Blepharitis
| Blepharitis | |
|---|---|
 | |
| Scaling and debris at the margin of the eyelid | |
| Pronunciation |
|
| Specialty | Ophthalmology |
| Symptoms | Red, itchy, and crusty eyelids[1] |
| Complications | Corneal ulcers[2] |
| Duration | Usually long term[1] |
| Types | Anterior, posterior[1] |
| Risk factors | Dandruff, rosacea, oily skin, allergies[1] |
| Diagnostic method | Eye exam[1] |
| Differential diagnosis | Stye, chalazion, dry eye[1] |
| Treatment | Regular cleaning of the eyelids[1] |
| Medication | Antibiotic or steroid eye drops[1] |
| Prognosis | Generally good[2] |
| Frequency | Common (1% per year)[1][2] |
Blepharitis is an eye condition that results in inflammation of the eyelid margin.[2] Symptoms commonly include red, itchy, and crusty eyelids.[1] Other symptoms may include irritation of the eyes, swollen eyelids, and dry eyes.[1] Complications may include eyelashes that grow in the wrong direction and corneal ulcers.[1][2]
Risk factors include dandruff, rosacea, oily skin, and allergies.[1] While the underlying mechanism often involves an excessive growth of bacteria, it is not contagious.[1] There are two main types: anterior and posterior.[1] Diagnosis is by eye exam.[1]
Treatment is generally by regular cleaning of the eyelids.[1] This can be carried out using warm water and baby shampoo.[1] Occasionally antibiotic or steroid eye drops may be used.[1] While outcomes are usually good, the condition is often long term.[1]
Blepharitis is a common eye conditions.[1] About 1% of people are estimated to be affected a year.[2] It is more common in those over the age of 50.[2] Females are affected more often than males.[2] Of people seen by eye specialists in the United States about 40% had signs of blepharitis.[3]
Signs and symptoms
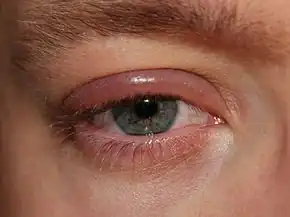
Blepharitis is characterized by chronic inflammation of the eyelid, usually at the base of the eyelashes.[4][5][6] Symptoms include inflammation, irritation, itchiness, a burning sensation, excessive tearing, and crusting and sticking of eyelids.[4][5] Additional symptoms may include visual impairment such as photophobia and blurred vision. Symptoms are generally worse in the mornings and patients may experience exacerbation and several remissions if left untreated.[3] It is typically caused by bacterial infection or blockage of the meibomian oil glands.[5] Diseases and conditions that may lead to blepharitis include: rosacea, herpes simplex dermatitis, varicella-zoster dermatitis, molluscum contagiosum, allergic dermatitis, contact dermatitis, seborrheic dermatitis, staphylococcal dermatitis, demodicosis (Demodex), and parasitic infections (e.g., Demodex and Phthiriasis palpebrarum).[3][4][6]
The parasite Demodex folliculorum (D. folliculorum) causes blepharitis when the parasite is present in excessive numbers within the dermis of the eyelids. These parasites can live for approximately 15 days. The parasites (both adult and eggs) live on the hair follicle, inhabiting the sebaceous and apocrine gland of the human lid. Direct contact allows this pathogen to spread. Factors that allow this pathogen to multiply include hypervascular tissue, poor hygienic conditions, and immune deficiency. In treating blepharitis caused by D. folliculorum, mechanical cleaning and proper hygiene are important towards decreasing the parasites numbers. [7]
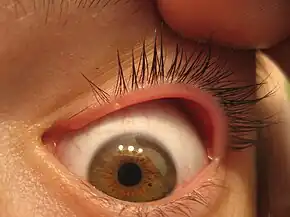
Symptoms include a foreign body sensation, matting of the lashes, and burning. Collarette, a ring-like formation around the lash shaft, can be observed.[8] Other symptoms include loss of eyelashes or broken eyelashes.[9] The condition can sometimes lead to a chalazion or a stye.[10] Chronic bacterial blepharitis may also lead to ectropion.[11] Posterior blepharitis or rosacea-associated blepharitis is manifested by a broad spectrum of symptoms involving the lids including inflammation and plugging of the meibomian orifices and production of abnormal secretion upon pressure over the glands.[12]
