Langerhans cell
| Langerhans cell | |
|---|---|
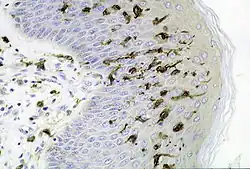 Section of skin showing large numbers of Langerhans cells in the epidermis. (M. ulcerans infection, S100 immunoperoxidase stain.) | |
| Details | |
| System | Immune system |
| Location | Skin and mucosa |
| Function | Dendritic cell |
| Identifiers | |
| MeSH | D007801 |
| FMA | 63072 |
| Anatomical terms of microanatomy | |
Langerhans cells (LC) are tissue-resident macrophages of the skin,[2] and contain organelles called Birbeck granules. They are present in all layers of the epidermis and are most prominent in the stratum spinosum.[3] They also occur in the papillary dermis, particularly around blood vessels,[3] as well as in the mucosa of the mouth, foreskin, and vaginal epithelium.[4] They can be found in other tissues, such as lymph nodes, particularly in association with the condition Langerhans cell histiocytosis (LCH).
Function
In skin infections, the local Langerhans cells take up and process microbial antigens to become fully functional antigen-presenting cells.
Generally, tissue-resident macrophages are involved in immune homeostasis and the uptake of apoptotic bodies. However, Langerhans cells can also take on a dendritic cell-like phenotype and migrate to lymph nodes to interact with naive T-cells.
Langerhans cells derive from primitive erythro-myeloid progenitors that arise in the yolk sac outside the embryo in the first trimester of pregnancy, and under normal circumstances persist throughout life, being replenished by local proliferation as necessary. If the skin becomes severely inflamed, perhaps because of infection, blood monocytes are recruited to the affected region and differentiate into replacement LCs.[5]
Langerin is a protein found in Langerhans cells,[6] and dendritic cells.[7]
Clinical significance
Langerhans cell histiocytosis
In the rare disease Langerhans cell histiocytosis (LCH), an excess of cells similar to these cells are produced. However LCH cells stain positive to CD14 which is a monocyte marker and shows a different, hematopoietic origin for the disorder.[8] LCH can cause damage to skin, bone and other organs.
HIV
Langerhans cells may be initial cellular targets in the sexual transmission of HIV,[9] and may be a target, reservoir, and vector of dissemination.[10]
Langerhans cells have been observed in foreskin, vaginal, and oral mucosa of humans; the lower concentrations in oral mucosa suggest that it is not a likely source of HIV infection relative to foreskin and vaginal mucosa.[4]
Human papillomavirus
High-risk human papillomaviruses (HPV) are sexually transmitted viruses causally associated with several cancers including cervical, vaginal, anal, and head and neck cancers that cause significant morbidity and mortality worldwide.[11][12][13][14] Over half of all cervical cancer cases are associated with HPV16, the most common of the cancer-causing high-risk genotypes.[15] During its natural life cycle, HPV16 infects the basal cells of the epithelium and interacts with Langerhans cells within the epithelial layer,[16] which are responsible for initiating immune responses against epithelial invading pathogens.[17] However, HPV does not activate Langerhans cells in vitro, and this may represent a key mechanism by which HPV evades immune detection in vivo.[18][19][20][21] Specifically, HPV16 entry into Langerhans cells via the annexin A2/S100A10 heterotetramer results in suppressive signaling and lack of Langerhans cell-mediated immune responses.[22] This Langerhans cell-targeted immune escape mechanism seems to be conserved among different HPV genotypes enabling these viruses to remain undetected in the absence of other inflammatory events.[23] T cells exposed to these inactivated Langerhans cells are not anergic, and can be activated against HPV upon receiving the appropriate stimuli at a later time point.[24]
It was demonstrated that Langerhans cells in HPV-induced cervical lesions were spherical, lacked dendrites, and secreted the suppressive cytokine IL-10 in vivo.[25] The authors further demonstrated that the number of IL-10 secreting immunosuppressive Langerhans cells, and the amount of IL-10 produced in lesions, corresponded with the severity of histopathology and HPV viral load, providing evidence of an active immunosuppressive mechanism employed by HPV that targets Langerhans cells in vivo.
