Orbital cellulitis
| Orbital cellulitis | |
|---|---|
| Other names: Postseptal cellulitis[1] | |
 | |
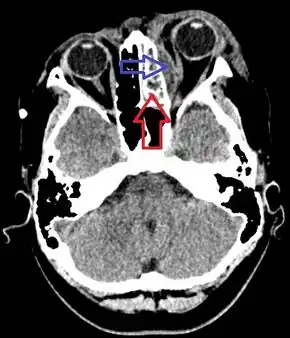
| Orbital cellulitis of the right eye | |
| Specialty | Ophthalmology |
| Symptoms | Eyelid redness and swelling, fever, pain with eye movement, double vision, vision loss, bulging of the eye[2][3] |
| Complications | Cavernous sinus thrombosis, meningitis[3] |
| Causes | Complication of bacterial sinusitis, local skin injury, tooth infection[3] |
| Diagnostic method | Based on symptoms, supported by medical imaging[3] |
| Differential diagnosis | Preseptal cellulitis, retinoblastoma, leukemia, giant cell arteritis[2][3] |
| Treatment | Intravenous antibiotics, surgery[3] |
| Prognosis | Generally good[4] |
| Frequency | Uncommon[2] |
Orbital cellulitis (OC) is inflammation, generally infectious in nature, of tissues within the eye socket.[2] Symptoms may include pain particularly with eye movement, double vision, vision loss, eyelid redness and swelling, fever, and bulging of the affected eye.[2][3] Complications may include cavernous sinus thrombosis, meningitis, and sepsis.[2][3]
It most commonly occurs due to spread of infection from the sinuses; though may occasionally occur after local injury to the skin, orbital fracture, from the teeth, or via the blood.[2][3] Diagnosis is based on symptoms and supported by medical imaging (CT scan or MRI.[3][5] Periorbital cellulitis, which is infection anterior to the orbital septum, may appear similar.[1][3]
Treatment is with intravenous antibiotics, such as ceftriaxone, piperacillin/tazobactam, or cefotaxime.[3] If injury to the skin has occurred and MRSA is common vancomycin may also be used.[3] While surgery is generally not required, it may be if certain complications occur.[3][6] Outcomes are generally good; though vision loss occurs in less than 10%.[2][4]
Orbital cellulitis is uncommon.[2][5] Children are more commonly affected (16 per million a year) than adults (1 per million a year).[2] Males may be slightly more frequently affected than females.[2] It occurs more often in winter.[2]
Signs and symptoms

Orbital cellulitis commonly presents with painful eye movement, sudden vision loss, chemosis, bulging of the infected eye, and limited eye movement. Along with these symptoms, patients typically have redness and swelling of the eyelid, pain, discharge, inability to open the eye, occasional fever and lethargy.
Complications
Complications include hearing loss, blood infection, meningitis, cavernous sinus thrombosis, cerebral abscess, and blindness.[7][8] It is possible that children experience more severe complications due to their immature immune system and because they have thinner orbital bones, which makes the infection easier to spread.[2][9]
Causes

Orbital cellulitis occurs commonly from bacterial infection spread via the paranasal sinuses, usually from a previous sinus infection. Other ways in which orbital cellulitis may occur are from blood stream infections or from eyelid skin infections. Upper respiratory infection, sinus infection, trauma to the eye, ocular or periocular infection, and systemic infection all increase one's risk of orbital cellulitis.
Staphylococcus aureus, Haemophilus influenzae B, Moraxella catarrhalis, Streptococcus pneumoniae, and beta-hemolytic streptococci are bacteria that can be responsible for orbital cellulitis.[10][9]
- Staphylococcus aureus is a gram-positive bacterium, which is the most common cause of staphylococcal infections. Staphylococcus aureus infection can spread from the skin to the orbit. This organism is able to produce toxins which promotes its virulence, leading to the inflammatory response seen in orbital cellulitis. Staphylococcus infections are identified by a cluster arrangement on gram stain. Staphylococcus aureus forms large yellow colonies when cultured (which is distinct from other Staph infections such as Staphylococcus epidermidis, which forms white colonies).
- Streptococcus pneumoniae is also a gram-positive bacterium responsible for orbital cellulitis due to its ability to infect the sinuses. Streptococcal bacteria can invade surrounding tissues, causing the inflammatory response seen in orbital cellulitis (similar to Staphyloccoccus aureus). Streptococcal infections are identified on culture by their formation of pairs or chains. Streptococcus pneumoniae produce green (alpha) hemolysis, or partial reduction of red blood cell hemoglobin.