Associated symptoms
- Watery eyes - due to excessive tearing.[13]
- Red eyes - due to dilated blood vessels on the sclera.[13]
- Swollen eyelids - due to inflammation.[13]
- Crusting at the eyelid margins/base of the eyelashes/medial canthus, generally worse on waking - due to excessive bacterial buildup along the lid margins.[5][6][13]
- Eyelid sticking - due to crusting along the eyelid margin.[13]
- Eyelid itching - due to the irritation from inflammation and epidermis scaling of the eyelid.[13]
- Flaking of skin on eyelids - due to tear film suppressed by clogged meibomian glands.[13]
- Gritty/burning sensation in the eye, or foreign-body sensation - due to crusting from bacteria and clogged oil glands[13]
- Frequent blinking - due to impaired tear film from clogged oil glands unable to keep tears from evaporating.[13]
- Light sensitivity/photophobia[6][13]
- Misdirected eyelashes that grow abnormally - due to permanent damage to the eyelid margin[13]
- Eyelash loss - due to excessive buildup of bacteria along the base of the eyelashes.[13]
- Infection of the eyelash follicle/sebaceous gland (hordeolum)
- Debris in the tear film, seen under magnification (improved contrast with use of fluorescein drops)
Chronic blepharitis may result in damage of varying severity and, in the worst cases, may have a negative effect on vision. This can be resolved with a proper eyeglass prescription.[14] Long-term untreated blepharitis can lead to eyelid scarring, excess tearing, difficulty wearing contact lenses, development of a stye (an infection near the base of the eyelashes, resulting in a painful lump on the edge of the eyelid) or a chalazion (a blockage/bacteria infection in a small oil glands at the margin of the eyelid, just behind the eyelashes, leading to a red, swollen eyelid), chronic pink eye (conjunctivitis), keratitis, and corneal ulcer or irritation.[5][15][16] The lids may become red and may have ulcerate, non-healing areas that may lead to bleeding.[14] Blepharitis can also cause blurred vision due to a poor tear film.[5] Tears may be frothy or bubbly, which can contribute to mild scarring along the eyelids. Symptoms and signs of blepharitis are often erroneously ascribed by the patient as "recurrent conjunctivitis".[17]
Mechanism
The mechanism by which the bacteria causes symptoms of blepharitis is not fully understood and may include direct irritation of bacterial toxins and/or enhanced cell-mediated immunity to S. aureus.
Staphylococcal blepharitis Archived 2018-03-04 at the Wayback Machine is caused by an infection of the anterior portion of the eyelid by Staphylococcal bacteria. In a study of ocular flora, 46% to 51% of those diagnosed with staphylococcal blepharitis had cultures positive for Staphylococcus aureus in comparison to 8% of normal patients.[3] Staphylococcal blepharitis may start in childhood and continue into adulthood.[18] It is commonly recurrent and it requires special medical care. The prevalence of Staphylococcus aureus in the conjunctival sac and on the lid margin varies among countries, likely due to differences in climate and environment.[19] Seborrheic blepharitis Archived 2018-03-04 at the Wayback Machine is characterized by less inflammation than Staphylococcal blepharitis; however, it causes more excess oil or greasy scaling. Meibomian gland dysfunction is a result of abnormalities of the meibomian glands and altered secretion of meibum, which plays an imperative role in lagging the evaporation of tear films and smoothing of the tear film to produce an even optical surface. Posterior blepharitis is an inflammation of the eyelids, secondary to dysfunction of the meibomian glands. Like anterior blepharitis, it is a bilateral chronic condition and may be associated with skin rosacea.[12] There is growing evidence that, in some cases, it is caused by demodex mites.[20]
