Lateral canthotomy
| Lateral canthotomy | |
|---|---|
| Other names: Canthotomy, lateral orbital canthotomy (LOC) | |
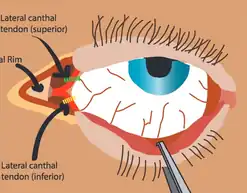 | |
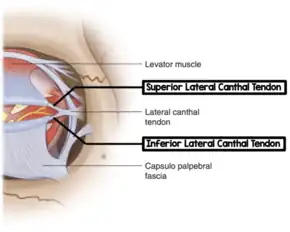
| Anatomy of the lateral canthus | |
| Specialty | Emergency medicine, ophthalmology |
| Indications | Orbital compartment syndrome[1] |
| Contraindications | Ruptured globe[1] |
| Steps | 1) Inject freezing 2) Clamp lateral canthus with a hemostat 3) Cut the lateral canthus with scissors 4) Pull away lower eyelid with forceps 5) Cut inferior tendon 6) If not sufficient cut the superior tendon[2] |
| Success | Decreased IOP, improved vision[1] |
| Complications | Globe injury, infection[1] |
Lateral canthotomy is an emergency procedure used to treat acute orbital compartment syndrome (OCS).[1] This may present with vision problems, increased intraocular pressure (IOP), decreased ability to move the eye, and dilation of the opposite pupil when a light is swung to shine in the affected eye.[1] Ideally it should be performed within two hours.[1] The procedure dose not take long to perform.[1]
The most common cause of acute OCS is an injury resulting in a bleeding behind the globe.[2] Other causes include spontaneous bleeding, recent eye surgery, and orbital infections.[1] Contraindications to the procedure include a ruptured globe.[1]
The procedure involves freezing the skin lateral to the eye with lidocaine with epinephrine.[1] The lateral corner of the eye is then briefly crushed with a hemostat.[1] A 1 to 2 cm cut is then made through this tissue with blunt tipped scissors.[1] The lower eyelid is then pulled away to expose the lateral canthal tendon.[1] The lower part of this tendon is than cut with the scissors.[1] If this is not sufficient the upper part may also be cut.[1]
Signs of success include a mobile lower eyelid, decreased IOP, and improved vision.[1] After the procedure the cut is left open and covered with a sterile dressing.[2] The head of the bed should be placed at 45 degrees, if possible.[3] Closure may occur by an ophthalmologist after a few days.[1]
Medical uses
Main indications
The primary use is suspected acute orbital compartment syndrome (OCS), plus one or more of the following:[4]
- Decreased visual acuity
- IOP >40 mmHg or marked difference in globe compressibility by palpation
- Proptosis
Other indications
Other indications (subjective and nonspecific) - if only secondary indications are present, get emergent ophthalmology consult prior to performing canthotomy.[4]
- Afferent pupillary defect
- Cherry red macula
- Ophthalmoplegia
- Nerve head pallor
- Significant eye pain
Contraindications
Technique
Preparation
The procedure is generally done with the person lying flat on their back.[1]
Steps
Steps include:[1]
- Consider sedation for procedure, if time allows.
- Begin by freezing the site of the incision. Using a 25-gauge needle, inject approximately 2 ml of 1% to 2% lidocaine with epinephrine into the lateral canthus, pointing away from the globe, in the affected eye.
- As the local anesthetic takes effect, use normal saline to flush any debris and foreign objects from the canthus and eye.
- Use a hemostat to gently crimp the lateral corner of the inferior eyelid. This step serves two functions: it will help establish the landmark for where to eventually cut, but also make the skin thinner for an easier cutting.
- Raise the skin around the aforementioned landmark using forceps while simultaneously using scissor to make a 1 to 2 cm cut at the landmark. The incision should be made from the lateral canthus and should be extended laterally.
- Use the blunt dissection technique until all tissue is out of the way, and the lateral canthal tendon is identified.
- Once the inferior crus of the lateral canthal tendon is identified, redirect the scissors inferiorly and strum the tendon. Once the tendon is strummed, cut the fibers of the tendon until complete laxity of the lower eyelid is achieved.
- Recheck the intraocular pressure. If the pressure is still elevated, this procedure can be repeated on the superior crus of the lateral canthal tendon.
.jpg.webp) Step 1
Step 1.jpg.webp) Step 2
Step 2.jpg.webp) Step 3
Step 3.jpg.webp) Step 4
Step 4.jpg.webp) Step 5
Step 5
Equipment
.jpg.webp)
- Betadine prep
- Sterile drape or towels
- Lidocaine with epi
- Syringe with 27-30ga needle
- Normal saline for irrigation
- Straight hemostat or needle driver
- Iris or suture scissors
- Forceps
Success
Complications
Risks of the procedure is relatively low.[2]
- Incomplete cantholysis
- Procedure caused globe or surrounding structure injury (rare)
- Loss of adequate lower lid suspension
- Bleeding
- Infection
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Desai, NM; Shah, Su (January 2021). "Lateral Orbital Canthotomy". PMID 32491408.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 Ballard, SR; Enzenauer, RW; O'Donnell, T; Fleming, JC; Risk, G; Waite, AN (2009). "Emergency lateral canthotomy and cantholysis: a simple procedure to preserve vision from sight threatening orbital hemorrhage". Journal of special operations medicine : a peer reviewed journal for SOF medical professionals. 9 (3): 26–32. PMID 19739474.
- ↑ "Orbital Compartment Syndrome" (PDF). MAGPAS AIr Ambulance. June 2018. Archived (PDF) from the original on 11 July 2021. Retrieved 14 March 2021.
- 1 2 McInnes, G; Howes, DW (January 2002). "Lateral canthotomy and cantholysis: a simple, vision-saving procedure". CJEM. 4 (1): 49–52. doi:10.1017/s1481803500006060. PMID 17637149.
- ↑ Scofi J. Lateral canthotomy. In: Shah K, Mason C, eds. Essential Emergency Procedures. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2015:(Ch) 17.
![]() This article incorporates creative commons material from the websites WikEM.org."Canthotomy - WikEM". wikem.org. Archived from the original on 13 August 2020. Retrieved 13 March 2021.
This article incorporates creative commons material from the websites WikEM.org."Canthotomy - WikEM". wikem.org. Archived from the original on 13 August 2020. Retrieved 13 March 2021.
External links
- MAGPAS Air Ambulance Archived 2021-07-11 at the Wayback Machine
- EM:RAP Smart Card Archived 2021-08-28 at the Wayback Machine
- Resus simulation Archived 2021-08-28 at the Wayback Machine