Risk factors
Risk factors for the development of orbital cellulitis include, but are not limited to:[11][12]
- Recent upper respiratory illness
- Sinus infection
- Younger age
- Retained foreign bodies within the orbit
- Trauma
- Immunosuppression
- Systemic infection
- Dental infection
Diagnosis
Early diagnosis of orbital cellulitis is urgent, and it involves a complete and thorough physical examination. Common presenting signs include: a protruding eye (proptosis), eyelid edema (swelling), eye pain, vision loss, inability to move the eye completely (ophthalmoplegia), and fever. It is important to correlate physical findings with patient history and reported symptoms.[13]
CT scan and MRI of the orbits are two imaging modalities that are commonly used to aid in the diagnosis and monitoring of orbital cellulitis, as they can provide detailed images that can show the extent of inflammation along with possible abscess location, size, and involvement of surrounding structures.[2] Ultrasound has also been used as an imaging modality in the past, but it cannot provide the same level of detail as CT or MRI.[2]
Blood cultures, electrolytes, and a complete blood count (CBC) with differential showing elevated white blood cell count is a useful laboratory test that may aid in diagnosis.[13][10]
Differential diagnosis
A variety of diseases can present similarly including:[14]
- Inflammatory causes (thyroid eye disease, idiopathic orbital inflammatory syndrome, sarcoidosis, granulomatosis with polyangiitis)
- Infectious causes (subperiosteal abscess)
- Neoplastic, benign and malignant (dermoid cyst, capillary hemangioma, rhabdomyosarcoma, optic nerve glioma, lymphangioma, neurofibroma, leukemia)
- Trauma (orbital fracture, retrobulbar hemorrhage, orbital foreign body, carotid cavernous fistula)
- Malformation (congenital, vascular)
With both orbital and preseptal cellulitis have eyelid redness and swelling, generally only orbital cellulitis has pain with eye movement, bulging of the eye, or double vision.[1] Fever and swelling of the conjunctiva are also more common in orbital cellulitis.[1]
Treatment
Immediate treatment is important, and typically involves intravenous (IV) antibiotics and frequent observation (every 4–6 hours).[8][15]
- Antibiotics – Agents used often include vancomycin together with ceftriaxone or piperacillin-tazobactam.[1] If improvement is noted after 3 to 5 days, a person may be switched to antibiotics by mouth for 2–4 weeks.[1]
- Surgery – An abscess may form as a complication and surgery may be required to drain it. If a subperiosteal abscess is present in the medial orbit, drainage can be performed endoscopically.
- Corticosteroids - There is inadequate evidence to draw judgments about the use of steroids in the treatment of orbital cellulitis.[16]
Prognosis
Although orbital cellulitis is considered an emergency, the prognosis is good with prompt treatment.
In 1933, in the pre-antibiotic era, death occurred in 17% and permanent blindness in 20%.[17]
Epidemiology
Orbital cellulitis is uncommon, with children being more frequently affected than adults.[2] One study reported that children are approximately 16 times more likely to get orbital cellulitis compared to adults.[18] It is twice as common among male children compared to female children.[7] Some studies reported that orbital cellulitis follows a seasonal pattern, with the highest rates occurring during the fall and winter, which coincides with the higher rates of sinus infection during the colder months.[19]
References
- 1 2 3 4 5 6 Danishyar, A; Sergent, SR (January 2023). "Orbital Cellulitis". StatPearls. PMID 29939678.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Tsirouki, Theodora; Dastiridou, Anna I.; Ibánez flores, Nuria; Cerpa, Johnny Castellar; Moschos, Marilita M.; Brazitikos, Periklis; Androudi, Sofia (July 2018). "Orbital cellulitis". Survey of Ophthalmology. 63 (4): 534–553. doi:10.1016/j.survophthal.2017.12.001.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Preseptal and Orbital Cellulitis - Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 1 December 2022. Retrieved 2 July 2023.
- 1 2 Gordon, Abigail A.; Phelps, Paul O. (October 2020). "Management of preseptal and orbital cellulitis for the primary care physician". Disease-a-Month. 66 (10): 101044. doi:10.1016/j.disamonth.2020.101044. PMID 32622679.
- 1 2 Pelletier, J; Koyfman, A; Long, B (June 2023). "High risk and low prevalence diseases: Orbital cellulitis". The American journal of emergency medicine. 68: 1–9. doi:10.1016/j.ajem.2023.02.024. PMID 36893591.
- ↑ Wong, Stephanie J.; Levi, Jessica (July 2018). "Management of pediatric orbital cellulitis: A systematic review". International Journal of Pediatric Otorhinolaryngology. 110: 123–129. doi:10.1016/j.ijporl.2018.05.006. PMID 29859573.