Diagnosis
Diagnosis of the condition is done via a physical examination under a slit lamp. Cultures of debris are occasionally collected for bacterial or fungal testing.[21][22]
Examination
In all forms of blepharitis, optometrists or ophthalmologists examine the tear film, which is the most efficient method in determining instability. The most frequently used method is to measure tear production via tear break-up time (TBUT), which calculates the duration interval between complete blinks. This serves as a primary indication of regional dryness in the pre-corneal tear film after fluorescein injections. If TBUT is shorter than 10 seconds, then this suggests instability.[3]
Staphylococcal blepharitis is diagnosed by examining erythema and edema of the eyelid margin. Patients may exhibit alopecia areata of eyelashes and/or growth misdirection, trichiasis. Other signs may include telangiectasia on the anterior eyelid, collarettes encircling the lash base, and corneal changes.[3] Seborrheic blepharitis is distinguished by less erythema, edema, and telangiectasia of the eyelid margins. Posterior blepharitis and Meibomian gland dysfunction are frequently associated with rosacea and can be seen during an ocular examination of the posterior eyelid margin. The Meibomian glands may appear caked with oil or visibly obstructed.[3]
Procedures
Cultures of the eyelid margins can be a clear indicator for patients suffering from recurrent anterior blepharitis with severe inflammation, in addition to patients who are not responding to therapy.[3] Measurements of tear osmolarity may be beneficial in diagnosing concurrent dry eye syndrome (DES), which may be responsible for overlapping symptoms and would allow the physician to decipher between conditions and move forward with the most beneficial protocol for the patient. Consequently, the measurement of tear osmolarity has various limitations in differentiating between aqueous deficiencies and evaporative dry eye.[23] Microscopic evaluation of epilated eyelashes may reveal mites, which have been evident in cases of chronic blepharoconjunctivitis. A biopsy of the eyelid can also determine the exclusion of carcinoma, therapy resistance, or unifocal recurrent chalazia.[24]
Differential diagnosis
| Condition | Entity |
|---|---|
| Bacterial infections | Erysipelas (due to Streptococcus pyogenes)
Impetigo (due to Staphylococcus aureus) |
| Viral infections | Herpes simplex virus |
| Parasitic infection | Pediculosis palperbrarum |
| Immunologic conditions | Atopic dermatitis |
| Dermatoses | Psoriasis |
| Benign eyelid tumors | Actinic keratosis |
| Malignant eyelid tumors | Melanoma |
| Trauma | Chemical
Radiation Thermal |
| Toxic conditions | Medicamentosa |
Prevention
Blepharitis is a result of bacteria and inflammation from congested meibomian oil glands at the base of each eyelash. Routine washing of the eyelids helps subdue symptoms and prevent blepharitis. Washing each eyelid for 30 seconds, twice a day, with a single drop of hypoallergenic soap (e.g. baby shampoo) and ample water can help. The most effective treatment is over the counter lid scrubs used twice a day. Some doctors may recommend using a hypochlorous acid treatment depending on the severity.[3]
Treatment
Blepharitis is a chronic condition causing frequent exacerbation, thus requiring routine eyelid hygiene. Hygienic practices include warm compresses, eyelid massages, and eyelid scrubs.[3] A Cochrane Systematic Review found topical antibiotics to be effective in providing help symptomatic relief and clearing bacteria for individuals with anterior blepharitis.[25] Topical steroids provided some symptomatic relief, but they were ineffective in clearing bacteria from the eyelids.[25] Lid hygiene measures such as warm compresses and lid scrubs were found to be effective in providing symptomatic relief for participants with anterior and posterior blepharitis.[25]
