Juvenile hyaline fibromatosis
| Juvenile hyaline fibromatosis | |
|---|---|
| Other names: Puretic syndrome[1] | |
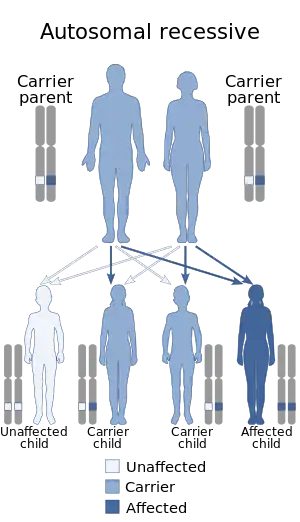 | |
| Autosomal recessive pattern is the inheritance manner of this condition | |
| Specialty | Dermatology |
Juvenile hyaline fibromatosis (also known as "Fibromatosis hyalinica multiplex juvenilis,"[2] "Murray–Puretic–Drescher syndrome"[2]) is a very rare, autosomal recessive disease due to mutations in capillary morphogenesis protein-2 (CMG-2 gene). It occurs from early childhood to adulthood, and presents as slow-growing, pearly white or skin-colored dermal or subcutaneous papules or nodules on the face, scalp, and back, which may be confused clinically with neurofibromatosis.[3] The World Health Organization, 2020, reclassified the papules and nodules that occur in juvenile hyaline firbromatosis as one of the specific benign types of tumors in the category of fibroblastic and myofibroblastic tumors.[4]
Signs and symptoms
.png.webp)
This condition is characterised by abnormal growth of hyalinized fibrous tissue with cutaneous, mucosal, osteoarticular and systemic involvement.
Clinical features include extreme pain at minimal handling in a newborn, gingival hypertrophy, subcutaneous nodules, painful joint stiffness and contractures, muscle weakness and hypotonia.
Genetics
This condition is due to mutations in the anthrax toxin receptor-2 (ANTXR2) gene. This gene is also known as capillary morphogenesis protein-2.
This gene is located on the long arm of chromosome 4 (4q21.21).
Diagnosis
The diagnosis of this condition is done via the following:[5]
- Medical history
- Physical exam
- Lab test
- Genetic test
Management
There is no presently known curative treatment for this condition.
Management is supportive
Prognosis
This is very poor with a median age at death of 15 months.
Epidemiology
84 cases have been reported as of 2018.[6]
See also
References
- ↑ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Juvenile hyaline fibromatosis". www.orpha.net. Archived from the original on 15 November 2017. Retrieved 28 April 2019.
- 1 2 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- ↑ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). Page 989. McGraw-Hill. ISBN 0-07-138076-0.
- ↑ Sbaraglia M, Bellan E, Dei Tos AP (April 2021). "The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives". Pathologica. 113 (2): 70–84. doi:10.32074/1591-951X-213. PMC 8167394. PMID 33179614.
- ↑ "Hyaline fibromatosis syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 18 March 2021. Retrieved 19 April 2022.
- ↑ Casas-Alba D, Martínez-Monseny A, Pino-Ramírez RM, Alsina L, Castejón E, Navarro-Vilarrubí S, Pérez-Dueñas B, Serrano M, Palau F, García-Alix A (2018) Hyaline fibromatosis syndrome: Clinical update and phenotype-genotype correlations. Hum Mutat doi: 10.1002/humu.23638
External links
| Classification | |
|---|---|
| External resources |
|