- 1 2 Nageswaran, Savithri; Woods, Charles R.; Benjamin, Daniel K.; Givner, Laurence B.; Shetty, Avinash K. (2006). "Orbital Cellulitis in Children". The Pediatric Infectious Disease Journal. 25 (8): 695–699. doi:10.1097/01.inf.0000227820.36036.f1. ISSN 0891-3668. PMID 16874168. S2CID 23453070.
- 1 2 Garcia, G (2000-08-01). "Criteria for nonsurgical management of subperiosteal abscess of the orbit Analysis of outcomes 1988–1998". Ophthalmology. 107 (8): 1454–1456. doi:10.1016/s0161-6420(00)00242-6. ISSN 0161-6420. PMID 10919887.
- 1 2 Ruiz Carrillo, José Daniel; Vázquez Guerrero, Edwin; Mercado Uribe, Mónica Cecilia (2017-03-01). "Orbital cellulitis complicated by subperiosteal abscess due to Streptococcus pyogenes infection". Boletín Médico del Hospital Infantil de México (English Edition). 74 (2): 134–140. doi:10.1016/j.bmhime.2017.11.020. ISSN 2444-3409.
- 1 2 Howe, L.; Jones, N. S. (2004-12-01). "Guidelines for the management of periorbital cellulitis/abscess". Clinical Otolaryngology and Allied Sciences. 29 (6): 725–728. doi:10.1111/j.1365-2273.2004.00889.x. ISSN 1365-2273. PMID 15533168.
- ↑ Branson, Sara V.; McClintic, Elysa; Yeatts, R. Patrick (2018). "Septic Cavernous Sinus Thrombosis Associated With Orbital Cellulitis". Ophthalmic Plastic and Reconstructive Surgery. 35 (3): 272–280. doi:10.1097/iop.0000000000001231. ISSN 0740-9303. PMID 30320718. S2CID 52980567.
- ↑ O., Chaudhry, Imtiaz A. Al-Rashed, Waleed Arat, Yonca (2012). "The Hot Orbit: Orbital Cellulitis". Middle East African Journal of Ophthalmology. Medknow Publications & Media Pvt Ltd. 19 (1): 34–42. doi:10.4103/0974-9233.92114. OCLC 806537339. PMC 3277022. PMID 22346113.
- 1 2 Mejia, Ernesto; Braiman, Melvyn (2018), "Ocular Cellulitis", StatPearls, StatPearls Publishing, PMID 30020691, archived from the original on 2022-07-14, retrieved 2018-11-25
- ↑ Hood, C T (2009-07-24). "The Wills eye manual: office and emergency room diagnosis and treatment of eye disease". British Journal of Ophthalmology. 93 (8): 1127–1128. doi:10.1136/bjo.2008.152355. ISSN 0007-1161. S2CID 72653095.
- ↑ Mbbs, M P Ferguson; Fraco, A A McNab (1999). "Current treatment and outcome in orbital cellulitis". Australian and New Zealand Journal of Ophthalmology. 27 (6): 375–379. doi:10.1046/j.1440-1606.1999.00242.x. ISSN 0814-9763. PMID 10641894.
- ↑ Kornelsen, Emily; Mahant, Sanjay; Parkin, Patricia; Ren, Lily Yuxi; Reginald, Yohann A; Shah, Samir S; Gill, Peter J (2021-04-28). Cochrane Eyes and Vision Group (ed.). "Corticosteroids for periorbital and orbital cellulitis". Cochrane Database of Systematic Reviews. 2021 (4). doi:10.1002/14651858.CD013535.pub2.
- ↑ GAMBLE, R. C. (1933-10-01). "Acute Inflammations of the Orbit in Children". Archives of Ophthalmology. 10 (4): 483–497. doi:10.1001/archopht.1933.00830050059008. ISSN 0003-9950.
- ↑ Murphy, C; Livingstone, I; Foot, B; Murgatroyd, H; MacEwen, C J (2014-06-17). "Orbital cellulitis in Scotland: current incidence, aetiology, management and outcomes: Table 1". British Journal of Ophthalmology. 98 (11): 1575–1578. doi:10.1136/bjophthalmol-2014-305222. ISSN 0007-1161. PMID 24939424. S2CID 206873221.
- ↑ Ivanišević, Milan; Ivanišević, Petar; Lešin, Mladen (2018-10-29). "Epidemiological characteristics of orbital cellulitis among adult population in the Split region, Croatia". Wiener Klinische Wochenschrift. 131 (9–10): 205–208. doi:10.1007/s00508-018-1402-4. ISSN 0043-5325. PMID 30374774. S2CID 53102990.
External links
| Classification | |
|---|---|
| External resources |