Ophthalmologists or optometrists may prescribe a low-dose, oral antibiotic such as Doxycycline.[12][26] A review of treatments showed that the anti-mite drug ivermectin can be an effective treatment for reducing symptoms.[27]
Eye drops or ointments containing corticosteroids are frequently used in conjunction with antibiotics and can reduce eyelid inflammation.[5][16][28]
Prognosis
Blepharitis is a chronic condition that has periods of exacerbation and remission. Patients should be informed that symptoms can frequently improve but are rarely eliminated. Infrequently, severe blepharitis can result in permanent alterations in the eyelid margin or vision loss from superficial keratopathy, corneal neovascularization, and ulceration. Patients with an inflammatory eyelid lesion that appears suspicious of malignancy should be referred to an appropriate specialist.[3][29]
Research
A study conducted in November 2017 detected a correlation between blepharitis and early-onset metabolic syndrome (MetS). To investigate the relationship between blepharitis and MetS, researchers used the Longitudinal Health Insurance Database in Taiwan. Results indicated that hyperlipidaemia and coronary artery disease were significantly correlated with the prior development of blepharitis. Therefore, blepharitis was shown to be significantly related to MetS and can serve as an early indication of the condition.[30]
In another study, the presence of Demodex mites was shown to be a common cause of blepharitis. However, the pathogenesis of demodicosis is still unclear. In this study, researchers provided a diagnosis of the disease and proposed diagnostic criteria for Demodex blepharitis.[31]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 "Blepharitis | National Eye Institute". www.nei.nih.gov. Archived from the original on 23 December 2021. Retrieved 10 February 2022.
- 1 2 3 4 5 6 7 8 Eberhardt, Mary; Rammohan, Guhan (2022). "Blepharitis". StatPearls. StatPearls Publishing. Archived from the original on 10 February 2022. Retrieved 10 February 2022.
- 1 2 3 4 5 6 7 8 9 10 11 Singh Tonk R, Hossain K (November 27, 2014). "Blepharitis". Archived from the original on February 3, 2022. Retrieved February 8, 2022.
- 1 2 3 "Blepharitis Definition - Diseases and Conditions - Mayo Clinic". Archived from the original on 2017-10-01. Retrieved 2022-02-08.
- 1 2 3 4 5 6 7 "Blepharitis: Symptoms, Treatment, and Prevention". Archived from the original on 2022-01-29. Retrieved 2022-02-08.
- 1 2 3 4 "Medscape: Medscape Access". Archived from the original on 2021-07-11. Retrieved 2022-02-08.
- ↑ Inceboz T, Yaman A, Over L, Ozturk AT, Akisu C (2009). "Diagnosis and treatment of demodectic blepharitis". Turkiye Parazitolojii Dergisi. 33 (1): 32–6. PMID 19367544.
- ↑ R Scott Lowery (Jun 17, 2011). "Adult Blepharitis". Medscape. Archived from the original on 12 January 2013. Retrieved 21 December 2012.
- ↑ James Garrity (August 2012). "Blepharitis". The Merck Manual. Archived from the original on 6 June 2012. Retrieved 21 December 2012.
- ↑ "Blepharitis, Stye and Chalazion". University of Illinois College of Medicine. Archived from the original on 19 April 2014. Retrieved 21 December 2012.
- ↑ "How to Get Rid of Sore, Red Eyelids (Blepharitis)". Archived from the original on 2021-11-30. Retrieved 2022-02-08.
- 1 2 3 Emmett T. Cunningham; Paul Riordan-Eva (2011-05-17). Vaughan & Asbury's general ophthalmology (18th ed.). McGraw-Hill Medical. ISBN 978-0071634205.
- 1 2 3 4 5 6 7 8 9 10 11 12 "Blepharitis Symptoms - Diseases and Conditions - Mayo Clinic". Archived from the original on 2017-09-22. Retrieved 2022-02-08.
- 1 2 Frank J. Weinstock. "Eyelid Inflammation Symptoms". emedicinehealth.com. Archived from the original on 18 October 2012. Retrieved 21 December 2012.
- ↑ "Blepharitis Complications - Diseases and Conditions - Mayo Clinic". Archived from the original on 2017-09-10. Retrieved 2022-02-08.