Dengue fever
Langerhans cells are also the initial target of the virus that causes dengue fever during its development.[26]
Declining function during ageing
During ageing the capacity of Langerhans cells to migrate declines.[27] This compromises immunity and exposes the skin to infectious diseases and cancer.
History
Langerhans cells are named after Paul Langerhans, a German physician and anatomist, who discovered the cells at the age of 21 while he was a medical student.[28] Because of their dendrite-like appearance, he mistakenly identified the cells as part of the nervous system.[29]
See also
References
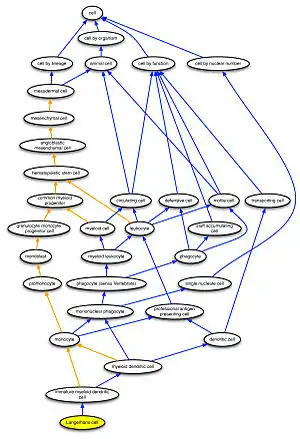
- ↑ Masci, Anna; Arighi, Cecilia N; Diehl, Alexander D; Lieberman, Anne E; Mungall, Chris; Scheuermann, Richard H; Smith, Barry; Cowell, Lindsay G (2009). "An improved ontological representation of dendritic cells as a paradigm for all cell types". BMC Bioinformatics. 10: 70. doi:10.1186/1471-2105-10-70. PMC 2662812. PMID 19243617.
- ↑ Doebel, Thomas; Voisin, Benjamin; Nagao, Keisuke (2017-11-01). "Langerhans Cells – The Macrophage in Dendritic Cell Clothing". Trends in Immunology. 38 (11): 817–828. doi:10.1016/j.it.2017.06.008. ISSN 1471-4906. PMID 28720426.
- 1 2 Young, Barbara; Heath, John W. (2000). Wheater's Functional Histology (4th ed.). Churchill Livingstone. p. 162. ISBN 0-443-05612-9.
- 1 2 Hussain, LA; Lehner, T (1995). "Comparative investigation of Langerhans' cells and potential receptors for HIV in oral, genitourinary and rectal epithelia". Immunology. 85 (3): 475–84. PMC 1383923. PMID 7558138.
- ↑ Collin, Matthew; Milne, Paul (2016). "Langerhans cell origin and regulation". Current Opinion in Hematology. 23 (1): 28–35. doi:10.1097/MOH.0000000000000202. PMC 4685746. PMID 26554892.
- ↑ Valladeau, Jenny; Dezutter-Dambuyant, Colette; Saeland, Sem (2003). "Langerin/CD207 Sheds Light on Formation of Birbeck Granules and Their Possible Function in Langerhans Cells". Immunologic Research. 28 (2): 93–107. doi:10.1385/IR:28:2:93. PMID 14610287. S2CID 37296843.
- ↑ Poulin, Lionel Franz; Henri, Sandrine; de Bovis, Béatrice; Devilard, Elisabeth; Kissenpfennig, Adrien; Malissen, Bernard (2007). "The dermis contains langerin+ dendritic cells that develop and function independently of epidermal Langerhans cells" (PDF). Journal of Experimental Medicine. 204 (13): 3119–31. doi:10.1084/jem.20071724. PMC 2150992. PMID 18086861. Archived from the original (PDF) on 2018-07-19. Retrieved 2018-11-04.
- ↑ "NCI Summary View > Urology - Yale School of Medicine". medicine.yale.edu. Archived from the original on 17 June 2019. Retrieved 19 April 2018.
- ↑ Kawamura, Tatsuyoshi; Kurtz, Stephen E.; Blauvelt, Andrew; Shimada, Shinji (2005). "The role of Langerhans cells in the sexual transmission of HIV". Journal of Dermatological Science. 40 (3): 147–55. doi:10.1016/j.jdermsci.2005.08.009. PMID 16226431.
