Disease". Viruses. 11 (7): 610. doi:10.3390/v11070610. PMC 6669544. PMID 31277410.
- ↑ "CDC – Diagnosing and Treating Hantavirus Pulmonary Syndrome (HPS) – Hantavirus". www.cdc.gov. Archived from the original on 2016-11-20. Retrieved 2016-11-09.
- ↑ Jonsson, Colleen B.; Hooper, Jay; Mertz, Gregory (2008-04-01). "Treatment of hantavirus pulmonary syndrome". Antiviral Research. Special Issue: Treatment of highly pathogenic RNA viral infections. 78 (1): 162–169. doi:10.1016/j.antiviral.2007.10.012. PMC 2810485. PMID 18093668.
- ↑ Klempa B, Witkowski PT, Popugaeva E, Auste B, Koivogui L, Fichet-Calvet E, Strecker T, Ter Meulen J, Krüger DH (2012). "Sangassou Virus, the First Hantavirus Isolate from Africa, Displays Genetic and Functional Properties Distinct from Those of Other Murinae-Associated Hantaviruses". Journal of Virology. 86 (7): 3819–3827. doi:10.1128/JVI.05879-11. PMC 3302504. PMID 22278233.
- ↑ "男生患漢坦食署Hea補鑊 住處附近僅派傳單". Archived from the original on 2020-04-23. Retrieved 2021-03-25.
- ↑ "Man in China dies after testing positive for hantavirus – what exactly is it?". The Free Press Journal. Archived from the original on 2020-03-24. Retrieved 2020-03-24.
- ↑ "What is hantavirus? Man in China tests positive after dying of infection spread by rodents". Newsweek. 2020-03-24. Archived from the original on 2020-03-24. Retrieved 2020-03-24.
- ↑ Leonardi, Anthony (March 24, 2020). "'Do not panic, unless you plan to eat rats': Man who died in China tests positive for hantavirus". Washington Examiner. Archived from the original on March 24, 2020. Retrieved March 24, 2020.
- ↑ Bi, P.; Cameron, S.; Higgins, G.; Burrell, C. (2005). "Are humans infected by Hantaviruses in Australia?". Internal Medicine Journal. 35 (11): 672–674. doi:10.1111/j.1445-5994.2005.00954.x. PMID 16248862. S2CID 37603482.
- ↑ Vapalahti O, Mustonen J, Lundkvist A, Henttonen H, Plyusnin A, Vaheri A (2003). "Hantavirus infections in Europe". The Lancet Infectious Diseases. 3 (10): 653–661. doi:10.1016/S1473-3099(03)00774-6. PMID 14522264.
- ↑ Hofmann J, Krüger DH, Loyen M (2018). "Hantavirus-Infektionen in Deutschland – ein Rückblick auf das Ausbruchsjahr 2017". Epid Bull. 15: 143–146. doi:10.17886/EpiBull-2018-018.
- 1 2 Drebot, Jones S.; Grolla, A.; Safronetz, D.; Strong, J. E.; Kobinger, G.; Lindsay, R. L. (4 June 2015). Hantavirus pulmonary syndrome in Canada: An overview of clinical features, diagnostics, epidemiology and prevention. Canada Communicable Disease Report (Report). Vector-borne diseases in Canada. Vol. 41–06. Winnipeg, MB: National Microbiology Laboratory, Public Health Agency of Canada. p. 40. ISSN 1481-8531. Archived from the original on 19 July 2017. Retrieved 25 March 2021.
- ↑ "Hantavirus Cases, by State of Reporting | Hantavirus | DHCPP". Centers for Disease Control and Prevention. 2017-07-19. Archived from the original on 2017-08-26. Retrieved 2017-08-25.
- ↑ Kariwa H, Yoshida H, Sánchez-Hernández C, Romero-Almaraz Mde L, Almazán-Catalán JA, Ramos C, Miyashita D, Seto T, Takano A, Totani M, Murata R, Saasa N, Ishizuka M, Sanada T, Yoshii K, Yoshimatsu K, Arikawa J, Takashima I (2012). "Genetic diversity of hantaviruses in Mexico: Identification of three novel hantaviruses from Neotominae rodents". Virus Research. 163 (2): 486–494. doi:10.1016/j.virusres.2011.11.013. PMID 22138671.
- ↑ Medina RA, Torres-Perez F, Galeno H, Navarrete M, Vial PA, Palma RE, Ferres M, Cook JA, Hjelle B (2008). "Ecology, Genetic Diversity, and Phylogeographic Structure of Andes Virus in Humans and Rodents in Chile". Journal of Virology. 83 (6): 2446–2459. doi:10.1128/JVI.01057-08. PMC 2648280. PMID 19116256.
- ↑ Thwaites G, Taviner M, Gant V (1997). "The English Sweating Sickness, 1485 to 1551". New England Journal of Medicine. 336 (8): 580–582. doi:10.1056/NEJM199702203360812. PMID 9023099.
- ↑ Taviner M, Thwaites G, Gant V (1998). "The English sweating sickness, 1485–1551: a viral pulmonary disease?". Medical History. 42 (1): 96–98. doi:10.1017/S0025727300063365. PMC 1043971. PMID 9536626.
- ↑ Bridson, Eric (2001). "English 'sweate' (Sudor Anglicus) and Hantavirus pulmonary syndrome, The". British Journal of Biomedical Science. 58 (1): 1–6. PMID 11284216. Archived from the original on 2006-03-24.