- 1 2 "Medscape: Medscape Access". Archived from the original on 2021-04-20. Retrieved 2022-02-08.
- ↑ Dahl, Andrew. "What are the symptoms and signs of blepharitis?". medicinenet.com. Archived from the original on 2 January 2013. Retrieved 21 December 2012.
- ↑ "Blepharitis". Angeles Vision Clinic. Archived from the original on 4 May 2012. Retrieved 21 December 2012.
- ↑ Smolin G, Okumoto M (1977). "Staphylococcal blepharitis". Archives of Ophthalmology. 95 (5): 812–816. doi:10.1001/archopht.1977.04450050090009. PMID 324453.
- ↑ Liu J, Sheha H, Tseng SCG (October 2010). "Pathogenic Role of Demodex Mites in Blepharitis". Curr Opin Allergy Clin Immunol. 10 (5): 505–510. doi:10.1097/aci.0b013e32833df9f4. PMC 2946818. PMID 20689407.
- ↑ "Blepharitis Tests and diagnosis - Diseases and Conditions - Mayo Clinic". Archived from the original on 2017-09-06. Retrieved 2022-02-08.
- ↑ "Medscape: Medscape Access". Archived from the original on 2021-05-17. Retrieved 2022-02-08.
- ↑ Savini G, Prabhawasat P, Kojima T, Grueterich M, Espana E, Goto E (March 2008). "The challenge of dry eye diagnosis". Clinical Ophthalmology (Auckland, N.Z.). 2 (1): 31–55. doi:10.2147/opth.s1496. PMC 2698717. PMID 19668387.
- ↑ Yuji Nemoto, Atsushi Mizota, Reiko Arita, Yuko Sasajima (September 2014). "Differentiation between chalazion and sebaceous carcinoma by noninvasive meibography". Clinical Ophthalmology. 8: 1869–1875. doi:10.2147/OPTH.S69804. PMC 4172083. PMID 25258508.
- 1 2 3 Lindsey K, Matsumara S, Hatel E, Akpek EK (2012). "Interventions for chronic blepharitis". Cochrane Database Syst Rev. 5 (5): CD00556. doi:10.1002/14651858.CD005556.pub2. PMC 4270370. PMID 22592706.
- ↑ Liu J, Sheha H, Tsenga CG (2010). "Pathogenic role of Demodex mites in blepharitis". Curr Opin Allergy Clin Immunol. 10 (5): 505–510. doi:10.1097/ACI.0b013e32833df9f4. PMC 2946818. PMID 20689407.
- ↑ Navel V, Mulliez A, Benoist d'Azy C, Baker JS, Malecaze J, Chiambaretta F, Dutheil F (October 2019). "Efficacy of treatments for Demodex blepharitis: A systematic review and meta-analysis". The Ocular Surface. 17 (4): 655–669. doi:10.1016/j.jtos.2019.06.004. PMID 31229586.
- ↑ "Blepharitis Treatments and drugs - Diseases and Conditions - Mayo Clinic". Archived from the original on 2017-09-22. Retrieved 2022-02-08.
- ↑ Dahl, Andrew A. "Blepharitis". MedicineNet. Archived from the original on 2017-08-10. Retrieved 2022-02-08.
- ↑ Lee CY, Chen HC, Lin HW, Huang JY, Chao SC, Yeh CB, Lin HY, Yang SF (November 2017). "Blepharitis as an early sign of metabolic syndrome: a nationwide population-based study". The British Journal of Ophthalmology. 102 (9): 1283–1287. doi:10.1136/bjophthalmol-2017-310975. PMID 29146760. S2CID 26261977.
- ↑ Liang LY, Liu Y, Li J (September 11, 2017). "Diagnostic criteria of demodex blepharitis". [Zhonghua Yan Ke Za Zhi] Chinese Journal of Ophthalmology. 53 (9): 648–652. doi:10.3760/cma.j.issn.0412-4081.2017.09.003. PMID 28926882.
External links
| Classification | |
|---|---|
| External resources |