- ↑ Dezutter-Dambuyant, C; Charbonnier, AS; Schmitt, D (December 1995). "Cellules dendritiques épithéliales et infection par HIV-1 in vivo et in vitro" [Epithelial dendritic cells and HIV-1 infection in vivo and in vitro]. Pathologie Biologie (in French). 43 (10): 882–8. PMID 8786894.
- ↑ Walboomers, J. M.; Jacobs, M. V.; Manos, M. M.; Bosch, F. X.; Kummer, J. A.; Shah, K. V.; Snijders, P. J.; Peto, J.; Meijer, C. J. (1999-09-01). "Human papillomavirus is a necessary cause of invasive cervical cancer worldwide". The Journal of Pathology. 189 (1): 12–19. doi:10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. ISSN 0022-3417. PMID 10451482.
- ↑ Arbyn, M.; Castellsagué, X.; de Sanjosé, S.; Bruni, L.; Saraiya, M.; Bray, F.; Ferlay, J. (2011-12-01). "Worldwide burden of cervical cancer in 2008". Annals of Oncology. 22 (12): 2675–2686. doi:10.1093/annonc/mdr015. ISSN 1569-8041. PMID 21471563.
- ↑ Haedicke, Juliane; Iftner, Thomas (2013-09-01). "Human papillomaviruses and cancer". Radiotherapy and Oncology. 108 (3): 397–402. doi:10.1016/j.radonc.2013.06.004. ISSN 1879-0887. PMID 23830197.
- ↑ HOFFMANN, MARKUS; QUABIUS, ELGAR S.; TRIBIUS, SILKE; HEBEBRAND, LENA; GÖRÖGH, TIBOR; HALEC, GORDANA; KAHN, TOMAS; HEDDERICH, JÜRGEN; RÖCKEN, CHRISTOPH (2013-05-01). "Human papillomavirus infection in head and neck cancer: The role of the secretory leukocyte protease inhibitor". Oncology Reports. 29 (5): 1962–1968. doi:10.3892/or.2013.2327. ISSN 1021-335X. PMC 3658815. PMID 23467841.
- ↑ Bosch, F. X.; Manos, M. M.; Muñoz, N.; Sherman, M.; Jansen, A. M.; Peto, J.; Schiffman, M. H.; Moreno, V.; Kurman, R. (1995-06-07). "Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group". Journal of the National Cancer Institute. 87 (11): 796–802. doi:10.1093/jnci/87.11.796. ISSN 0027-8874. PMID 7791229.
- ↑ Stanley, M. A.; Pett, M. R.; Coleman, N. (2007-12-01). "HPV: from infection to cancer". Biochemical Society Transactions. 35 (Pt 6): 1456–1460. doi:10.1042/BST0351456. ISSN 0300-5127. PMID 18031245.
- ↑ Merad, Miriam; Ginhoux, Florent; Collin, Matthew (2008-12-01). "Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells". Nature Reviews. Immunology. 8 (12): 935–947. doi:10.1038/nri2455. ISSN 1474-1741. PMID 19029989. S2CID 22286432.
- ↑ Fausch, Steven C.; Da Silva, Diane M.; Rudolf, Michael P.; Kast, W. Martin (2002-09-15). "Human papillomavirus virus-like particles do not activate Langerhans cells: a possible immune escape mechanism used by human papillomaviruses". Journal of Immunology. 169 (6): 3242–3249. doi:10.4049/jimmunol.169.6.3242. ISSN 0022-1767. PMID 12218143.
- ↑ Fausch, Steven C.; Da Silva, Diane M.; Kast, W. Martin (2003-07-01). "Differential uptake and cross-presentation of human papillomavirus virus-like particles by dendritic cells and Langerhans cells". Cancer Research. 63 (13): 3478–3482. ISSN 0008-5472. PMID 12839929.
- ↑ Fausch, Steven C.; Fahey, Laura M.; Da Silva, Diane M.; Kast, W. Martin (2005-06-01). "Human papillomavirus can escape immune recognition through Langerhans cell phosphoinositide 3-kinase activation". Journal of Immunology. 174 (11): 7172–7178. doi:10.4049/jimmunol.174.11.7172. ISSN 0022-1767. PMID 15905561.
- ↑ Fahey, Laura M.; Raff, Adam B.; Da Silva, Diane M.; Kast, W. Martin (2009-11-15). "A major role for the minor capsid protein of human papillomavirus type 16 in immune escape". Journal of Immunology. 183 (10): 6151–6156. doi:10.4049/jimmunol.0902145. ISSN 1550-6606. PMC 2947488. PMID 19864613.
- ↑ Woodham, Andrew W.; Raff, Adam B.; Raff, Laura M.; Da Silva, Diane M.; Yan, Lisa; Skeate, Joseph G.; Wong, Michael K.; Lin, Yvonne G.; Kast, W. Martin (2014-05-15). "Inhibition of Langerhans cell maturation by human papillomavirus type 16: a novel role for the annexin A2 heterotetramer in immune suppression". Journal of Immunology. 192 (10): 4748–4757. doi:10.4049/jimmunol.1303190. ISSN 1550-6606. PMC 4019435. PMID 24719459.
- ↑ Da Silva, Diane M.; Movius, Carly A.; Raff, Adam B.; Brand, Heike E.; Skeate, Joseph G.; Wong, Michael K.; Kast, W. Martin (2014-03-01). "Suppression of Langerhans cell activation is conserved amongst human papillomavirus α and β genotypes, but not a μ genotype". Virology. 452–453: 279–286. doi:10.1016/j.virol.2014.01.031. ISSN 1096-0341. PMC 3987942. PMID 24606705.
- ↑ Woodham, Andrew W.; Yan, Lisa; Skeate, Joseph G.; van der Veen, Daniel; Brand, Heike H.; Wong, Michael K.; Da Silva, Diane M.; Kast, W. Martin (December 2016). "T cell ignorance is bliss: T cells are not tolerized by Langerhans cells presenting human papillomavirus antigens in the absence of costimulation". Papillomavirus Research (Amsterdam, Netherlands). 2: 21–30. doi:10.1016/j.pvr.2016.01.002. ISSN 2405-8521. PMC 4862606. PMID 27182559.
- ↑ Prata, Thiago Theodoro Martins; Bonin, Camila Mareti; Ferreira, Alda Maria Teixeira; Padovani, Cacilda Tezelli Junqueira; Fernandes, Carlos Eurico Dos Santos; Machado, Ana Paula; Tozetti, Inês Aparecida (2015-09-01). "Local immunosuppression induced by high viral load of human papillomavirus: characterization of cellular phenotypes producing interleukin-10 in cervical neoplastic lesions". Immunology. 146 (1): 113–121. doi:10.1111/imm.12487. ISSN 1365-2567. PMC 4552506. PMID 26059395.
- ↑ Martina BE, Koraka P, Osterhaus AD (October 2009). "Dengue virus pathogenesis: an integrated view". Clinical Microbiology Reviews. 22 (4): 564–81. doi:10.1128/CMR.00035-09. PMC 2772360. PMID 19822889.
- ↑ Pilkington, S; et al. (2018). "Lower levels of interleukin-1β gene expression are associated with impaired Langerhans' cell migration in aged human skin". Immunology. 153 (1): 60–70. doi:10.1111/imm.12810. PMC 5721243. PMID 28777886.
- ↑ Langerhans, Paul (1868). "Ueber die Nerven der menschlichen Haut" [On the nerves of the human skin]. Archiv für pathologische Anatomie und Physiologie und für klinische Medicin (in German). 44 (2–3): 325–37. doi:10.1007/BF01959006. S2CID 6282875.
- ↑ Online Mendelian Inheritance in Man (OMIM): Langerhans cell histiocytosis - 604856
External links
- Langerhans Cell Histiocytosis at eMedicine
- Illustration at trinity.edu at the Wayback Machine (archived January 27, 2004)
- Brun, Scott C.; Rubin, Peter A. D. (1997). "25 year old kickboxer with progressive proptosis". Digital Journal of Ophthalmology. 3 (26).
- Langerhans+Cells at the US National Library of Medicine Medical Subject Headings (MeSH)